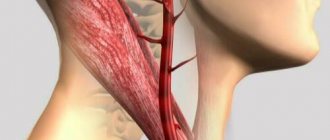
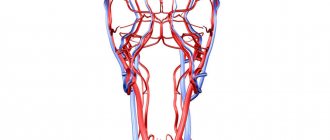
Carotid artery stenosis is a condition in which there is narrowing (stenosis) or complete closure (occlusion) of the carotid artery. A person has two carotid arteries located in the neck (right and left). These blood vessels carry blood to the brain and face.
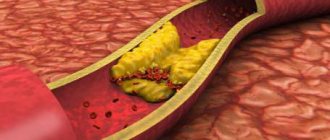
The most common cause of narrowing or occlusion of the carotid artery is the deposition of atherosclerotic plaques on the inner walls of the vessel. The plaque is made up of scar tissue, blood cells, cholesterol and other fatty substances. Enlarged plaque narrows the artery and slows blood flow.
Blood clots (thrombi) can form on the plaques, further obstructing blood flow. Parts of a blood clot or atherosclerotic plaque can break off and travel through the bloodstream into the arteries of the brain.
As a result, a so-called cerebral embolism occurs, leading to the development of ischemic stroke.
Occlusion of the carotid artery can lead to stroke or sudden rapid death.
The risk to life increases if there is damage to the carotid arteries on both sides. The most common cause of narrowing or occlusion of the carotid artery is the deposition of atherosclerotic plaques on the inner walls of the vessel.
The plaque is made up of scar tissue, blood cells, cholesterol and other fatty substances. Enlarged plaque narrows the artery and slows blood flow. Blood clots (thrombi) can form on the plaques, further obstructing blood flow.
Parts of a blood clot or atherosclerotic plaque can break off and travel through the bloodstream into the arteries of the brain. As a result, a so-called cerebral embolism occurs, leading to the development of ischemic stroke.
Occlusion of the carotid artery can lead to stroke or sudden rapid death.
The risk to life increases if there is damage to the carotid arteries on both sides.
The most common cause of narrowing or occlusion of the carotid artery is the deposition of atherosclerotic plaques on the inner walls of the vessel.
The plaque is made up of scar tissue, blood cells, cholesterol and other fatty substances. Enlarged plaque narrows the artery and slows blood flow.
Blood clots (thrombi) can form on the plaques, further obstructing blood flow.
Parts of a blood clot or atherosclerotic plaque can break off and travel through the bloodstream into the arteries of the brain. As a result, a so-called cerebral embolism occurs, leading to the development of ischemic stroke.
Occlusion of the carotid artery can lead to stroke or sudden rapid death. The risk to life increases if there is damage to the carotid arteries on both sides.
Symptoms of carotid artery stenosis
Most people with carotid artery lesions have no symptoms. If symptoms are present, the risk of ischemic stroke increases several times.
The most common symptoms are transient (i.e., intermittent) ischemic attacks, which are sometimes called minor strokes.
During an ischemic attack, blood supply to certain areas of the brain is reduced. This may cause temporary dizziness, blurred vision, numbness and tingling of the skin of the extremities, and weakness in an arm or leg, which usually lasts no more than 30 minutes.
The risk of stroke is very high in people who have had a transient ischemic attack.
A stroke occurs when there is a sharp decrease in blood supply to a vessel supplying the brain or when it is occluded. Depending on the area of the brain affected, a stroke manifests itself as paralysis of an arm and/or leg, visual and speech disturbances, and behavioral changes.
The larger the area of the brain affected, the greater the risk to life.
Risk factors for stroke:
- Atherosclerosis
- Diabetes
- High blood pressure
- Smoking
- Eating fatty foods
- Excess weight
- Increased thrombus formation
Symptoms
The main role among developing disorders belongs to ischemia of tissues that are supplied with blood from the subclavian vessel.
Symptoms of the first stage of blood supply failure:
- increased sensitivity to cold;
- a feeling of chilliness and numbness appears;
- paresthesia;
- are formed by vasomotor reactions.
Symptoms of the second stage of blood supply failure:
- weakness;
- pain appears;
- numbness;
- the hands, fingers and forearm muscles become cold.
Symptoms of the third stage of blood supply failure:
- constant coldness and numbness of the hands;
- muscle wasting;
- decreased muscle strength;
- inability to perform subtle and precise movements with the fingers.
Symptoms of the fourth stage of blood supply failure:
- cyanosis and swelling of the phalanges;
- cracks and trophic ulcers develop, which turn into necrosis and gangrene of the phalanges.
- Thrombosis and cerebral ischemia contribute to the rapid development of the disease. The result may be acute ischemic stroke.
Symptoms of closure of the lumen of the first segment:
- dizziness, frequent headaches;
- vestibular ataxia and hearing loss;
- visual disturbances;
- ischemia of the upper extremities;
- coronary-mammary-subclavian steal syndrome.
Symptoms that are characteristic of any type of pathology:
- loss of consciousness;
- paresis;
- swallowing and speech disorders;
Diagnosis of carotid artery stenosis
To determine whether you have stenotic lesions of the carotid arteries or not, your doctor will examine you.
Even if you have no symptoms, your doctor may hear a murmur over your carotid arteries caused by blood flowing through the stenotic area.
If necessary, you will be prescribed Doppler ultrasound of the main arteries of the head (USDG MAG), electroencephalography of the brain (EEG) or computed tomography (CT).
For a more detailed assessment of the condition of the carotid arteries, your doctor may recommend an angiography (x-ray examination of blood vessels).
This study is performed by catheterization, usually of the femoral artery, under local anesthesia in a special operating room equipped with an angiography unit.
After the examination, the doctor will determine the presence of a lesion and choose the optimal treatment method for you.
Diagnostics
To begin with, a physical examination is performed. To do this, you need to make an appointment with a cardiologist. In case of visual impairment, consultation with an ophthalmologist is necessary. To confirm the diagnosis, the doctor prescribes the following:
- Doppler ultrasound;
- duplex scanning of all vessels of the upper limb;
- peripheral arteriography;
- X-ray contrast angiography;
- rheovasography;
- thermography;
- sphygmography;
- magnetic resonance angiography;
- peripheral CT arteriography;
- MSCT angiography.
Angiography of the carotid arteries
During this test, a very thin catheter is inserted into an artery in your leg and advanced toward your neck. A contrast agent is then injected through the catheter, making the carotid arteries and other arteries in the neck visible under X-rays.
On the eve of the examination, you should shave the skin in the groin area. You should also abstain from food and liquids (except medications) in the evening. In the operating room, you will be covered with sterile sheets, which you cannot touch so as not to compromise sterility.
During the test, your doctor will monitor your electrocardiogram (ECG) and blood pressure (BP). The catheter insertion site will be treated with an antiseptic and numbed.
After this, the doctor will puncture your artery, through which he will pass a catheter to your neck. You won't feel it, but you will be able to see the catheter on the monitor.
You must follow all doctor's instructions. Sometimes you will need to hold your breath and not move. From time to time, from the administration of a contrast agent, you may feel warmth or a rush of heat in your head. The doctor will take pictures of the artery. If you have stenosis or occlusion of the carotid arteries, they will be detected.
Depending on the results obtained, you may be recommended a treatment procedure or scheduled for re-examination at a later date.
Treatment of vertebral artery syndrome
Questions and answers
Possibly gongrene I injured my hand, the skin was torn off while drinking on gravel and my hand became rusty in two hours, what should I do?
Answer:
See a surgeon for an appointment.
Hypoplasia of the left vertebral artery
Hello. I have been sick for a long time. Nausea. vomiting. Impaired coordination. unsteadiness. Severe headaches. What examination should I do before someone turns to you for help?
Answer:
Do MSCT of the arteries of the neck and brain with contrast.
Thromboangiitis obliterans
Hello. My mother is 58 years old, disabled group 1. She had both legs amputated below the knees due to thromboangiitis obliterans. We underwent an ultrasound examination of the NK vessels. What additional research needs to be done...
Answer:
What about the stumps now?
Leg amputated
Hello! My brother had his leg amputated in December 2021 due to atherosclerosis, after which he developed gangrene. In January we underwent re-amputation. It is now March, but the wound is not healing. They did a CT scan of the vessels...
Answer:
What to do?
Restore blood flow. Send a link to MSCT of vessels. Gangrene
Hello, my dad had gangrene on his right leg on the big toe, his toe was amputated, the treatment prescribed by the doctor did not help, there was pain, a large crust and there was pus, they applied ointments...
Answer:
It is urgent to perform an ultrasound of the arteries of the extremities and MS CT with contraception; after receiving the examination results, we will be able to offer you the optimal treatment method.
How to treat trophic ulcers and necrosis of the fingers.
Hello. After examination at the Donetsk Institute of Emergency and Reconstructive Surgery named after. In K. Gusak (DPR), my husband was diagnosed with ischemic heart disease: atherosclerotic cardiosclerosis. CH2a. GB 2st. risk 3. Left ventricular thrombus. ...
Answer:
Good afternoon.
The left leg suffers from ischemia, i.e. lack of blood flow. To prevent it from bothering you, you need to restore blood flow. Need surgery. Perform CT angiography of the abdominal aorta and arteries of the lower extremities (to the feet)…. Red spots.
Hello, I broke my leg in September, but after 4 months, red spots in the form of bruises appeared on my leg, and they just don’t go away. WHAT COULD BE?
Answer:
Good afternoon.
Without examination it is not possible to make a diagnosis. See a traumatologist. Wet gangrene
Hello! My dad (70 years old) has wet gangrene of the leg, we live together in the same apartment with a small child (2 years old), is this situation dangerous for the baby? Thank you!
Answer:
Good afternoon.
Gangrene is dangerous if it is accompanied by an infection. Show the patient to the surgeon. Atherosclerosis of the lower extremities.
Hello, my dad is sick, he is 81 years old. atherosclerosis, calcification of blood vessels of the lower extremities. In Perm, doctors did everything they could (including angioplasty, which did not bring results). For now…
Answer:
Most likely it is possible, but you need to see the patient in person.
You cannot establish a forecast by correspondence. Occlusion of the upper limb.
My mother is 68 years old. Since August 2021, for the first time, very severe pain appeared in the elbow on the right. Gradually, the pain intensified and spread lower throughout the arm; conservative treatment had no effect. Consulted by a neurosurgeon from the Federal Center of Neurology of...
Answer:
Perform CT angiography of the arteries of the upper extremities. Send a link to the study by mail
Non-invasive methods for visualizing brachiocephalic vessels. Ultrasound examination (ultrasound)
Vascular duplex scanning is usually the first method used in most clinics in Krasnoyarsk, providing useful information about anatomy and hemodynamics. In fact, subclavian steal phenomenon is often diagnosed incidentally during ultrasound imaging of the carotid and vertebral arteries. However, this technique can be difficult due to the overlying bony structures (clavicle, ribs and sternum). Duplex scanning has signs indicating the phenomenon of blood flow stealing, which will consist of a decrease in the flow rate in the vertebral artery. This decrease will be related to the degree of steal as long as the direction is initially antegrade, whereas as the disease progresses it will reverse. Reversed blood flow in the left vertebral artery will be combined with normal flow cephalad in the contralateral vertebral artery. However, it should be remembered that even a continuous, total change in flow in the vertebral artery does not indicate the presence of neurological symptoms.
Reversal of blood flow in the vertebral artery can be obtained by visualizing this vessel during reactive hyperemia caused by exercise of the arm. The presence of stenosis of the proximal subclavian artery or its occlusion can be inferred from changes in the spectral signal detected in the distal subclavian, axillary or brachial arteries, as a rule, on duplex scanning there is a loss of the usual triphasic pattern. Likewise, compensatory increased flow may be evident in the remaining extracranial arteries in the presence of subclavian steal syndrome. Despite severe stenosis of the proximal left subclavian artery, reversal of blood flow in the ipsilateral vertebral artery may be absent in 6% of patients when the left vertebral artery arises directly from the aorta. This anatomical variant can be difficult to study directly on duplex scanning due to the prominent bony structures, but is clearly visible during angiography.
Magnetic resonance imaging (MRI)
MRI is a rapidly evolving technique, and its clinical use is expanding in most cases. MR angiography uses the principle of enhancement flow, where two-dimensional or three-dimensional images can be obtained. In particular, MRA is often used as a rapid method of imaging the cervical carotid and vertebral arteries. While it is generally reliable in demonstrating anatomy and vascular patency, it may overestimate the degree of arterial constriction and is less reliable than ultrasound in tortuous vessels, especially in the presence of turbulent flow.
Contrast-enhanced arterial tree imaging is less susceptible to artifacts due to complex anatomy and flow patterns and can cope with more complex anatomical regions. MRA, however, remains a technique that some patients cannot tolerate (claustrophobia) or cannot undergo due to concomitant pathology (pacemakers, cerebral aneurysm clips, etc.).
Computed tomography (CT)
CT angiography allows us to determine the anatomy of the vessels of the aortic arch along with the complex anatomical features of the soft tissues and adjacent bone structures. Vessel identification has improved significantly with the advent of multislice CT, as fast image processing provides high concentrations of contrast agent. At the same time, software developments make it possible to obtain images in three-dimensional reconstruction, which can provide information about the extent and localization of obliterating atherosclerosis. CT angiography, however, involves exposure to ionizing radiation and, unlike conventional angiography, does not allow vascular intervention.