The postpartum period is probably the most beautiful and most awaited time for every woman. Due to the fact that the body undergoes many changes at this stage, the expectant mother should be regularly examined by a specialist.
The most common procedure is a general blood test. One of the most important indicators is platelets during pregnancy.
This examination is necessary for the early detection of abnormalities that are dangerous not only for the woman, but also for her unborn child.
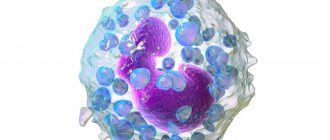
Description of cells
Platelets are very thin discs that help blood clot. Their peculiarity is the ability to stick together when a cut or wound forms.
As a result of this process, clots are formed that block the blood vessels and prevent large amounts of blood from leaking out. Against this background, a crust appears on the surface of the skin. If it is removed, bleeding may resume.
In addition, platelets perform a protective function, protecting the body from the penetration of pathogenic bacteria and viruses.
They contribute to the formation of the immune system and are regularly updated.
The number of platelets in the blood is a temporary indicator. It is constantly changing depending on the influence of internal and external factors. For example, it changes during pregnancy and during the menstrual cycle.
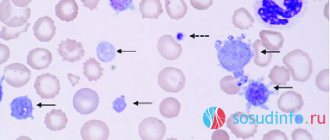
Platelet count (according to Fonio)
Platelets are involved in the entire process of blood coagulation, starting from the formation of a primary thrombus in the area of damage to blood vessels and ending with participation in the processes of regulating vascular permeability and tone.
The calculation of the most accurate number of platelets is carried out using the Goryaev camera and the Fonio method. The Fonio platelet count is quite accurate. The Fonio method is most convenient for automatic counting.
Units
In a stained smear, 1000 red blood cells and all platelets found are counted. The result is a number expressed in ppm. To obtain the absolute number of platelets, a clinical laboratory diagnostics physician multiplies this value by the number of red blood cells present in 1 μl, and then divides by 1000.
What biomaterial can be used for research?
Venous, capillary blood.
How to properly prepare for research?
- Eliminate alcohol and medications from your diet (in consultation with your doctor) the day before donating blood.
- Do not eat for 8 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
An important condition for the correct functioning of the coagulation system is the presence of a certain number of mature platelets in the bloodstream. Deviations in any direction can have adverse consequences. The normal platelet count in the blood differs depending on age and gender. If their level is reduced, there is a tendency to bleeding, blood clotting worsens, and is difficult to stop. If the platelet count exceeds the norm, the blood becomes thick, and there is a risk of blood clots and blockage of blood vessels.
Platelets are formed in the bone marrow from giant cells called megakaryocytes. In fact, they are fragments of these cells and are small, nuclear-free, colorless oval or round shaped plates surrounded by a membrane, including granules. The diameter of platelets ranges from 2 to 4 microns. They are usually called blood cells, like leukocytes and red blood cells, although they are not. These are postcellular structures, or Bizzazero plaques (named after the Italian scientist who made a great contribution to their study). About 2/3 of all platelets are found in the blood, the rest are found in the spleen.
Functions of blood platelets
When the vascular wall is damaged, blood platelets are immediately activated. They take on a spherical shape and outgrowths appear on them, making them look like a star. Platelets in their active form are capable of sticking to each other (aggregation) and sticking to the vessel wall (adhesion). They secrete an enzyme into the blood plasma, under the influence of which soluble fibrinogen is converted into insoluble fibrin, which entangles the formed elements of the blood with its threads, like nets. The resulting thrombus closes the defect in the damaged vessel. Platelets take part in the dissolution of the fibrin clot and maintain spasm of damaged vessels. Another important function is to provide nutrients to the cells that line the inner surface of blood vessels.
What do the results mean?
Platelets
| Age | Reference values |
| Less than 10 days | 99 - 421 *10^9/l |
| 10 days – 1 month | 150 – 400 *10^9/l |
| 1-6 months | 180 – 400 *10^9/l |
| 6 months – 1 year | 160 - 390 *10^9/l |
| 1-5 years | 150 – 400 *10^9/l |
| 5-10 years | 180 - 450 *10^9/l |
| 10-15 years | 150 – 450 *10^9/l |
| More than 15 years | 180 - 320 *10^9/l |
Thrombocytopenia
Causes:
- thrombocytopenic purpura/hemolytic-uremic syndrome;
- DIC syndrome (disseminated intravascular coagulation);
- drug thrombocytopenia (co-trimoxazole, procainamide, thiazide diuretics, heparin);
- hypersplenism;
- idiopathic thrombocytopenic purpura.
It should be remembered that in pregnant women, platelets can normally decrease to 75-150×109/l.
Thrombocytosis
Causes:
- Primary thrombocytosis (malignant disease of the myeloid lineage of the bone marrow, including essential thrombocytosis and chronic myeloid leukemia);
- Secondary thrombocytosis after removal of the spleen, during an infectious process, iron deficiency anemia, hemolysis, trauma and malignant diseases (reactive thrombocytosis).
- An increase in Hb, MCV, or total leukocyte count suggests primary thrombocytosis.
The indicator is normal
The platelet count in a pregnant woman is an important indicator that should always be monitored. It may decrease during pregnancy due to an increase in blood volume and the formation of a placental circle of blood flow. The average volume considered normal in pregnant women is about 140-340 thousand/mcL.
This number depends on when you became pregnant. The normal platelet count in the blood is:
- I trimester - 170-340 thousand / microliter;
- Second trimester - 160-330;
- 2nd trimester - 160-330; III trimester - 140-320.
After childbirth, a woman's body undergoes some changes, the main purpose of which is to reduce blood loss. This is due to increased blood clotting. After the end of the postpartum period, all indicators return to normal.
A complex test, including a group of laboratory tests to determine the general health, functioning of the main systems and organs of a pregnant woman in the third trimester of pregnancy.
Synonyms Russian
Pregnancy, III trimester.
English synonyms
Pregnancy third (III) trimester.
What biomaterial can be used for research?
Venous blood, an average portion of morning urine.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Eliminate fatty foods from your diet for 24 hours before the test.
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid (in consultation with your doctor) taking diuretics for 48 hours before collecting urine.
- Completely avoid (in consultation with your doctor) taking medications for 24 hours before the test.
- It is recommended to collect urine before menstruation or 2-3 days after it ends.
- Avoid physical and emotional stress for 30 minutes before the test.
- Testing for HIV infection can be carried out anonymously and confidentially. During a confidential examination, it is mandatory to present a passport.
- Do not smoke for 30 minutes before the test.
General information about the study
The third (III) trimester of pregnancy includes the period between 27 (28) and 38 (40) weeks of pregnancy. During this period, active growth of the fetus occurs, improvement of organ systems, in particular the respiratory system, development of sensory organs, and maturation of the nervous system. Clinical laboratory diagnostics are aimed at assessing the functioning of major organs and systems, in particular the kidneys, liver, blood coagulation system, endocrine system of a pregnant woman, as well as controlling infection during pregnancy.
A clinical blood test allows you to evaluate the qualitative and quantitative composition of blood according to the main indicators: red blood cells, leukocytes and their varieties in absolute and percentage terms, platelets. Detection of deviations in these indicators may indicate the presence of pathological processes and diseases in a pregnant woman. A reduced number of red blood cells and the hemoglobin content in red blood cells may indicate the presence of anemia in pregnant women. This condition can lead to placental insufficiency - the main cause of miscarriage, low birth weight babies and fetal death. Changes in the leukocyte formula may indicate a wide range of changes in the body of a pregnant woman. These may be laboratory signs of inflammatory and infectious diseases, pathologies that a woman has, but have not previously been diagnosed. The platelet count during pregnancy may be lower than normal, which must be taken into account. Significant changes in these indicators and developing thrombocytopenia require special monitoring, as they may be indirect signs of pathologies of the blood coagulation system, as well as such a severe complication of pregnancy as DIC syndrome (disseminated intravascular coagulation syndrome). Changes in ESR can be observed in the presence of acute and chronic inflammatory diseases and infectious processes. A slight increase in ESR can be observed during pregnancy. This test has high sensitivity but low specificity and is prescribed in combination with other indicators.
A general urinalysis with microscopy of urinary sediment is a set of diagnostic tests that allow one to assess the general properties of urine, its physicochemical properties, the content of metabolic products, and identify the qualitative and quantitative content of a number of organic compounds. These tests reflect the functional state of the kidneys and urinary tract, allow one to judge general metabolic processes, and suggest the presence of possible disorders, infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, and pregnancy diabetes. Detection of protein in the urine may be a sign of developing nephropathy in pregnancy; proteinuria more than 0.3 g in daily urine may indicate the development of a severe complication of pregnancy - preeclampsia. The severity of this condition varies greatly. Thus, with the development of mild preeclampsia after 36 weeks, the prognosis is usually favorable. On the contrary, the threat to the health of the mother or fetus increases significantly if preeclampsia develops early (before 33 weeks) and is aggravated by the presence of concomitant diseases.
In the third trimester of pregnancy, it is also necessary to monitor the functional state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic clotting pathway. The following indicators are obtained as results: Quick prothrombin time and international normalized ratio. Activated partial thromboplastin time (aPTT) characterizes the intrinsic pathway of blood coagulation. Fibrinogen is factor I (the first) factor of the blood plasma coagulation system. These indicators make it possible to assess the functional state of the liver, the main pathways of the blood coagulation system, and assess the functional state of its components. Their determination is important for predicting thrombosis during pregnancy, diagnosing a complication such as disseminated intravascular coagulation syndrome, and planning the necessary therapy during childbirth - a process accompanied by massive blood loss. It should be noted that there is a physiological increase in the levels of prothrombin and fibrinogen in the third trimester of pregnancy. But a sharp increase in these indicators requires special monitoring and prescription of the necessary therapy. The level of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, but a sharp increase in the concentration of D-dimer may indicate a large number of blood clots, which is most often caused by venous thromboembolism or disseminated intravascular coagulation syndrome.
Determination of such biochemical parameters as alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin and direct bilirubin fraction, total protein in serum allows us to assess the functional state of the liver. ALT levels may be slightly elevated, while AST levels are decreased. A significant increase in the concentration of transaminases may indicate the presence of liver damage, hepatitis, and the development of preeclampsia. A decrease in the level of total protein in the blood serum along with the loss of protein in the urine and with an increase in blood pressure more than 140/90 mm Hg. Art. is also a sign of developing preeclampsia.
To exclude the development of diabetes in pregnant women (gestational diabetes), the development of complications, in particular diabetic nephropathy, it is necessary to determine the level of glucose in the blood plasma.
To assess the functional state of the kidneys, in particular the integrity of glomerular filtration processes, several diagnostic parameters are used. The most important and characteristic is the determination of the levels of urea and creatinine in the blood serum, as well as the assessment of the glomerular filtration rate. It is important that creatinine levels are reduced by almost half in pregnant women due to increased blood volume, increased blood flow in the kidneys and, accordingly, an increased degree of filtration. Also, an increase in renal filtration causes a decrease in the amount of urea in pregnant women.
Typically, pregnancy occurs with normal levels of thyroid-stimulating hormone (TSH) in the blood. This euthyroid state is maintained by all components of the thyroid system and placental hormones, in particular human chorionic gonadotropin and human chorionic thyrotropin. The thyroid hormone systems of the mother and fetus are independent of each other and weakly penetrate the mature placenta. The TSH level in the blood of pregnant women may increase with the development of preeclampsia.
In the third trimester of pregnancy, it is also recommended to retest for hepatitis B - HBsAg, hepatitis C - anti-HCV, antibodies, HIV infection - HIV 1.2 Ag/AbCombo (determination of antibodies to HIV types 1 and 2 and p24 antigen), syphilis - antibodies to Treponema pallidum. The incubation period for some infections varies greatly and a negative result from tests taken early in pregnancy may change in the last weeks of pregnancy or remain negative. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or perform a planned cesarean section.
What is the research used for?
- For preventive examination of pregnant women in the third trimester of pregnancy.
- If there is a suspicion of deviations in the normal functioning of the systems and organs of pregnant women.
- To diagnose complications of the third trimester of pregnancy.
When is the study scheduled?
- Pregnant women in the third trimester at 27-38 (40) weeks of pregnancy.
What do the results mean?
Reference values
For each indicator included in the complex:
- [02-005] Clinical blood test (with leukocyte formula)
- [02-006] Urinalysis with microscopy
- [02-007] Erythrocyte sedimentation rate (ESR)
- [03-001] D-dimer
- [03-003] Activated partial thromboplastin time (APTT)
- [03-007] Coagulogram No. 1 (prothrombin (according to Quick), INR)
- [03-011] Fibrinogen
- [06-003] Alanine aminotransferase (ALT)
- [06-010] Aspartate aminotransferase (AST)
- [06-015] Plasma glucose
- [06-021] Serum creatinine (with GFR determination)
- [06-034] Serum urea
- [06-035] Total protein in serum
- [06-036] Total bilirubin
- [06-037] Direct bilirubin
- [07-009] anti-HCV, antibodies
- [07-025] HBsAg
- [07-032] HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- [07-049] Treponema pallidum, antibodies
- [08-118] Thyroid-stimulating hormone (TSH)
What can influence the result?
- The use of medications, in particular hormonal ones.
Reasons for increase or decrease
In some cases, the number of these blood cells decreases or increases. There could be many reasons for this. The main factors for low platelet levels are:
- the occurrence of an allergic reaction;
- intrauterine fetal death;
- viral diseases;
- Poor nutrition leading to insufficient intake of vitamin B12 and folic acid;
- drug poisoning;
- long-term use of antibiotics;
- obstetric hemorrhage, for example caused by placental abruption;
- autoimmune thrombocytopenia;
- neuropathic diseases;
- increased death of red blood cells due to hormonal imbalances.
In some cases, low levels of these cells can be observed under the influence of physiological factors. In this case, no special treatment is required. However, it is important to keep track of all times. For this purpose, blood tests are carried out regularly.
There is also a secondary form of the pathological condition, in which there is a decrease in the number of platelets. In this case, the cause may be radiation or toxic poisoning.
Factors that contribute to the appearance of an increased platelet count include:
- cardiovascular abnormalities;
- predisposition to thrombosis;
- phlebeurysm;
- allergic reactions;
- lack of iron in the body;
- formation of malignant neoplasms;
- taking certain medications;
- infectious diseases;
- pathologies of the autoimmune system;
- increased toxicity in early pregnancy.
Sometimes a high cell count occurs when there is no fluid in the body.
Tests in the third trimester
- General blood analysis;
- Blood chemistry;
- General urine test at each appearance;
- Repeated vaginal flora smear;
- Repeated tests for HIV infection, hepatitis B and C;
- Wasserman reaction;
- Last screening ultrasound;
- Additional tests as recommended by doctors.
In addition to these tests, a cardiotocogram is prescribed - an instrumental diagnostic method designed to determine the fetal heart rate and also record its movements.
Symptoms
Although the diagnosis is made solely on the basis of test results, in most cases an abnormality can be suspected by the appearance of certain symptoms.
If your platelets have dropped, you may experience symptoms such as:
- The formation of bruises on the body, which can be provoked even by a light blow to the skin;
- small rashes;
- Bleeding gums during oral hygiene procedures;
- Nose bleed;
- Poor blood clotting due to skin changes;
- Dark-colored stool;
- Bloody discharge from the genital tract.
The symptoms of an increase in the number of cells are in many ways similar to the symptoms of thrombocytopenia. This is due to the fact that, despite the various factors that provoke the development of these pathological conditions, the manifestation is common: blood cells in the vessels begin to be distributed unevenly.
To avoid negative consequences that can be dangerous for both the pregnant woman and the fetus, constant monitoring of platelet levels in the body is necessary.
What tests are needed?
To control the composition of the blood, certain laboratory tests are carried out. Only after a thorough examination of the biological material is a diagnosis made: low or high platelet count in pregnant women.
Diagnostics consists of performing tests such as:
- General examination of the patient by a gynecologist, therapist or hematologist;
- Blood test to determine platelet count, ferritin and serum iron levels;
- Ultrasound examination of internal organs.
If necessary, an additional bone marrow biopsy may be recommended.
Sometimes there are situations where, despite positive blood test results, you may find that you have a low blood clot level or a tendency to form one. In this case, the patient is referred for a coagulogram.
This testing method determines the level of cell aggregation, that is, their ability to bind to collagen. In the normal range, this ratio should be between 30 and 60 percent.
To obtain the most accurate results, you must be well prepared when submitting material for analysis. It is important that blood sampling is carried out on an empty stomach. For several days, it is recommended to avoid taking medications that can negatively affect the number of platelets in the blood.
In addition, it is better to refuse the analysis if three days before the study there was an injury accompanied by bleeding or a burn.
Tests in the second trimester
In addition to mandatory monthly visits to the gynecologist, the following tests are taken:
- Repeated ultrasound - screening + 3 triple test (determination of β - hCG, AFP and free estriol fraction);
- General blood analysis;
- General urine test at each appearance;
- Blood test for toxoplasmosis;
- Blood test for glucose;
In addition to the above tests, the doctor will prescribe a gynecological examination, which will give an idea of the size of the uterus and determine the presence of tumors. For chronic diseases, additional studies are prescribed. Also, starting from the second trimester, the doctor will be required to listen to the fetal heartbeat, using a special device - an obstetric stethoscope.
Treatment of thrombocytopenia and thrombocytosis
Treatment tactics will be chosen based on the diagnosis. In both cases, complex treatment will be required to correct the situation.
Drug therapy
The third trimester of pregnancy is considered the most dangerous period for low platelet levels. Treatment in this case should be aimed at eliminating the cause that caused the decrease in the number of cells.
The following drugs are used to increase the platelet count:
- Glucocorticosteroids, the course of which can be either systemic or short-term;
- intravenous immunoglobulins;
- lamellar mass, which is prescribed for complicated pathological conditions.
If conservative treatment methods do not bring positive results, a method is used in which the spleen is removed using laparoscopy.
If you have been diagnosed with elevated platelet levels, you should take medications such as:
- coagulants;
- antiplatelet drugs.
If thrombocytosis is incompatible with labor, your doctor will advise you to terminate the pregnancy.
If there is a slight deviation in height from the norm, no special treatment is required. In this way, the body can respond to uteroplacental blood flow.
Diet
No less important for the normalization of platelets is the nutrition of the expectant mother. To increase your platelet count, you should follow certain recommendations:
- Include plenty of beets and beet juice in your diet.
- Consume plenty of sesame oil. It can be added to vegetable salads. This drug regulates platelet levels and improves blood clotting.
- Monitor your iron levels. The daily norm should be about 30 milligrams. Experts recommend eating buckwheat, beef and liver.
- Eat foods high in vitamin B12 and folic acid every day. This may include meat, fish, dairy products, nuts and eggs.
- Take ascorbic acid.
In addition, to normalize the reduced number of cells, it is good to drink rosehip tea, as well as nettle decoction.
If this indicator increases, it is necessary to include in the diet such foods as:
- juice (can be made from cranberries, tomatoes, citrus fruits, apples or cranberries);
- olive oil or flaxseed oil;
- mackerel and other fatty fish;
- Garlic;
- legumes and grains;
- milk and dairy products;
- Herbs.
- bananas;
- pomegranate juice;
- rosehip;
- lentils;
- Italian nuts;
- mango.
Fluid intake also plays an important role. The daily minimum allowable intake for pregnant women is at least one and a half liters of clean water.
Possible complications
If you do not take quick action to normalize your platelet levels, this can lead to serious consequences.
Deviation from the norm in a large direction leads to:
- intrauterine growth retardation;
- inevitable miscarriage;
- severe toxemia;
- phlebeurysm;
- thrombosis of the upper and lower extremities;
- heart attack or embolism.
When platelet levels are low, complications arise such as:
- uncontrolled heavy bleeding;
- premature birth;
- Thrombocytopenia in a child.
With early diagnosis and proper treatment, such problems can be avoided.
Prevention
To prevent the development of thrombocytopenia in a pregnant woman, it is important to follow certain rules:
- Eliminate all factors that can negatively affect the state of the immune system;
- Before planning a pregnancy, get all the necessary vaccinations against ARVI, rubella, chickenpox and other viral infections;
- Stop taking certain medications in early pregnancy;
- Change your diet.
To prevent thrombocytosis, the following preventive measures are taken:
- maintaining an active lifestyle;
- Excluding foods that increase blood viscosity from the menu;
- Drink more fluids and food to thin your blood.
Be sure to monitor your platelet count throughout your pregnancy. This is why it is so important not to neglect regular examinations by specialists and examinations.
Interpretation of basic blood and urine tests during pregnancy.
During pregnancy, changes occur in a woman's body that allow her to adapt to new conditions. For this reason, many test results differ from those before pregnancy. But in no case are deviations from accepted norms any kind of diagnosis, but serve only as a method for diagnosing various diseases. Only a doctor monitoring the course of pregnancy should interpret the tests, and even more so prescribe treatment.
General and biochemical blood tests
Hemoglobin is the source of oxygen in the body. It is with a lack of this blood indicator that the so-called iron deficiency anemia develops. Norms during pregnancy: 110 – 150 g/l.
White blood cells recognize foreign cells in the body. Their increase indicates the presence of an infectious inflammatory process in the body of a pregnant woman, which requires immediate medical intervention. Norm: 4.0-11×109 / l, in some cases it is allowed to exceed the indicator up to 15x109 / l.
Red blood cells deliver oxygen throughout the body. Normally, this figure ranges from 4.0 to 11×109 /l.
Platelets are responsible for blood clotting. Norm: 180-320x109/l. A low platelet count indicates poor blood clotting, which can cause bleeding during pregnancy.
The ESR (erythrocyte sedimentation rate) level increases during pregnancy. In the first trimester, this figure can be 15 mm/h, in the second – 25 mm/h, in the third – 40 mm/h.
A biochemical blood test allows you to assess the functioning of internal organs and timely detect pathological changes in the functioning of the kidneys, liver, heart, lungs, etc. Most often, the following indicators are considered in pregnant women: ALT (normal: up to 32 U/l), AST (normal: up to 30 U/l), total protein (norm: 63/68 g/l), glucose level (norm: up to 3.5-4.0 mmol/l), alkaline phosphatase (norm: up to 240 U/l), bilirubin ( norm: 3.4 – 17.2 µmol/l), urea (normal: 2.5-6.3 mmol/l), etc. At the discretion of the doctor, the list of indicators can be shortened, or vice versa – expanded.
Analysis of urine
Urine examination is a very important and indicative method for detecting all kinds of abnormalities throughout pregnancy. In addition, urine analysis allows you to monitor kidney function, especially in late pregnancy, when the load on this important organ increases.
When taking the test, you need to make sure that the urine collection container is clean and sterile. It is best to buy a special disposable jar at the pharmacy for collecting tests: firstly, it is not so expensive, and secondly, it will provide the most accurate analysis.
When examining urine, the following indicators are considered:
- Protein. According to the norm, it should not be there, but for pregnant women there is a small amount of protein in the urine up to 0.033 g/l. acceptable.
- The level of salts in the urine may be slightly reduced.
- There should be no leukocytes in the urine, but it is considered acceptable if their value does not exceed 5 units.
- Red blood cells should also be absent, but their content is acceptable up to 3 units in the field of view.
- Bacteria in the urine may indicate acute or chronic diseases of the kidneys and the urinary system as a whole, because Normally they shouldn't be there.
- Bilirubin, ketone bodies, casts and glucose should be absent in a normal urine test.
- Urine acidity (pH) in pregnant women is 4.5 – 8. A low value indicates early toxicosis, potassium deficiency or dehydration.
In case of any deviations from the established standards, the doctor will require you to retake the test, and will also prescribe more detailed studies, for example, a urine test using the Nechiporenko method, which is designed to identify hidden inflammatory processes in the urinary system.