Features of the respiratory system in a child
During the period of intrauterine development of the fetus, the formation and development of vital organs occurs. Their formation is completed after birth. The respiratory system begins to function at full capacity only in adulthood.
Distinctive features of the respiratory system in children:
- At birth, the baby takes its first breath and the lungs open. Their volume is much smaller than the size of the chest. But it contains a sufficient number of blood vessels. To saturate their organs with oxygen, children make breathing movements more often than adults ;
- The large number of breathing movements of children is also due to the fact that the bulk of oxygen enters through the nasal passages. In children, they are narrow and short and contain a large number of lymphatic and blood vessels. At the slightest irritation (dust, infection or allergens), swelling of the mucous membrane occurs, which further complicates the passage of air into the lungs.
Children are not good at breathing through the mouth, so parents are advised to clean their nasal passages more often.
Importance of indicators
With the help of measurements you will find out how correctly the ventilation is working. If you notice rapid breathing, this means that your breathing is now shallow. This problem leads to the formation of pathogenic microflora in the body. The frequency of breathing movements depends on how cheerfully the baby behaved all day. If he lay there all the time, then the number of breaths may be much less.
- Heart rate norms for women: Table by age at rest and during training
Measuring your baby's heart rate helps check his overall health. Therapists check both of these indications every time they examine the baby. If the measurements were taken over several days (which makes them more accurate), show them to a specialist. Pay special attention to newborns, because they cannot tell that something hurts.
Methods for calculating the breathing rate of a child
The respiratory rate in children (the norm by age has significant differences) is checked by pediatricians during monthly examinations and compared with indicators for the child’s age. Parents can count the number of inhalations and exhalations themselves. When determining indicators, you need to take into account the child’s age, weight category, general health condition and time of day.
Sequence of performing the procedure at home:
- Determine the child's breathing type. Up to 4 years of age, children predominate in belly breathing, that is, when inhaling and exhaling, the peritoneum (abdomen) rises and falls. From 4 to 10 years, predominantly chest breathing is observed. The rise and fall of the chest is visually noted. After 10 years, abdominal breathing predominates in males, and chest breathing in females.
- After determining the type of breathing, you need to prepare a watch with a second hand and bring the child into a calm state. Playing games, watching cartoons, or being scared about the upcoming procedure will not allow you to obtain accurate data. In infants, it is recommended to take measurements during sleep. The indicator will be slightly lower than during the waking period.
- A comfortable position for correctly counting inhalations and exhalations is a lying position. Children from 1 to 5 years old can be calmed with a rattle or calm conversation. In this case, the participation of 2 parents will be required.
- The number of breathing movements can be assessed visually or by placing your hand on your stomach or ribs.
- The most accurate indicators are those measured in 1 minute. If the child is fidgety, then it is allowed to make calculations for 15 or 30 seconds. Multiply the resulting number by 4 or 2. But the data will have an error.
- To increase the measurement accuracy, the procedure must be performed 3-4 times. The resulting arithmetic mean will give the exact number that needs to be compared with the age norm.
At the same time, it is recommended to measure the number of heartbeats. If there is a deviation in the indicators, the child should be shown to a pediatrician. The specialist will re-measure the indicator, taking into account accompanying factors (excess weight, presence of a runny nose).
Treatment strategy
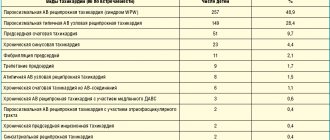
After a comprehensive examination of the child, a therapeutic program is developed. Taking into account the severity of the violations, the following technologies are often used:
- Rinsing the nasal passages and prescribing special medications.
- Creating positive pressure on a continuous basis in the airways so that air flow is continuously supplied to the body. This CPAP technique is safe for children.
- Removal of tonsils, that is, denotonsillectomy , is used for pathology and diseases of the ENT organs.
- Positional therapy , that is, treatment by changing body position .
- Surgical treatment vulopalatopharyngoplasty. Its purpose is to widen the airways when soft tissue is partially removed.
Purpose of research
Comparison of respiratory rate with standards is required to assess the development of the respiratory system and heart function. A change in indicators in any direction may indicate the presence of pathology (infectious and non-infectious in nature).
Timely identification of developmental deviations increases the likelihood of a child’s complete recovery, without the development of complications. If the measurements were taken over several days, then they need to be shown to the pediatrician. The data will allow you to make a diagnosis faster.
Preventive measures
To prevent breath holding, it is important to follow these rules:
- The room needs regular ventilation.
- It is very important to treat colds to the end.
- During routine examinations, tell the pediatrician the nuances of your child’s well-being, and also tell him in detail about his complaints. If necessary, the doctor will write a referral for Doppler testing.
Remember that only a doctor can correctly assess the condition of the airways, blood vessels and heart.
Norms of breathing rate in newborns
Newborns have the highest respiratory rates. Moreover, in premature babies, a reduced range may be important due to the irregularity of inhalations and exhalations. Deviations from the norm can only be determined by a pediatrician.
The permissible range of breathing rates in children under one year of age:
| Age parameter | Number of breathing movements in 1 minute | |
| Full-term babies | Premature | |
| From birth to 14 days | 40-60 | 20-80 |
| From 15 days to 3 months | 40-45 | 35-50 |
| From 3 to 6 months | 30-40 | 35-45 |
| Over 6 months and up to a year | 30-35 | 30-35 |
By the age of one year, the range of respiratory rates in full-term and premature infants narrows. In children born prematurely, breathing stops for 10-15 seconds, which is considered normal, if there is no blueness of the extremities and there is no developmental disorder of the child. If there are deviations, an urgent examination by a pediatrician is necessary.
Norms of respiratory rate in children by age during wakefulness
The respiratory rate in children (the norm by age presented in the table does not take into account the characteristics of the child’s condition) gradually decreases until the child reaches 18 years of age. Since the lungs are fully expanded (over the entire chest), the condition of the nasal passages changes and the child learns to breathe through the mouth.
Respiratory rate indicators for children from one to 18 years of age:
| Age Ranges | Minimum number of breaths per minute | Maximum number of breaths per minute |
| From 1 year to 2 years | 30 | 35 |
| From 2 to 3 years | 25 | 35 |
| From 3 to 4 years | 25 | 30 |
| From 4 to 5 years | 20 | 30 |
| From 5 to 7 years | 20 | 25 |
| From 7 to 10 years | 18 | 25 |
| From 10 to 14 years old | 18 | 20 |
| From 14 to 18 years old | 16 | 20 |
When measuring the frequency of inhalations and exhalations yourself, it is recommended to pay attention to the depth of inhalations.
If your breathing is shallow, then it will naturally become more frequent to replenish the oxygen deficiency. If a child breathes deeply, but often, this signals the development of pathology. An examination of the pulmonary and cardiovascular systems is necessary.
Leukocyte formula
Let's look at the leukocyte count in children under 5 years of age. Many modern parents prefer to take blood tests in specialized laboratories, which deliver the results directly or send them by email. Having received the data, moms and dads begin to analyze the numbers, compare them with reference values and sometimes panic.
Don't worry ahead of time. In infants, the leukocyte formula is somewhat different from the same formula in adulthood. As in previous cases, this is explained by the fact that the child’s body is in the development stage.
MedVedik encourages you to trust the interpretation of test results to professionals.
The number of leukocyte cells is constantly changing; for this purpose, a leukocyte formula was created, which helps doctors assess the general condition of the patient and promptly identify this or that abnormality. The norms for the content of different bodies belonging to the group of leukocytes vary depending on age. The number of some cells increases, while others decrease, even with normal development. At certain moments, the number of different leukocytes equalizes. Experts call all this a crossover of the formula and do not classify it as a pathology. Most often, crossover occurs during the first year of a child’s life.
Our clinic is ready to advise you on all questions that may arise.
How often should babies breathe in their sleep?
Indicators of the rhythm and frequency of breathing during night sleep differ from the values at the time of wakefulness. Infants, during rest, may experience periodic breathing (discussed below) or apnea (stopping breathing for 10-15 seconds with a frequency of repetitions of at least 15 times within 1 hour).
At the moment of sleep, the whole body rests (muscles and nervous system relax, heart rate slows down), as a result, oxygen consumption decreases, as a result, the frequency and depth of inhalations and exhalations decreases. If you are in doubt whether the child is breathing or not, you can determine the presence of breaths by the rise and fall of the ribs or peritoneum.
It is not recommended to wake up the child every 5-10 minutes. This will harm his nervous system.
In the presence of apnea in premature infants, parents are advised to monitor the rhythm of breathing. Sometimes the baby cannot resume the breathing process during sleep due to muscle relaxation. It is recommended to wake the child, if there is no reaction, urgently call emergency help , and additionally take the necessary measures to restore the respiratory process.
As you grow older, the rhythm and frequency of breathing during sleep stabilizes. In rare cases, these deviations are observed in adults.
Arterial pressure
Blood pressure (BP) is one of the few health markers that can be measured at home. Today, almost every family has a device for independently measuring blood pressure. But not all adults know that the norm for children differs from the “120 to 80” we are all used to.
MedVedik reminds that blood pressure depends on the age of the baby. The younger the child, the lower his normal blood pressure. This is due to the fact that the child’s circulatory system and heart continue to develop after birth, so initially the child’s blood vessels and capillaries have less tone than those of adults.
Keep this helpful sign with BP limits for children. These are generalized indicators that are the result of many years of research. They correspond to the working pressure of 95% of healthy children.
Have you noticed a significant discrepancy in the child’s blood pressure readings and in the table? This is already a reason to see a doctor. He will calculate an individual rate specifically for your child and, if necessary, select treatment.
PS By the way, to obtain an accurate measurement result, the size of the tonometer cuff is important. A large cuff on a small child's hand may distort the readings somewhat.
Causes of decreased breathing rate
Factors that reduce the frequency of inhalation and exhalation can be natural or pathological:
| Natural processes | Pathological processes |
| Frequent attacks of apnea. | Injuries in the chest area. Perhaps damage to the lung tissue, or due to a bruise, the breathing process may be accompanied by severe pain, which will interfere with the normal breathing rhythm. |
| Strong relaxation of the respiratory muscles during sleep. | Damage to brain cells responsible for the respiratory reflex. |
| Physiological feature of the body (rare breathing rate). | The presence of a foreign object in the respiratory tract. |
| Formation of the pulmonary system as the child grows up. | Damage or inflammation of the nerve cells that regulate the frequency of inhalation and exhalation. |
| Temperature drop | Violation of the condition or functioning of the bronchi. |
| Side effects from taking medications. | |
| Electric shock may slow down your breathing. | |
| Poor blood supply, swelling or tumor formations in the brain affecting the functioning of the respiratory system. | |
| Spinal injury. There may be a disruption of the nerve cells that regulate the performance of the muscle tissue responsible for respiratory contractions. | |
| Severe poisoning of the body with poisons. There is a malfunction in the functioning of all organs and systems. | |
| Atrophy of muscle tissue as a result of paralysis or prolonged muscle inactivity. | |
| Curvature of the spine or rickets with subsequent deformation of the chest. | |
| Pathological processes in the cardiovascular system. |
Video on what to do if a child is holding his breath:
Whether a violation of the breathing process is a pathology or a natural process can be determined through regular monitoring of the child and a full examination by a pediatrician and pulmonologist.
What does rapid breathing in children mean?
The frequency of inhalation and exhalation may deviate upward from age-related norms, also due to the influence of natural and pathological factors. This pathology occurs more often in children, since they cannot yet regulate the breathing process normally.
| Natural processes | Pathological processes |
| The air is too dry, hot, rarefied (found in the mountains). | Having a runny nose. Congestion and swelling of the nasal passages occurs. As a result, the child is forced to perform frequent breathing processes through the mouth. |
| Exercising and brisk walking. | Bronchial diseases. As a result, oxygen supply to tissues deteriorates. The brain sends signals to increase the breathing rate. |
| Excitement, fear or crying in a child. | Increased body temperature due to infection. |
| Clogged nasal passages with crusts of waste mucus. | Impaired functioning of brain cells due to injury, the presence of a tumor, or impaired blood supply. |
| Heavy weight of the child. For the normal functioning of all organs, more oxygen is required. | Tumor formations (of any nature) in the respiratory system. |
| Individual features of the functioning of the pulmonary system. | Chest injury. The pain prevents you from taking deep breaths, as a result the child switches to frequent, shallow breathing. |
| Overheating of the body | Impaired functioning of the cardiovascular system. Due to poor blood circulation, the body lacks oxygen. The brain sends signals to increase it (respiration rate increases). |
| Colic in the digestive tract. The pain does not allow me to breathe deeply. Less painful frequent and shallow breathing. | |
| Disruption of the functioning of the nervous system, areas responsible for the rhythm and depth of breathing. | |
| Presence of bronchial asthma. | |
| Due to the action of allergens. | |
| Increased levels of toxins or poisoning from poisons or medications. | |
| Side effects of drugs. | |
| Lack of iron in the blood. As a result, in order to sufficiently supply tissues with oxygen, the respiratory rate increases. |
Respiratory rate in children: the norm should be checked by a pediatrician during a monthly examination and compared with indicators according to the child’s age
In the absence of natural factors affecting the respiratory process, the child must be examined by a pediatrician.
What is periodic breathing, is it dangerous?
Periodic disturbances in the rhythm and depth of breathing are possible in 4 types:
- Cheyne-Stokes. This type is characterized by initially rare and shallow breathing with a gradual increase in inhalation amplitude and depth. When the maximum threshold is reached, the frequency and depth of inspiration gradually decreases, after which an interval of up to 1.5 minutes is possible. Then the process is repeated.
- Biotta. Rhythmic breathing is interrupted by pauses of 30 seconds or more.
- Kussmaul. The breathing process is accompanied by deep but rare breaths and accompanied by noise.
- Grocco. Breathing occurs according to the Cheyne-Stokes type, but instead of pauses there is shallow, weak breathing.
These types of respiratory processes cause harm to both adults and children:
- in children there is a disruption in the development of the respiratory system;
- Oxygen starvation of tissues and organs periodically occurs, which affects their performance. This is a decrease in the functioning of the brain, cardiovascular and nervous systems;
- the development of pathologies in these systems is possible, as well as deterioration of hearing, vision and the presence of constant headaches;
- there is a regular feeling of weakness. At the peak of rapid breathing, loss of consciousness is possible due to an excess of oxygen. At the peak of low breathing, fainting is possible due to lack of oxygen;
- Metabolic processes are disrupted, which leads to a delay in the child’s development (mental, weight and physical).
If pathological breathing is detected in a newborn or an older child, it is recommended to contact a pediatrician for an examination. The specialist will also explain how to behave to parents during prolonged respiratory arrest and the rules for emergency care before the ambulance arrives.
Relationship between breathing rate and heart rate
Respiratory rate in children (the norm by age is often measured together with the heart rate) and heart rate at rest:
| Age indicator | Range of values | |
| Breathing frequencies | Heart rates | |
| From birth to 14 days | 40-60 | 110-160 |
| From 15 days to 3 months | 40-45 | 135-160 |
| From 3 to 6 months | 30-40 | 130-140 |
| Over 6 months and up to a year | 30-35 | 105-155 |
| From 1 year to 2 years | 30-35 | 100-150 |
| From 2 to 3 years | 25-35 | 95-150 |
| From 3 to 4 years | 25-30 | 90-145 |
| From 4 to 5 years | 20-30 | 85-130 |
| From 5 to 7 years | 20-25 | 80-125 |
| From 7 to 10 years | 18-25 | 70-115 |
| From 10 to 14 years old | 18-20 | 65-105 |
| From 14 to 18 years old | 16-20 | 60-95 |
When the heart rate changes, the breathing process is disrupted and vice versa.
Rapid and slow breathing with a normal pulse
An increase or decrease in the respiratory rate value with normal pulse values is possible with the following deviations:
- individual physiological characteristics of the child’s body;
- poor indoor air quality (hot, dry, polluted);
- age-related changes in the child’s body;
- the presence of colic in the digestive tract;
- clogging of the respiratory tract (dried mucus).
These causes are not pathological in nature and go away on their own, without medical intervention. If in doubt, you should be examined by a pediatrician.
With an accelerated heart rate
An increase in the number of heart contractions is accompanied by a change in breathing rate.
Factors causing the violation:
- physical activity, running, as well as stress, fear or increased anxiety;
- increased body temperature due to overheating;
- disruption of the cardiovascular and respiratory systems;
- when an infection enters the body;
- severe poisoning by toxins and poisons;
- side effects from taking medications;
- development of oncology;
- presence of internal or external bleeding;
- entry of a foreign object into the respiratory tract. The body prevents normal breathing, and due to fear, the heart rate increases.
These symptoms (increased or decreased respiratory rate along with an increase in the number of heartbeats) require contact with specialists (pediatrician, pulmonologist, cardiologist) for examination.
With a slow heartbeat
When the heart beats slow down, the breathing process is disrupted in the following cases:
- pathological processes in the cardiovascular system;
- disruption of brain cell activity;
- electric shock;
- when the body is hypothermic;
- the effect of infection;
- side effect from taking medications.
Reduced heart rate and respiration rates are observed in children involved in sports. If a child does not engage in sports activities, then a change in indicators means the development of pathologies. An examination is required.
Pneumonia among all pulmonary pathologies in young children is almost 80%. Even with the introduction of progressive technologies in medicine - the discovery of antibiotics, improved diagnostic and treatment methods - this disease is still one of the ten most common causes of death. According to statistical data in various regions of our country, the incidence of pneumonia in children is 0.4-1.7%.
- Improper treatment of influenza and ARVI can lead to pneumonia in a child
- Pneumonia in children - differential diagnosis of ARVI, acute bronchitis and bronchiolitis
- Signs of pneumonia in a child. Symptoms of pneumonia in infants, children under one year old
- Chlamydial, mycoplasma pneumonia in a child
- Indications for hospitalization
- Treatment of pneumonia in a child
When and why can pneumonia occur in a child?
The lungs perform several important functions in the human body. The main function of the lungs is gas exchange between the alveoli and the capillaries that envelop them.
Simply put, oxygen from the air in the alveoli is transported into the blood, and carbon dioxide from the blood enters the alveoli.
They also regulate body temperature, regulate blood clotting, are one of the filters in the body, promote cleansing, the removal of toxins, breakdown products that occur during various injuries, and infectious inflammatory processes. And in the event of food poisoning, burns, fractures, surgical interventions, or any serious injury or illness, a general decrease in immunity occurs, and it is more difficult for the lungs to cope with the load of filtering toxins.
That is why very often a child develops pneumonia after suffering or against the background of injuries or poisoning.
Most often, the causative agent of the disease is pathogenic bacteria - pneumococci, streptococci and staphylococci, and recently cases of the development of pneumonia from pathogens such as pathogenic fungi, legionella (usually after staying in airports with artificial ventilation), mycoplasma, chlamydia, which are not They are rarely mixed or associated.
Pneumonia in a child, as an independent disease that occurs after serious, severe, prolonged hypothermia, is extremely rare, since parents try to prevent such situations.
As a rule, in most children, pneumonia does not occur as a primary disease, but as a complication after ARVI or influenza, less often than other diseases.
Why is this happening?
Many of us believe that acute viral respiratory diseases have become more aggressive and dangerous due to their complications in recent decades. This may be due to the fact that both viruses and infections have become more resistant to antibiotics and antiviral drugs, which is why they are so severe in children and cause complications.
One of the factors in the increase in the incidence of pneumonia in children in recent years has been the general poor health of the younger generation - how many children today are born with congenital pathologies, developmental defects, and lesions of the central nervous system.
A particularly severe course of pneumonia occurs in premature or newborn babies, when the disease develops against the background of an intrauterine infection with an insufficiently formed, immature respiratory system.
In congenital pneumonia, the causative agents are often herpes simplex virus, cytomegalovirus, mycoplasma, and when infected during childbirth - chlamydia, group B streptococci, opportunistic fungi, Escherichia coli, Klebsiella, anaerobic flora; when infected with hospital infections, pneumonia begins on the 6th day or 2 weeks after birth.
Naturally, pneumonia most often occurs in cold times, when the body already undergoes a seasonal adjustment from heat to cold and vice versa, overloads occur for the immune system, at this time there is a lack of natural vitamins in foods, temperature changes, damp, frosty, windy weather contribute to hypothermia of children and their infection.
In addition, if a child suffers from any chronic diseases - tonsillitis, adenoids in children, sinusitis, dystrophy, rickets (see rickets in an infant), cardiovascular disease, any severe chronic pathologies, such as congenital lesions of the central nervous system, developmental defects, immunodeficiency states - significantly increase the risk of developing pneumonia and aggravate its course.
The severity of the disease depends on:
- Extensiveness of the process (focal, focal-confluent, segmental, lobar, interstitial pneumonia).
- The age of the child, the younger the baby, the narrower and thinner the airways, the less intense gas exchange in the child’s body and the more severe the course of pneumonia.
- Places where and for what reason pneumonia occurred:
— community-acquired: most often have a milder course
— hospital: more severe, since infection with bacteria resistant to antibiotics is possible
- aspiration: when foreign objects, mixture or milk enter the respiratory tract.
The most important role is played by the general health of the child, that is, his immunity.
Improper treatment of influenza and ARVI can lead to pneumonia in a child
When a child gets sick with a common cold, acute respiratory viral infection, or influenza, the inflammatory process is localized only in the nasopharynx, trachea and larynx.
If the immune response is weak, and also if the pathogen is very active and aggressive, and the child is treated incorrectly, the process of bacterial reproduction descends from the upper respiratory tract to the bronchi, then bronchitis may occur. Further, inflammation can also affect lung tissue, causing pneumonia.
What happens in a child’s body during a viral disease?
In most adults and children, various opportunistic microorganisms - streptococci, staphylococci - are always present in the nasopharynx, without causing harm to health, since local immunity inhibits their growth.
However, any acute respiratory disease leads to their active reproduction, and if the parents act correctly during the child’s illness, the immune system does not allow their intensive growth.
What should not be done during ARVI in a child to avoid complications:
Antitussives should not be used.
Coughing is a natural reflex that helps the body clear the trachea, bronchi and lungs of mucus, bacteria, and toxins. If, to treat a child, in order to reduce the intensity of a dry cough, you use antitussives that affect the cough center in the brain, such as Stoptusin, Bronholitin, Libexin, Paxeladin, then an accumulation of sputum and bacteria in the lower respiratory tract may occur, which ultimately leads to pneumonia.
You cannot carry out any preventive antibiotic therapy for colds or viral infections.
Antibiotics are powerless against the virus, but the immune system must cope with opportunistic bacteria, and their use is indicated only if complications arise as prescribed by a doctor.
The same applies to the use of various nasal vasoconstrictors; their use promotes faster penetration of the virus into the lower respiratory tract, therefore Galazolin, Naphthyzin, Sanorin are not safe to use for a viral infection.
Drinking plenty of fluids - one of the most effective methods of relieving intoxication, thinning mucus and quickly clearing the airways is drinking plenty of fluids, even if the child refuses to drink, parents should be very persistent.
If you do not insist that the child drinks a sufficiently large amount of liquid, there will also be dry air in the room - this will help dry out the mucous membrane, which can lead to a longer course of the disease or a complication - bronchitis or pneumonia.
Constant ventilation, the absence of carpets and rugs, daily wet cleaning of the room in which the child is located, humidification and purification of the air using a humidifier and air purifier will help to quickly cope with the virus and prevent pneumonia from developing. Because clean, cool, moist air helps to thin sputum, quickly eliminate toxins through sweat, cough, and wet breath, which allows the child to recover faster.
Acute bronchitis and bronchiolitis - differences from pneumonia
ARVI usually has the following symptoms:
- High temperature in the first 2-3 days of illness (see antipyretics for children)
- Headache, chills, intoxication, weakness
- Qatar of the upper respiratory tract, runny nose, cough, sneezing, sore throat (not always the case).
In case of acute bronchitis against the background of acute respiratory viral infection, the following symptoms may occur:
- Slight increase in body temperature, usually up to 38C.
- At first the cough is dry, then it becomes wet, there is no shortness of breath, unlike pneumonia.
- Breathing becomes harsh, various scattered wheezes appear on both sides, which change or disappear after coughing.
- The radiograph shows an increase in the pulmonary pattern, and the structure of the roots of the lungs decreases.
- There are no local changes in the lungs.
Bronchiolitis occurs most often in children under one year of age:
- The difference between bronchiolitis and pneumonia can only be determined by X-ray examination, based on the absence of local changes in the lungs. According to the clinical picture, acute symptoms of intoxication and an increase in respiratory failure, the appearance of shortness of breath - are very similar to pneumonia.
- With bronchiolitis, the child’s breathing is weakened, shortness of breath with the participation of auxiliary muscles, the nasolabial triangle becomes bluish, general cyanosis and severe pulmonary heart failure are possible. When listening, a boxy sound and a mass of scattered fine-bubble rales are detected.
Signs of pneumonia in a child
When the infectious agent is highly active, or when the body’s immune response to it is weak, when even the most effective preventive treatment measures do not stop the inflammatory process and the child’s condition worsens, parents can guess from some symptoms that the child needs more serious treatment and urgent medical examination.
At the same time, under no circumstances should you start treatment with any traditional method. If it really is pneumonia, not only will this not help, but the condition may worsen and time will be lost for adequate examination and treatment.
Symptoms of pneumonia in a child 2 - 3 years old and older
How can attentive parents determine if they have a cold or viral illness that they should urgently call a doctor and suspect pneumonia in their child?
Symptoms that require x-ray diagnostics:
- After an acute respiratory infection or flu, there is no improvement in the condition for 3-5 days, or after a slight improvement, a jump in temperature and increased intoxication and cough reappear.
- Lack of appetite, lethargy of the child, sleep disturbances, and moodiness persist for a week after the onset of the illness.
- The main symptom of the disease remains a severe cough.
- The body temperature is not high, but the child has shortness of breath. At the same time, the number of breaths per minute in a child increases, the norm of breaths per minute in children aged 1-3 years is 25-30 breaths, in children 4-6 years old - the norm is 25 breaths per minute, if the child is in a relaxed, calm state. With pneumonia, the number of breaths becomes greater than these numbers.
- With other symptoms of a viral infection - cough, fever, runny nose - pronounced pallor of the skin is observed.
- If the temperature is high for more than 4 days and antipyretics such as Paracetamol, Efferalgan, Panadol, Tylenol are not effective.
Symptoms of pneumonia in infants, children under one year old
The mother can notice the onset of the disease by changes in the baby’s behavior. If a child constantly wants to sleep, becomes lethargic, apathetic, or vice versa, is capricious a lot, cries, refuses to eat, and the temperature may rise slightly, the mother should immediately consult a pediatrician.
Body temperature
In the first year of life, pneumonia in a child, the symptom of which is considered to be a high, unbroken temperature, is distinguished by the fact that at this age it is not high, does not reach 37.5 or even 37.1-37.3.
However, temperature is not an indicator of the severity of the condition.
The first symptoms of pneumonia in an infant
This is causeless anxiety, lethargy, loss of appetite, the baby refuses to breastfeed, sleep becomes restless, short, loose stools appear, there may be vomiting or regurgitation, runny nose and paroxysmal cough, which intensifies while the baby is crying or feeding.
Baby's breathing
Chest pain when breathing and coughing.
Sputum - with a wet cough, purulent or mucopurulent sputum (yellow or green) is released.
Shortness of breath or an increase in the number of breathing movements in young children is a clear sign of pneumonia in a child. Shortness of breath in infants may be accompanied by nodding of the head in time with breathing, and the baby also puffs out his cheeks and stretches out his lips, sometimes foamy discharge appears from the mouth and nose.
A symptom of pneumonia is considered to be exceeding the normal number of breaths per minute:
- In children under 2 months, the norm is up to 50 breaths per minute; over 60 is considered a high frequency.
- In children from 2 months to a year, the norm is 25-40 breaths, if 50 or more, then this is exceeding the norm.
- In children older than one year, the number of breaths exceeding 40 is considered shortness of breath.
Skin texture changes when breathing
Attentive parents may also notice retraction of the skin when breathing, usually on one side of the diseased lung.
To notice this, you should undress the baby and observe the skin between the ribs; it retracts when breathing. With extensive lesions, one side of the lung may lag behind during deep breathing.
Sometimes you can notice periodic stops in breathing, disturbances in the rhythm, depth, frequency of breathing, and the child’s desire to lie on one side.
Cyanosis of the nasolabial triangle
This is the most important symptom of pneumonia, when blue skin appears between the baby’s lips and nose. This sign is especially pronounced when the baby is breastfeeding.
With severe respiratory failure, slight blue discoloration may appear not only on the face, but also on the body.
Chlamydial, mycoplasma pneumonia in a child
Among pneumonias, the causative agents of which are not common bacteria, but various atypical representatives, mycoplasma and chlamydial pneumonia are distinguished.
In children, the symptoms of such pneumonia are somewhat different from the course of ordinary pneumonia. Sometimes they are characterized by a hidden, sluggish course.
Signs of atypical pneumonia in a child may be as follows:
- The onset of the disease is characterized by a sharp rise in body temperature to 39.5 C, then a persistent low-grade fever forms -37.2-37.5 or even normalization of temperature occurs.
- It is also possible that the disease begins with the usual signs of ARVI - sneezing, sore throat, severe runny nose.
- Persistent dry debilitating cough, shortness of breath may not be constant. This cough usually occurs with acute bronchitis, not pneumonia, which complicates the diagnosis.
- When listening, the doctor is most often presented with scant data: rare wheezing of various sizes, pulmonary percussion sound. Therefore, it is difficult for a doctor to determine atypical pneumonia based on the nature of wheezing, since there are no traditional signs, which greatly complicates the diagnosis.
- There may be no significant changes in the blood test for SARS. But usually there is an increased ESR, neutrophilic leukocytosis, combination with anemia, leukopenia, eosinophilia.
- A chest x-ray reveals a pronounced increase in the pulmonary pattern and heterogeneous focal infiltration of the pulmonary fields.
- Both chlamydia and mycoplasma have the ability to exist for a long time in the epithelial cells of the bronchi and lungs, so most often pneumonia is of a protracted, recurrent nature.
- Treatment of atypical pneumonia in a child is carried out with macrolides (azithromycin, josamycin, clarithromycin), since the pathogens are most sensitive to them (to tetracyclines and fluoroquinolones, too, but they are contraindicated for children).
Indications for hospitalization
The decision about where to treat a child with pneumonia - in a hospital or at home - is made by the doctor, and he takes into account several factors:
The severity of the condition and the presence of complications - respiratory failure, pleurisy, acute disturbances of consciousness, heart failure, drop in blood pressure, lung abscess, pleural empyema, infectious-toxic shock, sepsis.
Damage to several lobes of the lung. Treatment of focal pneumonia in a child at home is quite possible, but for lobar pneumonia it is better to treat it in a hospital setting.
Social indications are poor living conditions, inability to carry out care and doctor’s orders.
Age of the child - if an infant falls ill, this is grounds for hospitalization, since pneumonia in an infant poses a serious threat to life. If pneumonia develops in a child under 3 years of age, treatment depends on the severity of the condition and most often doctors insist on hospitalization. Older children can be treated at home, provided that the pneumonia is not severe.
General health - in the presence of chronic diseases, weakened general health of the child, regardless of age, the doctor may insist on hospitalization.
Treatment of pneumonia in a child
Antibiotics are the mainstay of treatment for pneumonia. At a time when doctors did not have antibiotics in their arsenal for bronchitis and pneumonia, pneumonia was a very common cause of death in adults and children, so in no case should you refuse to use them; no folk remedies are effective for pneumonia.
Parents are required to strictly follow all the doctor’s recommendations, provide proper care for the child, adhere to the drinking regime, nutrition:
Taking antibiotics must be carried out strictly on time; if the drug is prescribed 2 times a day, this means that there should be a break of 12 hours between doses, if 3 times a day, then a break of 8 hours. Antibiotics are prescribed - penicillins, cephalosporins for 7 days, macrolides (azithromycin, josamycin, clarithromycin) - 5 days. The effectiveness of the drug is assessed within 72 hours - improvement in appetite, decrease in temperature, shortness of breath.
Antipyretics are used if the temperature is above 39C , in infants above 38C. At first, antipyretic antibiotics are not prescribed, since it is difficult to assess the effectiveness of therapy. It should be remembered that during high temperatures the body produces the maximum amount of antibodies against the pathogen, so if a child can tolerate a temperature of 38C, it is better not to knock it down. This way the body can quickly cope with the microbe that caused pneumonia in the baby. If a child has had at least one episode of febrile convulsions, the temperature should be brought down already at 37.5C.
Feeding a child with pneumonia - lack of appetite in children during illness is considered natural and the child’s refusal to eat is explained by the increased load on the liver when fighting the infection, so you cannot force feed the child. If possible, you should prepare light food for the patient, exclude any ready-made chemicalized foods, fried and fatty, try to feed the child simple, easily digestible food - porridge, soups with a weak broth, steamed cutlets from lean meat, boiled potatoes, various vegetables, fruits.
Oral hydration - in water, natural freshly squeezed diluted juices - carrot, apple, weakly brewed tea with raspberries, rosehip infusion, water-electrolyte solutions are added (Rehydron, etc.).
Ventilation, daily wet cleaning, and the use of air humidifiers alleviate the baby’s condition, and the love and care of parents works wonders.
No general tonic (synthetic vitamins), antihistamines, or immunomodulators are used, since they often lead to side effects and do not improve the course and outcome of pneumonia.
Taking antibiotics for pneumonia in a child (uncomplicated) usually does not exceed 7 days (macrolides 5 days), and if you follow bed rest, follow all the doctor’s recommendations, in the absence of complications, the child will quickly recover, but within a month there will still be residual effects in the form cough, slight weakness.
With atypical pneumonia, treatment may take longer. P
When treated with antibiotics, the intestinal microflora in the body is disrupted, so the doctor prescribes probiotics - RioFlora Immuno, Acipol, Bifiform, Bifidumbacterin, Normobact, Lactobacterin.
To remove toxins after completion of therapy, the doctor may prescribe sorbents such as Polysorb, Enterosgel, Filtrum.
If the treatment is effective, the child can be transferred to a general regimen and walks from the 6-10th day of illness, and hardening can be resumed after 2-3 weeks.
In case of mild pneumonia, heavy physical activity (sports) is allowed after 6 weeks, in case of complicated pneumonia after 12 weeks.
Source: https://zdravotvet.ru/
Dependence of breathing rate on body temperature
The respiratory rate in children (the norm for age is a conditional indicator, since in diseases and certain characteristics of the body, breathing is often rapid or slow) depends on body temperature.
Until the child reaches 2 months, with an increase in temperature, only an increase in the respiratory rate occurs, the heartbeat remains normal. After the child reaches 2 months, both indicators increase. This reaction of the body is due to the protective and regenerative reaction of the body.
How to normalize your breathing rate
To restore breathing rate you need:
- during the period of night rest, take a horizontal position on your back, but at the time of an attack it is not recommended to put the child on your back;
- change your diet by increasing the amount of fresh vegetables and fruits;
- perform breathing exercises with the child for 15-20 minutes 3 times a day (slowly inhale through the nose, exhale through the mouth);
- in a playful way, breathe with the child into the bag and inflate the balloons;
- if the attack is caused by fear or stress, then you need to give children's sedatives or herbal decoctions;
- in the absence of breathing (during a prolonged attack of apnea), you need to rouse the child, let him smell ammonia (carefully so as not to burn the nasal mucosa). Sometimes it is recommended to hold the baby upside down for 1-3 minutes. In this case, you need to spank the baby on the buttocks. After this, splash the child’s face with cold water or wash it.
If the breathing rate is severely impaired, emergency assistance must be called.
Medicines, except for sedatives in liquid form, should not be given to a child until the symptoms are eliminated and the cause is determined. Normalization of the frequency of inhalation and exhalation in children varies by age towards a decrease in the indicator. If there are deviations, it is recommended to contact a pediatrician to determine the cause of the breathing disorder. Self-medication is unacceptable.
Author: Kotlyachkova Svetlana
Article design: E. Chaikina