Hypertension (essential or primary hypertension) is a chronic disease associated with a long-term and persistent increase in blood pressure (BP).
There are two forms of hypertension (hypertension): primary and secondary. Approximately 90-95% of patients with hypertension have the primary form. Unlike secondary hypertension, primary hypertension does not have a clearly defined known cause. Therefore, its diagnosis is made after ruling out known causes, which include what is called secondary hypertension. For example, blood pressure may increase symptomatically with kidney disease, and so on.
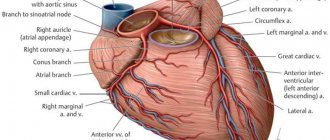
Blood pressure: Blood pressure resulting from the work of the heart, which pumps blood into the vascular system, and vascular resistance.
Blood pressure readings are usually given as two numbers: for example, 120 over 80 (written as 120/80 mmHg).
The top number is called systolic blood pressure (the higher pressure and the first number recorded) - this is the pressure that blood puts on the walls of the artery when the heart contracts to pump it to peripheral organs and tissues. The bottom number is diastolic blood pressure (the lower pressure and the second number recorded) - this is the residual pressure exerted on the arteries when the heart relaxes between beats.
Normal blood pressure is a relative value, which depends on age, physical activity, psychological state, and even on the use of various medications.
Hypertension occurs when the body's smaller blood vessels (arterioles) narrow, causing the blood to put undue pressure on the vessel walls and causing the heart to work harder to maintain the pressure. In this case, blood pressure reaches or exceeds 140/90 mm Hg.
Diastolic blood pressure is more common in people under 50 years of age. As we age, systolic hypertension becomes a more serious problem. At least a quarter of the adult population (and more than half of those over 60) have high blood pressure.
Causes and risk factors
Despite many years of active research, there is no unifying hypothesis to account for the pathogenesis (mechanism of occurrence) of hypertension. In chronic long-standing hypertension, blood volume and cardiac output are often normal, so hypertension is maintained by increased systemic vascular resistance rather than increased cardiac output. There is also evidence of increased vascular tone. In addition, disturbances in the nervous and endocrine regulation of blood pressure play a role in the development of the disease.
Many factors can affect blood pressure, including:
- Genetic, which play an important role in the occurrence of hypertension.
- How much water and salt is in your body.
- The condition of your kidneys, nervous system and blood vessels.
- Levels of various body hormones.
- Age. Blood pressure gets higher as you get older. This is because blood vessels become stiffer as a person ages.
You are at increased risk of hypertension if you:
- Are you obese?
- Frequently experience stress or anxiety;
- Drinking too much alcohol;
- Consume too much salt;
- Have a family history of the disease:
- Diabetic;
- Smoke;
- You lead a sedentary lifestyle;
- You are experiencing stress.
Characteristic symptoms of hypertension
Signs of arterial hypertension are:
- tinnitus due to a rush of blood to the head;
- headaches, dizziness;
- cardiopalmus;
- swelling;
- a state of chills accompanied by profuse sweating;
- pulsation disorder;
- attacks of anxiety and irritability;
- feeling tired and lack of sleep;
- swelling and numbness of the fingers and toes.
Symptoms of hypertension are periodic and resolve with rest. In the absence of timely medical care, the list of signs of the disease is supplemented by:
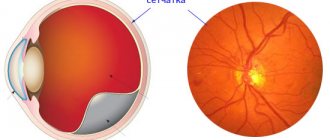
- drop in visual acuity;
- deterioration of memory and quality of mental activity;
- disruptions in the functioning of blood vessels and kidneys
- weakness in arms and legs;
- gait changes;
- decreased sensitivity.
Are you experiencing symptoms of hypertension?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Classification of hypertension
There is no single classification, but the one recommended by WHO is most often used. Hypertension, depending on the degree of increase in pressure, is divided into three stages:
Stage 1 hypertension. Soft or borderline stage. The pressure is 140/90 mm Hg. or higher.
Stage 2 hypertension. Moderate stage. The pressure is 160/100 mmHg. or higher.
Hypertension stage 3. Severe form of hypertension. Clinical systolic blood pressure is 180 mmHg. or higher, and diastolic is 110 mm Hg. or higher.
The disease is also divided into three stages, depending on the degree of development:
Stage 1: slight increase in blood pressure. There are no complaints, the functioning of the cardiovascular system is not impaired.
Stage 2: constant increase in blood pressure and associated enlargement of the left ventricle of the heart.
Stage 3: increased blood pressure affects the functioning of the heart, brain and kidneys.
Methods for diagnosing hypertension
The basis of diagnosis is monitoring the patient at home after exercise and in a state of physical rest using pressure gauges. In addition, the following results allow us to talk about arterial hypertension:
- recording risk factors;
- 24-hour blood pressure monitoring;
- electrocardiograms;
- conclusions of a nephrologist, endocrinologist and neurologist;
- blood and urine tests;
- Ultrasound of the kidneys and heart;
- chest radiographs.
Course of hypertension
The risk associated with increased blood pressure is continuous, with each 2-3 mmHg increase in systolic blood pressure. Art.
Hypertension increases the risk of mortality from coronary heart disease by 7% and the risk of mortality from stroke by 10%. The most common immediate cause of death associated with hypertension is heart disease, but death from kidney failure is also common.
Complications arise directly from increased blood pressure (cerebral hemorrhage, retinopathy, left ventricular hypertrophy, congestive heart failure, arterial aneurysm and vascular rupture), from atherosclerosis (increased coronary, cerebral and renal vascular resistance), as well as from decreased blood flow and ischemia ( myocardial infarction, cerebral thrombosis, infarction and renal nephrosclerosis).
If your blood pressure is not well controlled, you are at risk of:
- Bleeding from the aorta, the largest blood vessel,
- Chronic kidney disease,
- Heart attack or heart failure,
- Poor blood supply to the legs,
- Vision problems
- Stroke,
- Disturbance of cerebral blood supply.
FAQ
Do they take you into the army with hypertension?
A decision on this issue will be made at the medical examination of conscripts. But you need to notify the doctors conducting the examination about your illness and have a document with you confirming the diagnosis. If the disease progresses, complete or temporary medical withdrawal or alternative service is possible.
How do I know if I have hypertension?
The main symptom of the disease is an increase and persistence of high blood pressure with a simultaneous sharp deterioration in health, headaches, nausea, rapid heartbeat, etc. Even a rare repetition of such cases should be a reason to consult a doctor. The final diagnosis can be made only after a full examination of the patient.
Treatment of hypertension at the Innovative Vascular Center
Our clinics employ experienced cardiologists who can accurately determine the causes of high blood pressure and prescribe therapy appropriate to the causes and stage of the disease.
In case of hypertension, we always conduct a thorough diagnostic search, identifying all possible causes of secondary hypertension, especially those related to vascular damage (vasorenal hypertension, increased blood pressure due to narrowing of the carotid arteries, in the presence of adrenal tumors).
At the Innovative Vascular Center, it is possible to correct the causes of arterial hypertension using endovascular methods (stenting of the renal arteries, radiofrequency denervation of the renal arteries).
Is it possible to cure hypertension without giving up the joys of life?
Why do the measures that doctors usually recommend so rarely help? Because doctors' advice is often too difficult to implement in real life. Doctors recommend that patients voluntarily give up most of the joys of their lives. Naturally, patients are in no hurry to do this.
| Traditional recommendation for patients with hypertension | Why is it difficult to do? |
| Reduce stress levels at work and at home | To do this, you need to retrain or accept a decrease in income |
| Avoid fatty and salty foods and limit caloric intake | You'll have to go hungry all the time |
| Exercise outdoors | If after work there is also physical education, then when will we live? |
It is also good if a hypertensive patient swallows the pills prescribed to him in a disciplined manner every day. At best, they will delay the onset of target organ damage for several years. But, as a rule, you still don’t have to wait too long for a heart attack or stroke. Please note that this is actually beneficial for the state, because the number of pensioners is reduced, as well as the period during which they have to pay their pensions. What to do? Is there really no effective way to get your blood pressure under control and prolong your life? It turns out there is. Moreover, this wonderful method does not bring suffering to patients, quite the contrary. So, we have established and tested on dozens of patients that the best method of treating hypertension is limiting carbohydrates in the diet. A low-carbohydrate diet helps almost 100% of patients with hypertension, in whom this disease is combined with obesity or type 2 diabetes.
Cure from hypertension in 3 weeks - it's real! Read here:
- The best way to cure hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Do you have hypertension + insomnia + irritability? This is a deficiency of magnesium in the body!
- Hypertension, its causes and how you can eliminate them
It turns out that you can eat your fill of meat, fish, fatty poultry, eggs, butter, etc. - and have normal blood pressure of about 120-130/80, as well as excellent blood cholesterol levels. Many patients don't believe this is possible at first because it seems "too good." However, it is true. In a few weeks, you will see for yourself that you can eat tasty and satisfying meals, and at the same time your blood pressure will normalize. Take blood tests for cholesterol and you will see that your levels are also improving. This means that the “new life” can be safely continued. Since on a low-carb diet you will feel full and satisfied all the time, there will be no reason to “break down” and return to your old diet.
Low-carbohydrate diets (Dukan, “Kremlin” and Atkins) are triumphantly marching across the country, despite the desperate resistance of “official” medicine. They bring the most benefit to people suffering from:
- obese
- type 2 diabetes
- epilepsy.
- ...and at the same time they quickly normalize blood pressure.
Why are doctors so resistant to promoting these diets? Because they promise millions of dollars in losses for drug manufacturers, and many doctors will soon be left without work. But for patients, this is an excellent opportunity to prolong their lives and be free from serious illnesses. Attention! This method is not suitable if you have “secondary” hypertension caused by some other “primary” disease. For example, progressive renal failure or adrenal tumor. In such cases, hypertension does not respond to conventional treatment. It will go away only when the doctor identifies and treats the primary disease. This applies to no more than 5-10% of patients from their total number. If you already have kidney failure, liver problems or serious diseases of the gastrointestinal tract, use only in consultation with your doctor and under his close supervision. Limiting carbohydrates in the diet is not recommended for pregnant women.
Surgical intervention
For many people, the answer to the question “how to get rid of hypertension forever” is surgery. But even with high-quality and timely intervention, it is necessary to maintain a healthy lifestyle, otherwise everything will quickly return to its place. Surgery is often used in severe cases of blockage of blood vessels, in which there is no effect of drug treatment.
In surgery, the 2 most common methods of intervention are used:
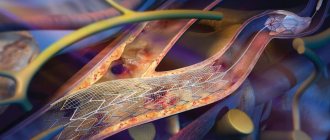
- Percutaneous angioplasty. The essence of this operation is to insert a catheter with a balloon into the vessel to improve its conductivity. The procedure is contraindicated for people whose artery passage is too narrow or if it is completely blocked. In rare cases, a vessel may rupture during catheter insertion.
- Open surgery. Unlike percutaneous angioplasty, this type of surgery is more traumatic. The patient will have to spend a lot of time under anesthesia and the recovery period will be much longer. The essence of the open operation is to remove the plaque that appears along with a piece of the vessel. An artificial or your own transplanted vessel will take its place. Thanks to this procedure, it is possible to effectively treat hypertension, since it will be possible to restore damaged arteries. This is especially true for extensive atherosclerosis.
Arterial hypertension – lifelong medication use?
Perhaps the majority of patients seen by a cardiologist are patients with high blood pressure - arterial hypertension (AH). Some of them had their blood pressure rise for the first time due to a stressful situation, some have been taking medications for a long time, but, as a rule, few have a complete understanding of their disease, and most importantly, how to live with it correctly and effectively treat it .
In a healthy person, blood pressure changes throughout the day depending on the level of stress (physical, mental, etc.), but in general these fluctuations do not exceed the so-called physiological norm, which supports the normal functioning of the body. For an adult, blood pressure is considered normal no higher than 140/90 mmHg. Art. And in some cases, for example, in the presence of diabetes mellitus, kidney disease, the pressure should be even lower at the level of 130/80 - 120/70 mm Hg. Art., which helps prevent the progression of these diseases and the development of complications. The state of the nervous system, heart and blood vessels plays an important role in maintaining blood pressure within optimal limits. With hypertension, the heart works overload, pumping an additional volume of blood. Over time, this leads to increased resistance from the vessels, which narrow under conditions of constant overload. The walls of the arteries thicken and harden, losing their elasticity. With the long-term existence of hypertension, the load on the vessels becomes unbearable, which can lead to degenerative changes in their wall, with the development of narrowing or pathological expansion, and even rupture of the vessel can occur. If this complication occurs in a vital organ (heart, brain), then it can result in myocardial infarction or cerebral hemorrhage (stroke) . But, despite this danger, the insidiousness of hypertension is that it can be completely asymptomatic for a long time.
The diagnosis of hypertension is usually not made after a single blood pressure measurement, unless the readings are too high, for example, over 170-180/105-110 mm Hg. Art. Typically, a series of measurements are taken over a period of time to completely eliminate random fluctuations and inaccuracies. It is also necessary to take into account the circumstances during which blood pressure measurements are taken. As a rule, blood pressure increases under stress, after drinking strong coffee or smoking a cigarette.
About 1/3 of the adult population has a persistent increase in blood pressure above 140/90 millimeters of mercury. 2/3 of those who suffer from hypertension do not know about their disease, and those who know often do not give it due importance (especially if the numbers are not so high, about 160/100 mm Hg), until headaches, heart pain, shortness of breath, arrhythmia, and swelling will not occur.
An interesting fact is that in a doctor’s office, when measuring blood pressure, the readings can be higher than at rest at home. This effect is called "white coat hypertension" and is caused by the patient's fear of the disease or the doctor. In addition to measuring blood pressure, the doctor usually checks for changes in other organs, especially if the pressure readings are at high levels.
If the blood pressure in an adult does not exceed 140/90 mm. rt. Art., then re-measurement is usually carried out no earlier than a year later. In patients whose blood pressure is between 140/90 and 160/100, repeated measurements are taken after a short period of time to confirm the diagnosis.
A high diastolic (bottom) pressure, such as 110 or 115 mmHg, indicates the need for immediate treatment.
Hypertension is one of the most common diseases. In developed countries, 10% of the adult population and about 60% of people over 65 years of age have high blood pressure. Unfortunately, no more than 30% of these people know about their illness, regularly receive therapy and follow the doctor’s recommendations. Unlike a number of diseases that you can “get over,” hypertension, as a rule, is a chronic, lifelong condition.
Arterial hypertension is most often primary in nature and is a symptom of hypertension. Less commonly, high blood pressure is secondary and is a sign of diseases of various organs (kidneys, blood vessels, etc.). Each of these diseases requires special treatment, which is why any increase in blood pressure requires consultation with a cardiologist.
In older people, a special type of hypertension sometimes occurs, so-called “isolated systolic hypertension.” In this case, systolic pressure readings are equal to or exceeding 140 mmHg, and diastolic pressure readings remain below 90 mmHg. This type of hypertension is a dangerous risk factor for the development of strokes and heart failure. Often, patients seek help only when the diastolic pressure, in their opinion, becomes too low - 50-60 mm Hg. Art. Sometimes this can be a sign of heart disease, but more often it is associated with age-related changes in the vascular wall, and it is very important to find drugs that will reduce the gap between systolic and diastolic pressure numbers, which in turn reduces the risk of stroke and heart failure .
In cases where routine and dietary measures do not allow adequate control of blood pressure, additional (and not instead) medications are prescribed. Today their list is quite impressive. Often, when a patient seeks help with complaints of high blood pressure despite taking prescribed medications, you can see that the medications were chosen correctly and are suitable for the patient for long-term use, but their dosages are inadequate. In cardiology, there is the concept of an effective dose - that is, one at which one can count on the manifestation of the desired effect. And if you take the same drug in halves or fours, and not just 2, but once a day, and often not even every day, then there is no need to talk about any hypotensive, much less therapeutic, effect of the drug. When prescribing one or more drugs, the cardiologist takes into account the level of blood pressure, the severity of hypertension, the individual daily blood pressure profile, the main risk factors or causes of arterial hypertension, the severity of target organ damage, the presence of concomitant diseases, and the interaction of drugs with each other and with other medications taken. , the possibility of developing side effects. Therefore, it is absolutely unacceptable for a patient to change doctor’s prescriptions, drug doses, frequency of administration, or discontinue one or another drug on their own. If, when taking a prescribed combination of antihypertensive drugs, the patient notices the occurrence of any side effects, the pressure does not decrease or, on the contrary, decreases excessively, it is necessary to discuss this with the attending physician, who, having understood the reasons, will adjust your prescriptions.
The role of the patient in the treatment of arterial hypertension cannot be underestimated. The effectiveness of treatment measures largely depends on how ready he is, in accordance with the doctor’s recommendations, to actively and consistently fight and, if possible, eliminate his risk factors. Dealing with risk factors means stopping smoking, limiting alcohol consumption, regularly taking recommended medications and monitoring their effect on blood pressure by recording measurements in a special diary.
Effective control of blood pressure should be considered if, as a result of lifestyle modifications, elimination of risk factors and bad habits, or taking antihypertensive drugs, it is possible to maintain blood pressure levels below 140/90 mmHg. Art., and for patients with diabetes mellitus, if possible, below 130/80 mmHg. Art. Achieving a target blood pressure level helps reduce the relative risk of developing fatal and non-fatal conditions/diseases, compared with patients who are not treated or are taking ineffective combinations. Each patient with hypertension needs to reduce excess weight, lead an active lifestyle, stop smoking, limit alcohol consumption (10 - 20 g for women, 20 - 30 for men in terms of pure ethanol), regularly take recommended medications and monitor their effect on blood pressure, enter blood pressure measurement data and other information necessary for the doctor in a special blood pressure self-monitoring diary.
If blood pressure exceed the specified level, then you should discuss with your doctor the possible reasons for the lack of effectiveness of the treatment. Among them:
- in blood pressure has not been identified
- Failure to comply with lifestyle modification recommendations
- Irregular use of antihypertensive drugs
- Inadequate antihypertensive therapy
As practice shows, if the patient trusts his doctor, with competent interaction between the doctor and the patient, in most cases it is possible to control this terrible disease.
What if you are already taking 3 or more medications and your blood pressure has not stabilized at your target level? This form of hypertension is classified as resistant.
Resistant hypertension is a condition in which blood pressure remains above target despite taking a combination of three or more antihypertensive drugs. Uncontrolled hypertension is not synonymous with resistant hypertension. Uncontrolled hypertension is caused by insufficient secondary control of blood pressure due to non-compliance with treatment regimen or true resistance to therapy. The criterion for refractory arterial hypertension is a decrease in systolic blood pressure by less than 15% and diastolic blood pressure by less than 10% from the initial level against the background of rational therapy using adequate doses of three or more antihypertensive drugs.
The lack of adequate blood pressure in more than 2/3 of patients is due to non-compliance with the treatment regimen - pseudo-refractoriness. Another most common and easily eliminated cause of this phenomenon is excessive consumption of table salt. Reasons that are much more difficult to cope with include obesity, alcohol abuse, the use of certain medications, breathing disorders and stopping during sleep, and kidney disease.
The following factors are associated with an increased risk of developing resistant hypertension: older age, high initial blood pressure, obesity, excessive consumption of table salt, chronic kidney disease, diabetes mellitus, left ventricular hypertrophy, female gender. The cause of true refractoriness in hypertension is volume overload associated with inadequate use of diuretics.
What's the solution?
Usually, in the case of resistant (refractory) hypertension, doctors continue to increase the doses of drugs taken by the patient to the maximum tolerated or add sequentially a fourth, fifth, and sometimes a sixth drug from other groups. Patients react to this differently. Many people stop trusting the doctor, some refuse to take medications altogether, because they do not notice any difference between their blood pressure while taking handfuls of medications and without them.
Of course, this decision is fundamentally wrong. In order to avoid progressive target organ damage and serious complications in the future, it is necessary to continue taking medications even if it is not possible to achieve the target blood pressure level. But no one will deny that the use of a multicomponent combination of drugs significantly increases the risk of side effects and unpredictable drug interactions.
What can modern medicine offer in this case? It turns out there is a way out.
Soon in our clinic we will be able to offer a non-surgical method for correcting blood pressure by denervation of the renal arteries. A new procedure, catheter-based renal denervation of the renal arteries, helps control high blood pressure by destroying some of the nerve fibers located in the wall of the renal arteries.
As often happens, the idea of denervation is not new, it is a well-forgotten old thing. Surgeons have long known that excision of the sympathetic nerve fibers responsible for maintaining blood pressure resulted in a decrease in blood pressure. But the procedure could not be used to treat hypertension, since it was accompanied by high operative mortality and long-term complications such as severe hypotension when moving to a vertical position, up to loss of consciousness, dysfunction of the intestines and pelvic organs. But this happens because the sympathetic stimulation of the kidneys and other organs is completely turned off, which leads to an imbalance of nervous regulation. Since the sympathetic nerve fibers innervating the kidney pass directly into the wall of the main renal artery and are adjacent to it, using catheter radiofrequency ablation (RFA) targeted destruction of fibers in the renal arteries will not lead to disruption of the innervation of the abdominal organs and lower extremities. In addition, by destroying only a small part of the nerve endings in the renal arteries, the kidneys are not deprived of nervous regulation. THE CAUSE OF RESISTANT HYPERTENSION IS EXCESSIVE SYMPATHETIC ACTIVITY OF THE KIDNEYS. And catheter RFA allows you to eliminate this excess activity. HYPERTENSION BECOME CONTROLLED.
The introduction of this procedure into our practice is based on a study published in the famous journal Lancet, which showed the safety and effectiveness of the technique, which allows us to achieve a lasting reduction in blood pressure up to 30 mm. rt. Art. from the initial level.
For this treatment, a radiofrequency catheter from Ardian is used, which is inserted through a puncture in the femoral artery. Next, the catheter is passed under X-ray control into the renal artery. Through the tip of the catheter, radiofrequency energy is dosed around the circumference at 4-5 points of the renal arteries. The procedure takes about 40 minutes, after which the catheter is removed. The patient's hospital stay is 24 hours. The condition for the procedure is normal kidney function. But the most striking thing about the procedure is that over time, the therapeutic effect not only does not decrease, but, on the contrary, the blood pressure of the majority gradually and steadily normalizes.
Currently, renal denervation is used only in patients with resistant hypertension. This should lead to approximately a 50% reduction in hypertension-related complications and mortality. This does not mean that medications are no longer needed. Patients will still likely need to take high blood pressure medications, but the number of medications needed to keep blood pressure at target levels will be significantly reduced.
What are the side effects of RFA of the renal arteries?
To date, no serious complications of catheter-based renal denervation have been reported worldwide. The procedure was accompanied by moderate abdominal pain, which was relieved by intravenous analgesics and sedatives. Only one patient had damage to the renal artery by the catheter before RFA, which was corrected by implantation of a stent. The most common complication in a small number of patients was pain and swelling in the groin area. No deterioration in renal function was noted.
Who needs renal denervation?
Denervation of the renal arteries
- Cost: 250,000 rub.
- Duration: 20-30 minutes
- Hospitalization: 1 day in hospital
More details
This intervention is indicated for patients with resistant hypertension, i.e. with a persistent increase in systolic (upper) blood pressure higher than 160 mm Hg. Art., despite the use of 3 or more antihypertensive drugs, including a diuretic. This is especially indicated if the combination of drugs is poorly tolerated or if there are side effects. In this case, patients must be preliminarily examined, and possible secondary causes of arterial hypertension (for example, diseases of the adrenal glands) must be reliably excluded. At the preliminary stage, it is necessary to conduct a computed tomography scan of the renal arteries to clarify the anatomical features of the vessels.
If you have high blood pressure , contact the cardiologists of our center. They will definitely help you.