What is the apical impulse and where is it located?
The heart is a muscle whose general function is to constantly pump blood through the body's circulatory system. It is located at the back of the sternum. Its apex is located above the diaphragm. When the heart beats, the muscles touch the chest wall, which can be felt by placing your hand on the left side of the chest.
The human heart is shaped like a pear. The apical or apical pulse is a heartbeat that is heard at the cardiac apex in the region of the left ventricle. This is one of the chambers of the heart that takes blood from the lungs, moves it to the aortic valve, then to the aortic arch, and the blood then flows through the rest of the body. It's a continuous cycle.
Heart rate is determined by the beat heard at the apex of the heart for one full minute. There are several reasons why this pulse is preferable to counting a detectable heartbeat from the wrist or neck. Some people experience irregular heartbeats that are not always transmitted to the arteries of the extremities.
Therefore, the pulse counted at the wrist may differ from the apical pulse.
The heart rate of young children and infants is estimated from the apical pulse because it is difficult to count the beat rate on the arms or legs of infants.
The apical impulse is normally a rhythmically pulsating protrusion of the intercostal space in the area of the cardiac apex onto the chest wall. It is created by tremors generated during systole. During diastole, the heart returns to its normal position. If the beat of the apex of the heart falls on the rib, then the push is invisible to the doctor.
The apical impulse can also be defined as a systolic protrusion of the space between the ribs. The point of the apical, apical pulsation can be found on the left side of the chest, just below the breast nipple. This position roughly corresponds to the lower pointed end of the heart.
Apex impulse. Characteristics, clinical significance. Changes in pathology.
⇐ PreviousPage 11 of 46Next ⇒
The apical impulse is a protrusion of a limited area of the chest in the region of its apex that occurs rhythmically, synchronously with the activity of the heart. Normally, the apical impulse is located in the 5th intercostal space 1.5-2 cm medially from the midclavicular line. In the position on the left side it moves outward by 3-4 cm, on the right - inward by 1-1.5 cm.
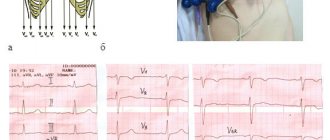
During palpation, the palm of the right hand is placed on the heart area: with the base of the palm towards the sternum, and the fingers between the IV-VII ribs. Also, during palpation, you can ask the patient to tilt the upper half of the body forward or take a deep breath. If the area of the apical impulse in thin people is located opposite the rib, the impulse is invisible.
Width is the area of that part of the chest that shakes under the blow of the apex of the heart. The apex beat is more than 2 cm - diffuse and associated with an enlargement of the left ventricle; less than 2 cm - limited
Height is the amplitude of vibration of the chest wall in the area of the apical impulse. It can be high or low. Depends on the strength of the contraction. The strength of the apical impulse is determined by the pressure felt by the fingers. It depends on the force of contraction of the left ventricle and the thickness of the chest. Resistance of the apical impulse depends on the functional state of the myocardium, its tone, thickness and density of the heart muscle.
Clinical significance: allows you to determine the strength and frequency of heart contraction, allows you to identify left ventricular hypertrophy. Allows you to identify various extracardiac causes (related to the lungs) that change the upper impulse
With compensatory hypertrophy of the left ventricle, the apical impulse shifts to the left to the axillary line and down into the 6-7 intercostal space, becomes diffuse, it is strong, high and highly resistant. A diffuse, but low, weak, soft apical impulse is a sign of developing functional failure of the left ventricular myocardium. With dextracardia, the impulse is determined on the right.
Shifts to the left: LV dilatation : with mitral regurgitation, aortic stenosis, hypertension, atherosclerotic cardiosclerosis. Dilatation of the RV: mitral stenosis, cor pulmonale, tricuspid valve insufficiency, extracardiac: exudate right-sided pleurisy, right-sided hydro-and pneumothorax, left-sided obturator atelectasis Left and down: aortic valve insufficiency, aortic stenosis Shifts left and up: ascites, flatulence, pregnancy, obesity, splenoid and hepatomegaly Shifts to the right: right-sided obstructive atelectasis and pneumosclerosis, left-sided exudative pleurisy and hydrothorax.
To the right and down : emphysema and asthenics
ECG registration method
5 electrodes are used, which are applied to: PR - red, LR - yellow, LN - green, PN - black and white electrode for chest leads. The ECG recording speed is 50 mm/sec , so the duration of 1 mm is 0.02 sec
Standard leads are bipolar leads, when both electrodes (negative on the right hand and positive on the left) are equally active.
Lead I - right hand - left hand.
Lead II - right arm - left leg, summation;
III lead - left arm - left leg.
These leads give a general picture of the bioelectric processes in the heart and its individual topographic formations. Standard lead I gives an idea of focal changes in the anterior wall, and lead III – in the posterior wall of the LV. If we talk about individual chambers of the heart, then I reflects the LV potentials, and III reflects the RV potentials. Reinforced leads according to Goldberg are unipolar leads, where the indifferent electrode (O) is connected to the negative pole, the active one to the positive one on one of the limbs. The potential difference between the electrodes increases, which improves the recording quality and information content. There are 3 limb leads, they are designated by the abbreviations aVR, aVL, aVF. The first letter a comes from the English “augmented” (strengthened), the letter V - “voltage” (voltage); the last letters R, L, F are the location of the electrode: R (right) - on the right hand, L (left) - on the left hand, F (foot) - on the left leg.
Reinforced leads do not have independent significance. Lead аVL duplicates standard lead I, аVF duplicates standard lead III. Lead aVR is on the right arm, the total EMF of the heart is in the opposite direction, i.e. from right to left. In lead aVR, the P, R, and T waves “have a negative value.” Wilson chest leads are unipolar leads. The indifferent electrode represents the connected electrodes from the limbs. The active electrode is placed at various points in the chest. 1st point (V1) in the 4th intercostal space at the lateral edge of the sternum, 2nd point (V2) - 4th intercostal space at the left edge of the sternum, 3rd point (VZ) - along the left parasternal line between the 4th and 5th intercostal spaces 4th point (V4) - in the 5th intercostal space along the left midclavicular line. 5th point (V5) - along the anterior axillary line at the level of V4, 6th point (V6) - along the midaxillary line in the 5th intercostal space. The main purpose of chest leads is topical diagnosis of focal changes in the myocardium. When diagnosing myocardial infarction, leads V1 - V2 reflect the potentials of the interventricular septum , V3 - the anterior wall of the left ventricle, V4 - the apex of the heart, V5 - V6 - the lateral wall of the left ventricle.
The chest leads also provide information about the right and left chambers of the heart. Leads V1 - V2 reflect the potentials of the RV and RA; leads V5 - V6 reflect the LV and LA potentials. Leads VZ – V4 are the transition zone between the right and left chest leads.
Additional chest leads can be used (V7 - V9 - for diagnosing infarctions of the basal parts of the posterior wall of the LV. V7 - along the posterior axillary, V8 - along the scapular, V9 - along the paraventebral lines at the level of position V4 (i.e. in the 5th intercostal space).
Neb leads: electrodes from the limbs are installed on a limited area of the anterior chest wall: red - in the 2nd intercostal space at the right edge of the sternum, yellow - in position V7, and green - in position V4). An Einthoven triangle is formed, where standard lead I will correspond to lead D (dorsalis) and reflects the potentials of the posterolateral wall of the LV, standard lead II will correspond to lead A (anterior) and reflects the potentials of the anterior wall of the LV, standard lead III - lead I (inferior), reflects potentials of the lower parts of the left ventricle.
Precordial mapping allows you to identify small focal changes in the myocardium (including infarctions), which are not accessible to diagnosis with routine leads. In this case, from 35 to 60 electrodes are applied to the heart area according to a certain pattern, and a micro-ECG is recorded from each point. Subsequent analysis using special maps allows us to identify areas of focal changes in the myocardium.
⇐ Previous11Next ⇒
Recommended pages:
Properties normal and abnormal
The apex beat can be heard with your fingers or with a stethoscope. Both options are effective.
When listening to the pulse, you should pay attention to the speed of the heartbeat:
- A slow beat is normal for a person who is in good physical shape. But a slowdown may occur under the influence of certain medications.
- An increased pace in adults indicates that the person has high blood pressure or cardiac problems. It is also typical for people involved in physical exercise and young children.
Before palpation, the pulsation is examined by a doctor under direct and then lateral lighting. The angle of rotation during inspection changes to 90°.
The apical impulse provides a broad picture of cardiac activity to the physician and helps to establish the correct diagnosis.
| Character of the blow | ||
| Fine | Abnormal | |
| Short early (systolic) impulse, felt over an area of 2-3 cm² | Property of momentum | Possible violations |
| Hyperdynamic impulse (very short impulse of large amplitude) | Thyrotoxicosis, anemia, sepsis, vitamin deficiency, ventricular septal defect | |
| Pulsating impulse | Hypertension, aortic stenosis, | |
| Hypodynamic impulse (weak or absent apical impulse) | Myocardial infarction | |
All conclusions about the quality of the apical impulse are based in most cases on subjective analysis and many years of experience of doctors.
Positive and negative
The apical impulse is normally positive, as a rule. In rare cases it may be negative.
Under the influence of the formed pericardial adhesions, a symptom of a negative apical impulse is detected. This occurs when during systole the chest does not protrude at the site of the apical impulse, but is pulled inward.
In the zone of the V intercostal space at the moment of ventricular contraction, a vacuum is formed. As a result, the intercostal space is retracted and a negative apical impulse occurs.
With a positive push, a pulsating protrusion of the space between the ribs occurs.
In what cases is it not determined (not palpated)?
Some physical conditions interfere with the transmission of impulse from the apex to the chest wall:
- obesity;
- pericardial effusion;
- accumulation of fluid in the pleura;
- subcutaneous emphysema.
It is impossible to locate the apical impact site if there is spinal deformity, chest wall deformity, or tracheal deviation.
Why might it be displaced?
The apex beat is normally determined by a limited rhythmic beat. For some people, the impulse may have a diffuse pulsation, be stronger or weaker. The displacement of the apical impulse is influenced by changes in the heart or organs surrounding it.
| Pulse point | Reasons for displacement |
| Shift left | Mitral or aortic valve insufficiency, myocardial damage. Right-sided pleurisy, pneumothorax, hydrothorax, tricuspid valve insufficiency. |
| Offset right | Left-sided pneumothorax, hemothorax, left-sided exudative pleurisy, dextrocardia. |
| Deviation left and down | Aortic valve insufficiency (dilatation of the left ventricle). |
| Mixing towards the center | Displacement of the heart to the right due to left-sided hydrothorax, pneumothorax, pneumosclerosis. |
| Shift up and left | Occurs in conditions when the level of the diaphragm increases (flatulence, obesity, acidosis). |
Do not confuse thrust displacement with displacement. If the patient lies on the left side, then the apical pulsation shifts to the left by 3-4 cm. When lying on the right side, the displacement occurs to the right by 1.5 cm. In pregnant women with increased weight, the pulse moves to the left. For people with nicotine addiction - to the right.
A stable change in the location of the pulse, displacement, occurs due to internal disorders.
Width and area
The area of the apical impulse is determined by the width between II and IV and the fingers located at the outer and inner borders of the visible pulsation. The indicator for a healthy person does not exceed 2 cm. If the width is less than 2 cm, such a push is called limited.
An increase in area was noted among athletes and people engaged in heavy physical labor.
What affects the change in the area of the apex beat:
| Increased area | Reduced area |
| Myocarditis | Well developed muscles |
| Heart defects | Narrow intercostal spaces |
| Hypertension | Enhanced nutrition |
| Tumor of the posterior mediastinum | |
| Left ventricular dilatation |
The boundaries of the push are established at the 1st stage of palpation. The doctor gives a qualitative assessment during the 2nd stage of palpating the patient.
Spilled
A diffuse cardiac impulse can be felt in 2 or more intercostal spaces.
An enhanced apical impulse, the area of which is more than 2 cm² (spread), indicates hypertrophy of the right or both ventricles of the heart.
In case of enlargement of the left ventricle, the apical pulse is shifted downwards, has a local point, and is often strengthened.
Limited
A localized pulse is felt in the 5th intercostal space. The location is influenced by gender, human constitution, and the level of the diaphragm. In some women, the impulse is determined in the area of the IV intercostal space; in hypersthenics, it falls on the midclavicular line.
Height
A high apical pulse is determined by the amplitude of finger lifting and manifests itself in the following cases:
- accelerated heartbeat;
- high diaphragm position;
- deep exhalation, during which the cardiac apex moves closer to the chest wall;
- tumor of the posterior mediastinum;
- left ventricular hypertrophy.
Low shock occurs when:
- obesity;
- left-sided exudative pleurisy;
- pericarditis;
- deep breath;
- emphysema.
The apex beat normally has an average height. It is characteristic of normosthenics, people with a normal width of intercostal distances.
The range of oscillations of the intercostal space does not exceed 2-3 mm and depends on several factors:
- thickness of the chest wall;
- dynamics of myocardial contractility;
- hemodynamic type of state of the cardiovascular system.
Force
The strength of the apical impulse can be determined as follows:
- an increased push raises the finger;
- pulsating, of medium strength, easily identified, but the finger does not lift;
- a weak push is hard to find.
The strength of the pulsating impulse, as well as the area, depends on the location of the heart in the chest, but mainly on the contractile power of the left ventricle.
A pulsation of average strength is determined in a person with a moderate diet, standard physical development, and normal hemodynamics.
Intensified shocks occur with increasing speed and strength of contractile work of the left ventricle. It is observed more often in athletes, in people after emotional stress or workload. Pathological causes are associated with left ventricular hypertrophy, tumor of the posterior mediastinum, thyrotoxicosis, and shrinkage of the lung tissue.
Weak tremors can be detected in completely healthy people. These include patients with enhanced nutrition and powerfully developed muscles.
Pathologies affecting the decrease in thrust force:
- subcutaneous emphysema;
- obesity;
- left-sided pneumothorax;
- adhesive pericarditis;
- cardiosclerosis;
- heart defects.
The most alarming cause of decreased strength is a decrease in myocardial contractility.
If the doctor notices the simultaneity of changes in some parameters, then on this basis the following conclusions are drawn:
| Properties | Volume | Violation | Volume | Violation | Volume | Violation |
| Square | Increased | Normal myocardial contractility, muscle hypertrophy | Increased | Dilatation of the left ventricle, decrease in its functions | Reduced | Myocardial damage |
| Height | Increased | Increased | Reduced | |||
| Force | Increased | Reduced | Reduced |
The strength or weakness of the apical impulse is determined during a deep inspiration, and the patient should lie on his back.
Resistance
The presence of resistance is determined by the force of finger pressure that must be applied to “extinguish” the apical impulse. With high blood pressure, narrowing of the aortic mouth, obstacles arise for the flow of blood from the left ventricle to the aorta. This makes the apex impulse unyielding and resistant.
The pulse may be moderate when the tissue is perceived as pliable upon palpation. The impulse is called resistant if the tissue is dense, which occurs with left ventricular hypertrophy. The pulsation can become dome-shaped when the area and force of the push are increased. More often this occurs with aortic defects.
Other types of unwanted vibrations
In the case when the cardiac impulse becomes diffuse and affects other areas, such as the armpit, epigastric region, it becomes widespread. This condition is characteristic of heart disease.
In cardiology, the symptom of “cat purring” is also known. This occurs due to trembling of the chest wall. It is determined by digital or palmar palpation and is caused by low-frequency fluctuations in the blood flow that passes through the narrowed opening of the valve.
The detected sign is compared with the pulse in the carotid artery. If the beats coincide, then a systolic “purr” is detected. If the apical impulse and the blow on the carotid artery do not coincide, then a diastolic “purr” is noted.
Systolic tremors are characteristic of narrowing of the pulmonary artery. Diastolic manifests itself in stenosis of the right atrioventricular orifice, which is a rare defect.
Characteristics of the apical impulse
When determining the apex beat, the following indicators are assessed.
1) Localization of the apex beat. Normally, it is determined in the 5th intercostal space 1-2 cm medially from the left midclavicular line.
a) A shift to the left is observed with dilatation of the left ventricle (insufficiency of the aortic or mitral valves, myocardial damage with the development of dilatation of the heart chambers). A displacement of the apical beat to the left is also possible in the presence of pathological processes that cause a displacement of the heart to the left (right-sided pleurisy, hydrothorax, pneumothorax, left-sided pneumosclerosis). The apical impulse is shifted to the left also as a result of its displacement by the dilated right ventricle (tricuspid valve insufficiency, stenosis of the left atrioventricular orifice).
b) A shift of the apex impulse to the left and down is observed with severe dilatation of the left ventricle (aortic valve insufficiency).
c) A shift to the left and up is observed in conditions accompanied by an increase in the level of the diaphragm (ascites, flatulence, obesity).
d) Inward displacement occurs as a result of displacement of the entire heart to the right due to left-sided exudative pleurisy, hydrothorax, pneumothorax or due to right-sided obstructive atelectasis, pneumosclerosis.
2) The area of the apex beat (or its width in centimeters) is the distance between the II and IV fingers located at the inner and outer borders of the palpated apex beat. In a healthy person, this figure does not exceed 2 cm. If the width of the apex beat is less than 2 cm, it is called limited. If the width of the apex beat is more than 2 cm, it is called diffuse. A diffuse apical impulse is detected with dilatation of the left ventricle (insufficiency of the aortic or mitral valves, myocardial damage with the development of dilatation of the heart chambers).
3) The strength of the apical impulse. Determined by the force of impact on the fingers. A strong apex beat is observed with increased cardiac activity (for example, with significant physical activity) or with pathology (left ventricular hypertrophy).
4) Height of the apex beat. Determined by the amplitude of finger lifting. A high apical impulse is detected in pathological conditions accompanied by diastolic overflow of the left ventricle. It is observed with insufficiency of the aortic valves, with severe insufficiency of the mitral valve.
5) Resistance to the apex beat. It is determined by the force of finger pressure that must be applied to “extinguish” the apical impulse. A resistant (i.e., unyielding) apical impulse is determined when there is an obstacle to the expulsion of blood from the left ventricle into the aorta (with stenosis of the aortic mouth, high blood pressure).
6) Negative apical impulse is a retraction of the chest above the projection of the apex of the heart in systole. The symptom is found in constrictive pericarditis and is the result of the formation of pericardial adhesions.
7) The symptom of “cat purring” is a vibration of the chest wall, reminiscent of a cat purring. The appearance of this symptom is due to low-frequency fluctuations in the blood stream as it passes through the narrowed (stenotic) valve opening. If there is a symptom of “cat purring”, it must be compared with the pulse in the carotid artery. If the vibration coincides with the pulse impulse on the carotid artery, a systolic “cat purr” is detected; if it does not coincide, a diastolic one is noted. The appearance of a diastolic “cat purr” during palpation of the apex beat is characteristic of mitral stenosis. This symptom can also be detected in the second intercostal space to the left and right of the sternum and at the base of the xiphoid process. Systolic trembling in the second intercostal space to the right of the sternum occurs when the aortic valve or aortic lumen narrows. Systolic trembling in the second intercostal space to the left of the sternum occurs when the mouth of the pulmonary artery narrows with an open ductus arteriosus. Diastolic tremor over the region of the xiphoid process is detected with stenosis of the right atrioventricular orifice (a rare defect).
PERCUSSION OF THE HEART
During percussion examination of the heart, the following indicators should be determined:
1) boundaries of relative cardiac dullness (borders of the heart);
2) position of the heart (variants of abnormal position of the heart are identified);
3) configuration of the heart, dimensions of the diameter of the heart and vascular bundle;
4) the boundaries of absolute dullness of the heart (the anterior surface of the heart, not covered by the lungs).
Limits of relative cardiac dullness
Determination of the right border of relative cardiac dullness. Place the pessimeter finger in the 2nd intercostal space along the right midclavicular line. First, the height of the diaphragm (the lower border of the lung) is determined. To do this, percussion is performed with a weak percussion blow down the intercostal space until the pulmonary sound disappears and a dull sound appears. The border is marked on the side of the pessimeter finger facing the clear pulmonary sound. Place your finger on the rib above. At a normal height of the diaphragm, the pessimeter finger will be in the 4th intercostal space. Place the pessimeter finger on the midclavicular line parallel to the right edge of the sternum. Carry out percussion, applying blows of medium force towards the edge of the sternum until the pulmonary sound disappears and a dull sound appears. The right limit of relative cardiac dullness will be determined. It is formed by the right atrium. In a healthy person, the right border of the relative dullness of the heart is located in the IV intercostal space and is 1.5-2 cm from the right edge of the sternum (Fig. 4.4.).
Determination of the left border of relative dullness of the heart. It begins with palpation of the apical impulse, after which the finger-pessimeter is placed vertically in the 5th intercostal space 1-2 cm outward from the outer edge of the apical impulse. If the apical impulse is not detected, percussion is carried out in the 5th intercostal space from the left mid-axillary line, applying blows of medium strength until the pulmonary percussion sound disappears and a dull sound appears. The established border is marked along the edge of the pessimeter finger on the side of the clear pulmonary sound. The left border of the relative dullness of the heart is formed by the left ventricle and coincides with the outer edge of the apex beat. Normally, the left border of the relative dullness of the heart is located in the 5th intercostal space 1-1.5 cm medially from the midclavicular line (Fig. 4.5.).
Determination of the upper limit of relative cardiac dullness. Place the pessimeter finger under the left collarbone parallel to the ribs so that the middle phalanx is directly at the left edge of the sternum. Apply percussion blows of medium strength. When the pulmonary sound disappears and the percussion sound appears, mark the border along the upper edge of the plessimeter finger (i.e., along the edge of the finger facing the clear pulmonary sound). The upper limit of relative dullness is formed by the conus pulmonary artery and the left atrial appendage. Normally, the upper limit of relative dullness runs along the upper edge of the third rib (Fig. 4.6.).
Changes in the percussion boundaries of the heart may be due to:
a) changes in the size of the heart or its chambers;
b) change in the position of the heart in the chest.
Shift of the right border of relative dullness of the heart to the right. This displacement occurs in pathological conditions accompanied by dilatation of the right atrium or right ventricle. The border may shift to the right with exudative pericarditis and hydropericardium.
Shift of the left border of the relative dullness of the heart to the left. This displacement occurs in pathological conditions accompanied by dilatation of the left ventricle. The dilated right ventricle in some cases can “push” the left ventricle outward, which causes a shift of the left border of the relative dullness of the heart to the left.
Shift of the upper limit of the relative dullness of the heart upward. This displacement occurs when the left atrium and/or conus pulmonary artery dilates.
Heart position
The following options for abnormal position of the heart are possible:
− dextracardia (congenital condition);
− displacement of the heart to the right (observed with left-sided pneumothorax, obstructive atelectasis of the right lung, right-sided pneumothorax);
− displacement of the heart to the left (observed with right-sided pneumothorax, right-sided exudative pleurisy, obstructive atelectasis of the left lung, left-sided pneumosclerosis).
Configuration of the heart, dimensions of the diameter of the heart and vascular bundle
The right and left contours of the heart are determined. To determine the right contour of the heart, percussion is performed at the level of IV, III, II intercostal spaces. To establish the left contour of the heart, percussion is performed at the level of the V, IV, III, II intercostal spaces. Since the boundaries of the heart at the level of the IV intercostal space on the right and the V intercostal space on the left have already been established when determining the boundaries of relative dullness of the heart, it remains to determine them at the level of IV, III, II intercostal spaces on the left and III, II intercostal spaces on the right.
Determination of the contours of the heart at the level of III and II intercostal spaces on the right and IV-II intercostal spaces on the left. The starting position of the pessimeter finger is on the midclavicular line on the corresponding side. The middle of the middle phalanx of the pessimeter finger should be in the corresponding intercostal space. Percussion is carried out with blows of medium strength. The pessimeter finger is moved towards the heart. When a dull sound appears, a boundary is marked along the edge of the finger-pessimeter facing the clear pulmonary sound (i.e., from the heart).
Normally, the right contour of the heart at the level of the II and III intercostal spaces is located along the right edge of the sternum, at the level of the IV intercostal space, 1-2 cm outward from the right edge of the sternum. The left contour of the heart at the level of the 2nd intercostal space is located along the left edge of the sternum, at the level of the 3rd intercostal space along the left parasternal line, at the level of the 4th and 5th intercostal spaces, 1-2 cm medially from the left midclavicular line.
The following pathological configurations of the heart are of diagnostic importance:
a) mitral;
b) aortic;
c) trapezoidal.
Mitral configuration. It is characterized by outward bulging of the upper part of the left contour, caused by dilatation of the left atrium and conus of the pulmonary artery. The waist of the heart is smoothed. This configuration is detected with stenosis of the left atrioventricular orifice and with mitral valve insufficiency.
Aortic configuration. It is characterized by outward bulging of the lower part of the left circuit, caused by dilatation of the left ventricle. The waist of the heart is emphasized. The shape of the heart resembles a felt boot or a duck sitting on the water. The aortic configuration is observed with aortic valve insufficiency and aortic stenosis.
Trapezoidal configuration. It is characterized by an almost symmetrical bulging of both contours of the heart, more pronounced in the lower parts. This configuration is observed with exudative pericarditis and hydrothorax.
Width of the vascular bundle. The contours of the heart, defined in the second intercostal space on the right and left, correspond to the width of the vascular bundle. Normally, the right border of the vascular bundle runs along the right edge of the sternum. It is formed by the aorta or superior vena cava. The left border of the vascular bundle normally runs along the left edge of the sternum. It is formed by the pulmonary artery. Normally, the width of the vascular bundle is 5-6 cm. An increase in the diameter of the vascular bundle is observed with atherosclerosis and aortic aneurysm.
Measuring the diameter of the heart. The length of the diameter of the heart is the sum of two sizes - right and left. The diameter of the heart in a healthy person is 11-13 cm. The right size is the distance from the right border of the relative dullness of the heart to the anterior midline. Normally, it is 3-4 cm. The left dimension is the distance from the left border of the relative dullness of the heart to the anterior midline. Normally it is 8-9 cm.
An increase in the size of the right component of the diameter of the heart occurs in pathological conditions accompanied by dilatation of the right atrium and right ventricle. Exudative pericarditis and hydropericardium also lead to an increase in the size of the right component of the diameter of the heart.
An increase in the size of the left component of the diameter of the heart occurs in pathological conditions accompanied by dilatation of the left, and in some cases, the right ventricle.
Limits of absolute dullness of the heart
The right, left and upper boundaries of absolute cardiac dullness are determined.
Determination of the right limit of absolute cardiac dullness. The initial location of the finger-pessimeter is the right border of the relative dullness of the heart (at the level of the IV intercostal space). Percussion is carried out with the quietest beats (threshold percussion). Continuing percussion, the pessimeter finger is moved inward. When the percussion sound changes from loud to dull (at the same time, the palpation perception of the percussion blow clearly changes, it becomes softer), the percussion is stopped and the border is marked along the edge of the pessimeter finger facing the right lung (the right border of absolute dullness of the heart). Determine the coordinates of the border.
Determination of the left border of absolute cardiac dullness. The initial location of the finger-pessimeter is the left border of the relative dullness of the heart (at the level of the 5th intercostal space). Percussion is carried out with the quietest beats (threshold percussion). Continuing percussion, the pessimeter finger is moved inward. When the percussion sound changes from loud to dull, the percussion is stopped and the border is marked along the edge of the plessimeter finger facing the left lung (the left border of absolute dullness of the heart). Determine the coordinates of the border.
Determination of the upper limit of absolute cardiac dullness. The initial location of the finger-pessimeter is the upper limit of the relative dullness of the heart. Percussion is carried out with the quietest blows. Continuing percussion, the pessimeter finger is moved downwards. When the percussion sound changes from loud to dull, the percussion is stopped and the border is marked along the upper edge of the finger (the upper limit of absolute dullness of the heart). Determine the level of this boundary in relation to the ribs.
Normally, the right border of absolute cardiac dullness is located along the left edge of the sternum, the left coincides with the border of relative cardiac dullness or deviates 1 cm inward from it, the upper one is located at the level of the 4th rib.
An increase in the area of absolute dullness of the heart occurs when:
a) pathological conditions accompanied by dilatation of the right ventricle;
b) exudative pericarditis or hydropericardium;
c) pathological processes occurring outside the heart, but causing a tighter fit of the heart to the anterior chest wall (for example, with a tumor of the posterior mediastinum).
A decrease in the area of absolute dullness of the heart occurs with pulmonary emphysema.
AUSCULTATION OF THE HEART. TONES
The purpose of cardiac auscultation is to listen and evaluate the sound phenomena that occur during the work of the heart. Two types of sound phenomena are recorded:
1) abrupt, short sounds heard in the region of the heart and synchronously associated with its activity - tones;
2) prolonged sounds - noises that in the vast majority of cases indicate the development of pathology.
Cardiac sound phenomena are naturally associated with cardiac cycles, repeating with them. In a healthy adult, when listening to the heart, a melody of two tones is heard. In healthy adolescents, it is sometimes possible to listen to a melody of three (rarely) or four (very rarely) tones.
Heart sounds have very complex formation mechanisms.
I (systolic) tone occurs predominantly in the phase of isovolumetric contraction of the ventricles, when, as a result of a rapid increase in pressure in the cavity of the ventricles, oscillations of various structures of the ventricles of the heart occur. The first tone is formed by the following components:
1) valvular (slamming of atrioventricular valves);
2) muscular (sharp rise in pressure in the ventricles);
3) vascular (oscillations of the great vessels at the very beginning of blood expulsion).
II (diastolic) tone occurs at the very beginning of ventricular diastole (in protodiastole), when the pressure in the ventricles quickly decreases and becomes lower than in the aorta and pulmonary artery. As a result, blood from the vessels rushes back into the ventricles, which leads to the slamming of the semilunar valves, short-term vibration of the valve leaflets, the walls of the aorta and pulmonary artery. Thus, the second tone is formed by the following components:
a) valve;
b) vascular.
The aortic component of the second sound normally and in the vast majority of cases in pathology precedes the pulmonary component. This is because the aortic valve closes earlier.
Normal indicators in children and adults by age
Table of apical pulse indicators:
| Age group | Readings are normal |
| Newborns | 80 – 140 beats/min |
| Children from 4 to 9 years old | 75 – 120 beats/min. |
| Children under 15 years old | 50 -90 beats/min |
| Adults | 60 – 100 beats/min. |
The apex beat is normal in an adult if it does not exceed 100 or not lower than 60 beats/min. The ideal heart rate at rest and during physical activity varies from person to person.
Reasons why your heart rate may increase:
- fear or anxiety;
- heat;
- recent physical activity;
- pain;
- hypotension;
- blood loss;
- insufficient oxygen consumption.
Additionally, a heart rate that is consistently higher than normal may be a sign of heart disease, heart failure, or an overactive thyroid gland. The decrease is affected by medications that can affect the heart rate.
Step-by-step palpation algorithm
Palpation of the apical pulse is carried out in 2 stages. To do this, landmarks on the body are used.
They include:
- bony point of the sternum;
- intercostal spaces;
- the midclavicular line (an imaginary line running down the body from the middle of the collarbone).
Stage I:
- The doctor stands to the right of the patient. The right hand is placed on the patient's chest. The base of the hand rests on the sternum, and the fingers cover the area from the III to VI ribs.
- The doctor presses the hand to the chest, bending the II, III, IV fingers, looking for the place of vibration of the intercostal space.
If the pulsation is not detected, the patient should lean forward 50°. This is done to bring the heart as close to the chest as possible. Before bending over, you need to exhale.
At the 2nd stage of palpation, the doctor determines the location of the push, type, area, strength, compliance, height.
Palpation technique:
- The doctor turns his hand with his fingers upward at the site of the found pulsation. The phalanges of the fingers should be located along the intercostal space.
- Slowly moving the fingers, slightly plunging them into the intercostal space, the doctor assesses the quality of the pulse.
The apex beat can be seen in only 50% of people. In others, it is hidden by a layer of fat, muscle, distance of the heart from the chest, or is affected by emphysema, which often accompanies older patients. Pulsation is clearly visible in asthenics, normosthenics and people with a thin fat and muscle layer.
PALPATION
Ø Palpation of the apical impulse: its localization, character (positive or negative), area (limited or diffuse), strength (normal or ordinary, enhanced, rising, dome-shaped); resistance (elasticity).
Ø Palpation of the heart area to determine pain and detect trembling, “cat purring”.
| Rice. 20. Determination of the localization of the apex beat | Rice. 21. Determination of the properties of the apex beat |
If there is a visible apex beat, palpation is carried out according to the place where it is visible. If the apical impulse is not visible, then you should place the palm of your right hand on the left anterior axillary line at the level of 4-6 ribs and move it towards the sternum until a pulsation is felt. Then, using the flesh of the end phalanges of three bent fingers, placed perpendicular to the surface of the chest, the location of the push is specified (Table 7, Fig. 20, 21).
The localization of the push is determined by two landmarks: the intercostal spaces and the relation in cm to the left midclavicular line. Normally, the apical impulse in a vertical position of the patient is located 1-2 cm medially from the left midclavicular line in the 5th intercostal space. A shift of the apical impulse to the left can be observed with expansion of both the left and right ventricles. The localization of the apical impulse is influenced by the position of the patient at the time of the study, as well as extracardiac factors (height of the diaphragm, condition of the lungs).
The area of the apical impulse normally does not extend beyond the area of the pads of the 2 fingers, that is, does not exceed 2 cm. Such an impulse is called limited. An apical impulse exceeding 2 cm is called diffuse. A diffuse apical impulse is characteristic of dilatation of the left ventricle.
The strength of the push is determined by the pressure that the push puts on the fingers. If you manage to restrain the apical impulse with a little effort with your fingers, then it is of normal strength (non-resistant); if this cannot be done and the fingers are lifted by the impulse, then the apical impulse is strengthened (resistant). A sharply enhanced apical impulse is sometimes called dome-shaped (with severe stenosis of the aortic mouth).
The apex beat is not always detected by palpation. The absence of an apex beat on palpation is not a sign of pathology; it may occur on the rib.
Table 7
Options for shifting the apex beat
| Bias | Extracardiac causes | Heart reasons |
| Up and left | Pregnancy, ascites, obesity, flatulence, tumors | |
| Down and right | After childbirth, with weight loss, emphysema. Visceroptosis, asthenic body type | |
| Left | Right-sided exudative pleurisy, hydrothorax, pneumothorax on the right | Left ventricular hypertrophy |
| Down and left | Aortic valve insufficiency | |
| Right | Pleuropericardial adhesions and shrinkage of the lungs with proliferation of connective tissue; obstructive atelectasis of the lungs on the right | |
| Absence | Large accumulation of fluid in the left pleural cavity; normally closed by a rib in 1/3 of cases | Severe effusion pericarditis |
“ Cat purring” (fremissement cataire) is reminiscent of the sensation of stroking a purring cat. “Cat purr” is detected in the area of the apex of the heart, in the 2nd intercostal space to the right of the sternum, in the 2nd intercostal space to the left of the sternum, in the 4th intercostal space at the right edge of the sternum. To determine it, you need to place the palm of your right hand flat in the already indicated areas (Fig. 22). In the presence of “cat purring”, it is necessary not only to identify its localization, but also the phase in which it is detected, that is, in systole or diastole. Systolic “cat purring” in the 2nd intercostal space to the right of the sternum is characteristic of aortic stenosis, in the 2nd intercostal space to the left of the sternum is characteristic of pulmonary artery stenosis. Diastolic “cat purring” at the apex of the heart is characteristic of mitral stenosis, in the 4th intercostal space at the right edge of the sternum - for tricuspid foramen stenosis. “Cat purring” is thus an important symptom for diagnosing stenosis of the main large openings of the heart. “Cat purring” in the 2.3 intercostal space to the left of the sternum, detected in systole and diastole, should be associated with patent ductus botallus.
| A | b |
Rice. 22. Definition of “cat purr”:
a – position of the hand during palpation; b – palpation zones
SAMPLE record for a healthy person. The apical impulse is palpated in the 5th intercostal space 1 cm medially from the left midclavicular line; positive, limited, ordinary strength. "Fremissement cataire" is not defined.
What is a cardiac impulse?
The shaking of the anterior chest wall caused by the contraction of the heart is called a cardiac impulse. It occurs synchronously with ventricular systole.
In the tension phase, the shape and size of the heart changes, which makes it possible for the surface of the ventricles to come into contact with the chest wall. The study of the cardiac impulse is carried out using inspection, palpation, and a sound signal.
Determination algorithm
The heartbeat is palpated as follows:
- The doctor's hand is placed on the precordial area, the fingers are at the level of the apical impulse, and the palm is at the right edge of the sternum, then palpation is performed. This is how the precordial region is assessed.
- Having assessed the condition at this level, the doctor’s hand moves to the third rib and palpation is also carried out here.
Thus, the doctor, with an existing cardiac impulse, distinguishes between the vibration of the lower part of the sternum, the pulse at the edges of the sternum and the epigastric pulsation.
Diseases detected by palpation, features of apical impulses in pathologies
The most common disorder that is revealed by palpation is an increase in the volume of the left ventricle, when the pressure in the systemic circulation steadily increases. This is affected by alcohol abuse and physical overload. This is an acquired pathology that is eliminated over time. But it is possible to identify other violations, more serious.
For hypertension
In the early stages, hypertension is not clearly expressed. However, even during this period, symptoms can be identified: headache, heart pain, vascular neurosis. The development of the disease is influenced by left ventricular hypertrophy. On palpation, an enhanced apical impulse is detected.
Other properties of apical pulsation:
- push is positive;
- spilled;
- resistant;
- domed in some cases;
- has a shift to the left and down.
With ventricular hypertrophy
This is a condition in which the muscles of the left ventricle thicken, often associated with uncontrolled hypertension. The process is not permanent, but in some cases can lead to heart failure. When the underlying problem is treated, the thickened ventricle may shrink in size over time.
With hypertrophy, the force of the apical impulse increases, a displacement occurs to the anterior axillary line, and down to the 6–7 intercostal space. The pulsation becomes diffuse, high, and takes on a dome-shaped shape.
For coronary heart disease
Insufficient supply of the heart muscle with oxygen and nutrients leads to myocardial damage. The main factor in the development of the disease is atherosclerosis of the coronary arteries, which reduces the blood supply to the heart muscle.
Upon visual examination of the heart area, the apex beat is not detected.
Upon palpation, the doctor determines:
- positive apical impulse;
- palpation of the pulse is carried out in the 5th intercostal space towards the outer side of the left midclavicular line;
- pulsation diffuse, low, resistant;
- shock area 3 cm².
Listening to the apical impulse is the most effective way to assess cardiac activity. If your pulse is outside the normal range or there is an irregular heartbeat, you should definitely visit a cardiologist.
Author: Belyaeva Anna
Palpation of the heart area. Apex beat
Palpation of the heart area makes it possible to better characterize the apex beat of the heart
, detect a heartbeat, evaluate visible pulsation or detect it, detect tremors of the chest (symptom of “cat purring”).
To determine the apical impulse of the heart, the right hand, palmar surface, is placed on the left half of the patient’s chest in the area from the sternal line to the anterior axillary between the 3rd and 4th ribs (in women, the left mammary gland is first retracted up and to the right). In this case, the base of the hand should be facing the sternum. First, the push is determined with the entire palm, then, without lifting the hand, with the flesh of the end phalanx of the finger placed perpendicular to the surface of the chest (Fig. 38).
Rice. 38. Determination of the apical impulse: a - palmar surface of the hand; b - the end phalanx of the bent finger.
Palpation of the apical impulse can be facilitated by bending the patient's torso forward or by palpation during deep exhalation. In this case, the heart is more closely adjacent to the chest wall, which is also observed in the position of the patient on the left side (in the case of turning on the left side, the heart shifts to the left by about 2 cm, which must be taken into account when determining the location of the push).
When palpating, pay attention to the localization, extent, height and resistance of the apical impulse.
Normally, the apical impulse is located in the 5th intercostal space at a distance of 1-1.5 cm medially from the left midclavicular line. Its displacement can cause an increase in pressure in the abdominal cavity, leading to an increase in the position of the diaphragm (during pregnancy, ascites, flatulence, tumors, etc.). In such cases, the impulse moves up and to the left, as the heart turns up and to the left, taking a horizontal position. When the diaphragm is low due to a decrease in pressure in the abdominal cavity (with weight loss, visceroptosis, emphysema, etc.), the apical impulse moves down and inward (to the right), as the heart turns down and to the right and takes a more vertical position.
An increase in pressure in one of the pleural cavities (with exudative pleurisy, unilateral hydro-, hemo- or pneumothorax) causes a displacement of the heart and, consequently, the apical impulse in the direction opposite to the process. Wrinkling of the lungs as a result of the proliferation of connective tissue (with obstructive pulmonary atelectasis, bronchogenic cancer) causes a displacement of the apical impulse to the painful side. The reason for this is a decrease in intrathoracic pressure in the half of the chest where the shrinkage occurred.
As the left ventricle of the heart enlarges, the apical impulse shifts to the left. This is observed with bicuspid valve insufficiency, arterial hypertension, and cardiosclerosis. With aortic valve insufficiency or narrowing of the aortic opening, the impulse can shift simultaneously to the left (up to the axillary line) and down (to the VI - VII intercostal space). In the case of dilation of the right ventricle, the impulse may also shift to the left, since the left ventricle is pushed by the dilated right ventricle to the left. With a congenital abnormal location of the heart on the right (dextracardia), the apical impulse is observed in the 5th intercostal space at a distance of 1-1.5 cm inward from the right midclavicular line.
With pronounced effusion pericarditis and left-sided exudative pleurisy, the apex beat is not detected.
The normal distribution (area) of the apex beat is 2 cm2. If its area is smaller, it is called limited; if it is larger, it is called diffuse.
Limited apical impulse
noted in cases where the heart is adjacent to the chest with a smaller surface than normal (occurs with emphysema, with a low diaphragm).
Spilled apical impulse
usually caused by an increase in the size of the heart (especially the left ventricle, which occurs with insufficiency of the mitral and aortic valves, arterial hypertension, etc.) and occurs when it is mostly adjacent to the chest. A diffuse apical impulse is also possible with wrinkling of the lungs, high standing of the diaphragm, with a tumor of the posterior mediastinum, etc.
Apex beat height
characterized by the amplitude of vibration of the chest wall in the region of the apex of the heart. There are high and low apical impulses, which are inversely proportional to the thickness of the chest wall and the distance from it to the heart. The height of the apical impulse is directly dependent on the strength and speed of heart contraction (increases with physical activity, anxiety, fever, thyrotoxicosis).
Apex beat resistance
determined by the density and thickness of the heart muscle, as well as the force with which it protrudes the chest wall. High resistance is a sign of hypertrophy of the left ventricular muscle, no matter what causes it. The resistance of the apical impulse is measured by the pressure it exerts on the palpating finger and the force that must be applied to overcome it. A strong, diffuse and resistant apical impulse upon palpation gives the sensation of a dense, elastic dome. Therefore, it is called a dome-shaped (elevating) apical impulse. Such a push is a characteristic sign of aortic heart disease, i.e. insufficiency of the aortic valve or narrowing of the aortic opening.
Heart beat
palpated over the entire palmar surface of the hand and is felt as a shaking of the chest area in the area of absolute dullness of the heart (IV-V intercostal space to the left of the sternum). A pronounced cardiac impulse indicates significant hypertrophy of the right ventricle.
The symptom of “cat purring” is of great diagnostic importance.
: The trembling of the chest resembles the purring of a cat when stroking it. It is formed when blood quickly passes through a narrowed hole, resulting in vortex movements that are transmitted through the heart muscle to the surface of the chest. To identify it, you need to place your palm on those places in the chest where it is customary to listen to the heart. The sensation of a “cat’s purr”, detected during diastole at the apex of the heart, is a characteristic sign of mitral stenosis; during systole in the aorta - aortic stenosis; in the pulmonary artery - pulmonary artery stenosis or patent ductus arteriosus.
In English: