Let's find out what ESR is, what is the norm in children, and should we worry if the criterion deviates?
The normal erythrocyte sedimentation rate (ESR) is a laboratory criterion determined during a general blood test in children. The need for determination is due to its high sensitivity to any pathological changes in the child’s body. However, ESR is characterized by extremely low specificity and cannot be used as the main diagnostic test.
This is due to the fact that the level of ESR can increase with autoimmune pathologies, infectious diseases, post-traumatic conditions, severe stress, etc.
What does ESR mean?
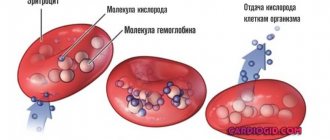
Due to their negative charge, red blood cells (erythrocytes) repel each other and do not stick together. When the immune system is activated, active synthesis of protective proteins begins: blood clotting factor I and immunoglobulins of various classes. Both factors influence ESR and act as a connecting “bridge” for red blood cells.
As a result, the process of red blood cell clumping is activated. The resulting aggregates of red blood cells are much heavier than individual cells and settle faster in the liquid medium of the blood.
Thus, the presence of specific proteins is the first sign of activation of the immune response to infection or internal pathologies, and an increase in ESR is additional confirmation of this process.
On what factors does a child’s ESR depend?
The ESR indicator in children is extremely sensitive to many external and internal factors. Among them, the quantitative content of protective specific proteins in the bloodstream that respond to infectious microorganisms and tumor neoplasms.
An increase in low-density lipoproteins (“bad cholesterol”), the bile pigment bilirubin and bile acids also has an effect. In this case, there is a significant increase in ESR.
The main causes of increased erythrocyte sedimentation rate are infectious diseases, tumors and autoimmune inflammatory processes.
ESR: what is it?
ESR and ROE - erythrocyte sedimentation reaction are the same, but the latter abbreviation is considered outdated. ESR shows the intensity of red blood cell aggregation followed by their sedimentation to the bottom.
The clumping of red blood cells is enhanced in the presence of the protein fibrinogen, which is involved in the formation of blood clots and is normally practically absent in plasma. A decrease in the largest fraction of proteins - albumin and an increase in numerous protein fractions of globulins - gamma, beta and alpha changes the ESR towards an increase.
The sedimentation rate will certainly change if the erythrocyte has an abnormal shape and non-standard size, which is typical for anemia of various etiologies, including those caused by complications of chemotherapy.
Any pathological process - infection, inflammation, tumor, especially a malignant blood disease, affects the ratio of blood proteins and, of course, can shift the indicator in one direction or another.
How to take an ESR test for children?
The accuracy and reliability of the result depends on how correctly the preanalytical stage (preparation and collection of biomaterial) is implemented. According to statistics, on average, more than 70% of errors are made at this stage. The consequence is the need for a repeat blood test, and the procedure for taking biomaterial is unpleasant for children.
Biomaterial for ESR analysis:
- venous blood taken from the cubital vein on the child’s elbow;
- capillary blood that collects from the baby’s ring finger or heel.
Venous blood is collected using a sterile vacuum system and a butterfly needle, which significantly speeds up and makes the procedure as safe as possible. The advantage of a vacuum system: no contact of blood with the external environment and minimal risk of hemolysis (destruction of red blood cells in a test tube), which makes analysis impossible.
Capillary blood is collected using a scarifier with a needle stop. Modern scarifiers for children control the depth of needle insertion and automatically hide the blade after a puncture, making it impossible to reuse.
After the puncture, the first drop of blood is removed with a clean cotton swab, and collection begins with the second drop. This technique allows you to prevent random impurities from entering the test tube. Special pressure or squeezing of the child’s finger should be avoided, which can lead to distortion of the analysis result.
Preference should be given to venous blood, since the risk of premature clotting or hemolysis is significantly reduced compared to capillary blood.
How to prepare a child for analysis?
The collection of biomaterial is carried out in the morning, preferably on an empty stomach. For infants, a minimum interval after the last meal of 2 hours is allowed, for children under 5 years old - 5-6 hours, for older patients it is necessary to wait at least 8 hours.
Important: to facilitate blood collection, the child should be given unsweetened water. This will make the blood less viscous and reduce the risk of false results.
It is important that the child is in a calm state. If possible, it should be explained that the procedure will not cause harm and is necessary for his health, and the unpleasant sensation from the injection is not strong and short-lived.
Read further: Norm of bilirubin in children, maximum deviations in the table
ESR norms in children by age in the table
The results of the blood test must be deciphered by the attending physician, and the information in this section is presented for informational purposes only.
The ESR norm for a child is selected taking into account age. In addition, it is impossible to establish a final diagnosis based on one parameter, so the erythrocyte sedimentation rate is assessed in conjunction with other studies (complete blood count).
The table shows the norm of ESR in the blood of children by age according to the Panchenkov method.
| Age | Acceptable values, mm/h |
| Newborns up to 1 month | 2 – 5 |
| 1 – 12 months | 4 – 10 |
| 15 years | 5 – 10 |
| 5 – 15 years | 2 – 10 |
| Over 15 years old | 2 – 15 |
For example, if the results of a blood test for a 5-year-old child indicate an ESR of 10 mm/h, then this is considered normal.
It should be noted that the normal ESR in a blood test for children is 3, 5, 10, etc. years is identical for both sexes. The indicator has no gender differences. However, in girls during menstruation, the indicator may increase to the upper limits of normal.
Detection of an ESR of 16 mm/h in a child over 15 years of age is considered acceptable. In this case, the analysis should be repeated after a few weeks.
Blood test for ARVI
When a child has a fever, cough and runny nose, parents want to be sure that this is a common ARVI and not a bacterial infection. Sometimes it seems to them that a general blood test will dot the i's - as soon as they take it, it will immediately become clear what the child is sick with and whether they need to give him antibiotics. However, this is not quite true. In some cases, a blood test will actually help the doctor make a diagnosis, but most often it is not necessary. In addition, the result obtained, where half of the indicators go beyond the norm, only needlessly scares parents. Pediatrician Alexandra Zhukovskaya talks about why you shouldn’t rush to get a blood test at the first symptoms of the disease.
What indicators can change during infection?
First of all, the total number of leukocytes changes - these are the cells that protect the body from viruses and bacteria. There are several types of white blood cells that perform different tasks: neutrophils, lymphocytes, monocytes, eosinophils and basophils. Their number and relationship to each other are displayed in the leukocyte formula - usually as a percentage. As soon as one indicator increases slightly, the rest will automatically decrease. This is why, with minor changes in the leukocyte formula, the forms look frighteningly red. In addition, in many laboratories, the forms indicate standards for adults, which differ from children. Thus, in children under 5 years of age, lymphocytes predominate, in older children - neutrophils, and the total number of leukocytes changes with age.
What do deviations mean?
With a bacterial infection, you usually experience:
- increase in the number of leukocytes (leukocytosis) - more than 15 × 10⁹/l;
- increase in the absolute* number of neutrophils - more than 10 × 10⁹/l;
- a shift in the leukocyte formula to the left - that is, the appearance of immature (band) forms of neutrophils - more than 1.5 × 10⁹/l.
*To estimate the absolute neutrophil count, you need to know the total white blood cell count and the percentage of neutrophils. For example: leukocytes are 9 × 10⁹/l, and neutrophils make up 72%, which is usually already highlighted in red. We count: 9 × 72/100%, we get 6.5 - that is, the normal absolute number of neutrophils.
With a viral infection, you usually experience:
- Decrease in the total number of leukocytes (leukopenia) - especially with influenza, measles, etc.
- Increased absolute number of lymphocytes (lymphocytosis).
- The appearance of “atypical” cells occurs in infectious mononucleosis.
Another nonspecific sign of inflammation is an increase in erythrocyte sedimentation rate (ESR). High ESR is typical for both viral and bacterial infections.
What then causes difficulties?
The fact is that in the first days of the disease there may not yet be any characteristic changes in the general blood test, or vice versa - the leukocytes may “jump” significantly even for a banal viral infection, casting doubt on the diagnosis. Many viruses (adenovirus, Epstein-Barr virus) lead to a persistent increase in the number of white blood cells - leukocytosis - which is usually associated with a bacterial infection.
Conversely, some bacterial diseases occur without abnormalities in blood tests - for example, otitis media or atypical pneumonia, or even with changes characteristic of a viral infection - for example, lymphocytosis is observed in whooping cough.
There are quite a few such exceptions, which is why at the beginning of the disease a general blood test cannot be a universal diagnostic method - the doctor will receive much more information during a thorough examination of the child.
How else can you clarify the diagnosis?
If the doctor suspects streptococcal sore throat or influenza, a streptate test or rapid test for influenza is performed. Methods are available to detect many viruses in saliva, nasal secretions, etc. A chest x-ray is indicated to rule out pneumonia. If a urinary tract infection is suspected, urine test strips and urine tests are performed. In case of severe intestinal infections, feces are examined for the presence of bacteria belonging to the intestinal group (salmonellosis, dysentery, etc.). If the child has been feverish for a long time and there is no obvious source of infection, the levels of C-reactive protein and procalcitonin are looked at in a biochemical blood test. Some time after the onset of the disease, specific antibodies against various infectious agents can be detected in the blood.
Isn't it easier to give an antibiotic right away?
No.
- Antibiotics are ineffective against viruses and cannot prevent bacterial complications, but vaccination against pneumococcus and other bacterial infections can cope with this.
- Antibacterial therapy disrupts the vital activity of normal microflora involved in protection against foreign and dangerous microorganisms.
- Taking antibiotics without indications leads to antibiotic resistance—bacterial resistance. This means that the next time an antibiotic is actually needed, it will no longer be harmful to the bacteria, and the disease will be more difficult to cure.
- For some viral infections (for example, infectious mononucleosis), the administration of widely used penicillin antibiotics leads to the appearance of a rash. This is often interpreted as an allergic reaction, although there are no contraindications for further use of this group of antibiotics in a child.
- All medications, including antibacterial drugs, have side effects. The benefit of any intervention should be greater than the potential harm - you should not break this rule by giving antibiotics “just in case”.
Why does ESR increase in children?
The reasons for the increase in the indicator are different, so only a doctor can prescribe treatment.
When collecting a medical history of a small patient, data from laboratory and instrumental research methods, as well as the presence and severity of symptoms of the disease are taken into account. As necessary, the most complete family history of the child is collected, taking into account genetic predisposition to hereditary pathologies.
It should be understood that a slight deviation from the norm has no diagnostic significance. So, if a one-year-old child has an ESR of 11 mm/h, then this is considered acceptable and may indicate a recent infection (the test must be repeated after 2 weeks).
The most common cause of increased ESR is an infectious disease, predominantly of a bacterial nature.
Inflammatory processes of various localizations, burns of varying degrees and mechanical injuries are also among the reasons for deviation of the criterion from the norm.
Also, the level of erythrocyte sedimentation rate may increase if the patient has malignant diseases. A significant excess of the norm is observed in the following oncopathologies:
- multiple myeloma (Rustitsky-Kale disease), localized in the bone marrow. In this case, the value of the criterion reaches critical values. The disease is characterized by excessive production of pathological proteins, leading to the formation of “coin columns” - multiple aggregation of red blood cells;
- Lymphogranulomatosis (Hodgkin's disease) affects people regardless of gender and age. This pathology affects lymphoid tissues. The ESR level is of primary importance not for identifying pathology, but for determining its course and assessing the effectiveness of selected therapeutic methods.
Other malignant neoplasms are also accompanied by an upward deviation from the norm. There is a direct correlation (dependence) between the degree of criterion deviation and the stage of cancer. Thus, the highest ESR values are characteristic of the terminal stage and the spread of metastases to neighboring organs and tissues.
Table of ESR indicators for oncology in men and women
On the Internet you can find tables of changes in ESR for various types of malignant processes separately for women and men. This information could be trusted if the ESR indicator were included in the mandatory criteria for cancer, as we know, most tumor markers produced by cancer cells do not have this honor.
The erythrocyte sedimentation rate in most cancer patients does not deviate from the norm over the period of cancer development. On the eve of death from the progression of a malignant disease, when the volume of the tumor and its aggression are practically incompatible with life, and the function of the most important body systems is reduced to a minimum, the ESR can demonstrate “full health.” A banal respiratory infection, which occurs in the average Russian six times a year, in a radically treated patient without any signs of a malignant process can increase the rate of red blood cell precipitation to 40-60 mm per hour for a month.
With a very small range of oncohematological diseases, ESR may coincide with the progression of the process, but this is not necessary, nor is a decrease in the indicator considered a victory over the tumor.
The interpretation of test changes is individual, and tables of ESR correspondence to certain cancer diseases can be considered a marketing ploy of the site that does not reflect the objective oncological reality.
Reasons for decreased ESR in a child
A low ESR is usually of no clinical significance. Most often, this situation occurs during fasting, low muscle mass, following a vegetarian diet, etc.
In rare cases, a similar situation occurs in the case of a pathological change in the morphology of red blood cells, preventing their deposition. Among them:
- hereditary Minkowski-Choffard disease (spherocytosis), in which hemolysis of red blood cells occurs against the background of genetically determined damage to structural proteins in their membrane;
- Sickle cell anemia is a congenital disease in which red blood cells become elongated.
A variant of the physiological norm is a temporary decrease in the indicator in a child as a result of prolonged diarrhea, dehydration or after vomiting. However, after the body is restored, the ESR value should return to within acceptable limits.