Back forward
Dear patient!
We hope that this brochure will help you understand more about your vascular system and your disease.
Arterial disease affects hundreds of thousands of men and women of all ages and lifestyles, just like you. While we are unable to defeat the disease, we must learn to live a full and productive life with it.
The brochure is intended as additional information for the patient and does not replace actual consultation with doctors. If you have any additional questions, please consult your physician or surgeon.
What is the vascular system?
First, let's take a look at the vascular system and how it works.
All parts of the human body require blood to be delivered to them. Blood carries oxygen and nutrients and performs many other important functions that allow your body to function properly. Blood is distributed throughout the body through the vascular system, which consists of the heart, arteries and veins. The heart is a highly efficient pump consisting of a special muscle that pumps blood into the arteries. Arteries are like tubes that distribute blood to all parts of the body.
The arteries divide into branches, which become smaller and smaller until they become microscopic capillaries. In capillaries, oxygen and nutrients can easily leave the blood and enter tissues and organs. After the blood passes through the capillaries, it enters the veins, which become larger and larger along the way to carry the blood back to the heart. The heart then pumps the blood to the lungs so that it can be oxygenated before being pumped back into the arteries. Thus the whole process begins again. The blood that leaves the heart is rich in oxygen, which then remains in the organs. The blood that returns back to the heart through the veins is depleted of oxygen and needs to be replenished in the lungs.
Normally, your heart contracts (beats) more than 100,000 times a day (an average of 70 beats per minute), pumping about 7,000 liters, on a total path of 19,000 kilometers through the entire vascular system, arteries and veins. This incredible system produces an average of 2.6 billion cycles over your lifetime.
Our vascular system contains about 4.5 liters of blood, which is regularly replenished with new cells.
Our services in cardiology
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Echocardiography (EchoCG) with Dopplerography and color mapping | 4 000 |
| Electrocardiogram monitoring (Holter, daily) | 5 400 |
| Treadmill test (stress test) | 4 900 |
All services
How do vascular diseases manifest themselves?
An elegant man is walking down the street and suddenly stops. There is a mask of suffering on the face. And after a few minutes, as if nothing had happened, he smiles and continues on his way. What's the matter? In extreme pain. The pain is especially noticeable when going up, for example up stairs. It forces you to stop or slow down. After 2-4 minutes the pain disappears. But as soon as you hit the road again, she returns. And so it repeats again and again: walking - pain - rest, walking - pain - rest. This is intermittent claudication - a symptom, alas, familiar to many firsthand. Its cause is insufficient blood supply to the muscles of the lower extremities, which occurs during exercise. At this time, the muscles require much more oxygen, but the arteries in the legs cannot cope with their work. Oxygen is not supplied in the required volume, and the muscles signal this with pain. Intermittent claudication is a symptom of “related” diseases: obliterating endarteritis and obliterating atherosclerosis of the lower extremities.
Using the compression technique
In many types of martial arts, fighters know how to put a person to sleep by pressing on the carotid artery. This technique allows them to render the enemy unconscious for a quarter of a minute. It only takes 15 seconds for a person to fall asleep. But this technique remains prohibited, because it cannot always be performed correctly.
Many people do not understand what happens if you press on the carotid artery. Especially teenagers. Therefore, you should not joke with squeezing the neck and its arteries in order to protect yourself and the other person from fatal complications.
It is useful to know what happens if the carotid artery is compressed. But it's not that useful to practice it. Just a few extra seconds without oxygen for the human brain can turn into a terrible tragedy.
What is atherosclerosis and endarteritis?
With obliterating endarteritis, vasospasm occurs. Prolonged spasm leads to changes in the inner wall of the artery, its coarsening and thickening. As a result, the tissues of the limbs suffer. Endarteritis is typical for men aged 20-30 years.
The cause of obliterating atherosclerosis is the well-known atherosclerotic plaque: a place where cholesterol and other fats accumulate. Atherosclerosis is a systemic process that affects arteries in many organs. In addition to the lower extremities, its “prey” includes the brain, heart, and kidneys.
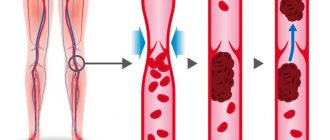
An atherosclerotic plaque grows into the lumen of the artery, blood clots form, and the blood supply to the lower extremities sharply deteriorates. Atherosclerosis usually affects large vessels: the aorta, iliac arteries, and the arteries of the thigh and leg extending from it. The higher the pain is felt, the closer to the heart the affected artery is, the more severe the disease. Atherosclerosis has its own “contingent” - men over 40. The vast majority of them are smokers. As the blood supply to tissues decreases, the cells left without oxygen die and die - gangrene develops. And then amputation is inevitable - a finger, a foot, part of a leg, a knee, a thigh... It's scary. Especially when you consider that young, able-bodied men become disabled. Necrosis may develop gradually or may occur suddenly. A sharp pain in the leg indicates that a disaster has occurred. What other manifestations of arterial disease occur? Chilliness, tingling, and burning sensations occur in the fingertips. The leg turns pale and becomes cold to the touch. The skin of the feet and legs dries and peels. Nail growth slows down, hair falls out on the leg.
In most cases, a specialist can establish a presumptive diagnosis based on examination. To clarify the diagnosis, the doctor may prescribe an examination, including rheovasography, thermography, and ultrasound. One of the most informative methods for diagnosing arterial diseases is angiography - x-rays of blood vessels after filling them with a special contrast agent. The information obtained will give the doctor the opportunity to determine treatment tactics, and most importantly, to decide whether surgery, bypassing the affected arteries and creating a bypass for blood flow is necessary.
The insidiousness of atherosclerosis lies in the fact that not only the arteries of the legs are affected, but also the vessels of other organs. If the arteries of the heart are damaged, coronary heart disease occurs (angina pectoris, arrhythmia, myocardial infarction), if the renal arteries are damaged, hypertension occurs, and if the arteries of the brain are involved in the process, chronic cerebrovascular insufficiency and stroke occur. Therefore, doctors of related specialties - therapists, cardiologists, neurologists - are involved in the examination.
Place of artery pulsation
Many people know that if a person loses consciousness, they need to check the pulse in their neck. This is where the external carotid artery can be felt.
It is worth placing two fingers just below (2-3 cm) the edge of the jaw, next to the large cervical muscle. The fingertips will feel the pulsation of the vessel wall. This skill is necessary for measuring heart rate, since it is not always possible to feel the pulse on the wrists.
What if you press too hard on the carotid artery? This will only worsen the person's condition. The pressure should be gentle so as not to block blood access to the brain even for a short period.
What is the reason?
When talking about the occurrence of atherosclerosis and other cardiovascular diseases, experts usually do not use the word “cause”. Instead, they use the concept of “risk factor,” that is, a factor that significantly increases the likelihood of developing a disease. The concept of “risk factor” includes habits, living conditions, age and gender. Taking into account all risk factors allows us to develop optimal recommendations for the prevention and treatment of cardiovascular diseases. Risk factors for the development of atherosclerosis include:
- age (over 40-50 years)
- male
- genetic predisposition
These risk factors, as you understand, are irreversible. That is why, if you are a man older than middle age, you should pay special attention to eliminating other risk factors that are fully or partially reversible:
- smoking
- high blood pressure (above 140/90 mm Hg)
- obesity
- high blood cholesterol
- diabetes
- low physical activity
- mental and emotional stress
Eliminating risk factors significantly reduces the likelihood of developing atherosclerosis and even delays the progression of an existing disease. Therefore, we can say with confidence that the prevention of atherosclerosis largely depends on ourselves. A healthy lifestyle, quitting smoking, reasonable physical activity, proper nutrition are the simplest and most effective ways to combat the disease. Assess your risk factors and draw a conclusion. If you smoke and are overweight, or your blood pressure is high, pay more attention to your diet. It is also useful to know the level of cholesterol in the blood. Normal cholesterol content is no more than 5.2 mmol/l. Cholesterol levels greater than 6.5 mmol/l require a combination of diet and drug therapy.
What should I change in my diet?
The basic principles of diet therapy for atherosclerosis can be formulated as follows:
DECREASE:
- total fat intake
- consumption of saturated fatty acids (butter, animal fats)
- eating foods rich in cholesterol
- salt consumption (up to 3-5 g per day)
INCREASE:
- consumption of fiber and complex carbohydrates (vegetables and fruits).
- consumption of foods containing polyunsaturated fatty acids (fish, seafood, liquid vegetable oil)
6. HYPOCHOLESTEROL (HYPOLIPIDEMICA) DIET
The principle of the diet is to significantly reduce the consumption of cholesterol and easily digestible carbohydrates, and for overweight patients, a significant reduction in calorie intake
This diet is general in nature; if there are various variants of lipid metabolism disorders, the attending physician makes appropriate adjustments. It is very important to avoid eating after 19:00, and dinner should consist entirely of foods containing a large amount of fiber and absolutely no cholesterol (vegetables, fruits).
I.N E L Z
Consume foods containing large amounts of saturated fat. These include the following:
- Milk and dairy products (condensed milk, cream, sour cream, butter, cheese, cottage cheese, kefir, curdled milk, yogurt, ice cream, milkshake), as well as milk porridge.
- Pork and cooking fat, margarines, coconut and palm oil.
- Pork, lamb (respectively ham, bacon, brisket, ham, carb, neck), lard and, accordingly, those products in which they can be included (smoked and boiled sausages, frankfurters, sausages, cutlets, steaks, meatballs, canned meat, meat in jelly), fatty meat broths.
- Liver (respectively pate) and other offal (kidneys, lungs, brains).
- Red poultry meat, leather.
- Sturgeon, fish spark, fish liver, crayfish, crabs, shrimp, shellfish.
- Eggs (respectively mayonnaise).
- High quality bread and crackers made from it, confectionery products (cakes, cookies, pastries, biscuits), because they contain milk, eggs, sugar.
- Pasta.
- Cocoa, chocolate, coffee beans.
- Sugar, honey
- Cold drinks: sweet carbonated drinks (Fanta, Pepsi, etc.)
- Alcoholic drinks: beer, sweet fortified wines, liqueurs.
II . CAN
Consume the following products in moderation (no more than 2 times a week, or more often, but in limited quantities as prescribed by your doctor):
- White poultry meat without skin, lean beef. The preferred cooking method is boiling, grilling, microwave processing; undesirable cooking method - stewing, frying.
- Secondary broth from lean beef and lean chicken (a portion of meat is boiled in water a second time, the first broth is drained).
- River fish, incl. red.
- Bread made from bran and rye flour, crackers made from it.
- Buckwheat (cook in water without adding oil).
- Potatoes soaked in water, peeled, for an hour. The preferred method of preparation is boiling. Light frying in vegetable oil is allowed.
- Mushrooms.
- Ketchup (not sweet), mustard, soy sauce, tkemali sauce, adjika, vinegar, spices, herbs.
- Tea, instant coffee without sugar.
- Chewing gum without sugar.
- Walnuts, almonds, hazelnuts.
- Alcoholic drinks: vodka, cognac, whiskey, tequila, dry wine.
III . NEED TO
Eat the following foods daily in large quantities:
- Vegetable oil (sunflower, corn, salad, olive, soybean, rapeseed, cottonseed).
- All vegetables (fresh, frozen, canned without sugar, dried fruits) with peel: carrots, beets, cabbage, turnips, radishes, radishes, zucchini, squash, eggplant, tomatoes, cucumbers, cauliflower, peas, beans, soybeans, corn. When preparing a vinaigrette, the vegetable oil should not be excessive (i.e., remain at the bottom of the dish). Cold vegetarian borscht is healthy.
- All fruits and berries with peel.
- Onions, garlic, herbs (parsley, celery, cilantro, basil, lettuce, spinach, wild garlic, sorrel, etc.).
- Sea fish (cod, hake, navaga, ice fish, haddock, sprat), incl. fatty (halibut, herring, tuna, sardine). Method of preparation: boiling, baking, frying in vegetable oil, under marinade.
- Sea kale.
- Oatmeal (from unrefined oatmeal or “Hercules”), boiled in water.
- Cold drinks: mineral water, fruit water, fruit juice and fruit drink without sugar.
When is surgery needed?
The above measures are practically all that a patient may need to treat atherosclerosis. Unfortunately, when the disease progresses far, the changes in the blood vessels are significant, and these measures become insufficient. Then surgical treatment is required. Only your attending physician or surgeon can decide whether you need this treatment.
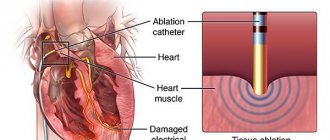
Usually, when the question of surgical intervention is raised, angiography is a very important step. This is an X-ray examination, which is accompanied by the introduction of a contrast solution (dye) into the vascular system through a syringe in the groin or arm area. An angiogram shows a “map” of your arteries and gives the exact location of narrowings and blockages that are causing the above symptoms. Some of the narrowings and blocks can be eliminated using a balloon catheter inserted into the vessel through a special needle. The balloon is positioned against the narrowing and then inflates, expanding the vessel. This is the so-called angioplasty. Other narrowings and blockages that cannot be treated with angioplasty are treated with surgery - bypass surgery, i.e. forming a bypass of the blockage site.
A vascular bypass can be described as a bypass built around a crowded city. An overpopulated city is a narrowing in the vessel, and a double road is actually a “shunt”. With this technique, the narrowed or blocked area is not removed, but a shunt is attached in the area of a healthy vessel above and below the narrowed area. The picture shows a diagram of this technique.
The choice of bypass material depends on the location of the affected part of the artery. Most often, a vessel prosthesis is installed instead of the abdominal aorta and arteries of the extremities. With this localization, the prosthesis can function flawlessly for many years. A shunt in the thigh and leg area is often made from your own vein, which can be used as a “spare part”.
With some bypass operations, a good result can only be achieved using an artificial prosthesis. In this case, the surgeon must decide which of them is most suitable in this case.
Branches of the external carotid artery
Where the external carotid artery is located was described above; now its slightly more detailed structure and classification of parts will be considered.
According to the topographic characteristics, four branched groups are part of the external carotid artery, namely:
- The branches of the anterior group are divided into the superior thyroid atrery, which supplies blood to the pole of the thyroid gland, namely its overlying part, the lingual artery, the trunk of which lies deep in the region of the submandibular triangle, and the facial artery, located slightly above the lingual.
- The branches of the posterior group are divided into the sternocleidomastoid artery, which, departing almost at the level of the facial artery, falls back and down, entering the sternocleidomastoid muscles, the occipital artery, passing under the belly of the digastric muscles and moving towards the back of the head, and the posterior auricular artery, which supplies blood to the human scalp and concha.
- Branches of the medial group. They include only the ascending pharyngeal artery, which originates from the surface of the inner wall of the external carotid artery and stretches to the lateral walls of the pharynx.
- The branches of the terminal group are represented by the artery of the maxilla, which, departing from the mandibular neck, goes forward and passes between the branch of the mandible and the sphenomandibular ligament and the superficial artery of the temple, which is the final part of the external carotid artery.
What is a vascular graft?
A vascular graft is a human-made tube that replaces or creates a bypass for a real blood vessel, most often an artery. This brochure has been specially prepared to help you understand how your vascular graft works and what it will do for you.
The successful development of vascular prostheses is an outstanding event of our time. Recently, there has been an extremely high interest in the problem of implantation of artificial vessels and other aspects of vascular surgery. The first vascular graft was developed in 1960. Since that time, dramatic changes have occurred to improve the quality of the material used, and modern prostheses are significantly superior to their ancestors.
Initially, replacing the vessel with an artificial one was just an experiment, but over time this operation became traditional and hundreds of thousands of people were successfully cured. Modern dentures are widely recognized as reliable and trustworthy.
How does an artificial vascular graft work?
Artificial vascular prostheses are a substitute for the blood vessels of the human body developed by scientists.
A vascular prosthesis consists of a tube of various lengths, shapes and diameters made of complex material. Each individual component is made from the highest quality material and is carefully monitored at every stage of production using the latest technology. The production technology guarantees complete sterility and no risk of transmission of infection when using the prosthesis.
The vascular prosthesis has a large margin of strength and stability, significantly exceeding the strength and stability of natural arteries. The prosthesis is designed to be a permanent part of your vascular system. While the functioning of natural vessels is constantly affected by many factors (such as age and disease), these factors do not affect the material of artificial prostheses.
How is the operation performed?
The carotid artery stenting procedure is performed from the femoral approach. The principle of the intervention is similar to stenting other arteries, but there is one caveat. When working with the carotid artery, special protection is used - a filter trap, which prevents destroyed fragments of atherosclerotic plaque from entering small arteries.
Stenting consists of the following steps:
- Installation of a sluice in the femoral artery under local anesthesia;
- The carotid arteries are contrasted using a special substance;
- The issue regarding stenting of one or more affected areas is being resolved;
- A conductor is inserted into the place of narrowing of the artery along the vascular bed, through which a filter-trap is passed;
- Then a stent is inserted into the problem area, which is carefully positioned and secured.
As a result, blood flow in the affected artery is completely restored.
How long can a vascular graft work?
The functioning of shunts (prostheses) can be influenced by many factors. For example, how much atherosclerosis was developed before surgery, how quickly it progressed after surgery, whether you continued smoking, and how things stand with other factors that influence the development of atherosclerosis. Taking certain medications may help make the shunt work longer. When a prosthesis malfunctions, the cause is hidden not in the prosthesis, but in the changes that occur in the body with age and illness.
Answers to your questions
- Question: How can I check that my prosthesis is working correctly?
Answer: After implantation of the prosthesis, the symptoms and signs that preceded surgical treatment will become significantly less and, in many cases, completely disappear. If symptoms and signs do not return or worsen, it is safe to say that the prosthesis is working normally.
- Question: What will happen to my vascular system if the prosthesis stops working properly?
Answer: The organ or tissue supplied by this prosthesis will gradually or suddenly receive less blood. In this case, typical symptoms and signs (depending on the area where the prosthesis is located) will develop. For example, increased pain when walking or decreased walking distance without pain, or cold feet.
- Question: How often does my vascular graft need to be replaced?
Answer: Your prosthesis was designed to last indefinitely. But as mentioned above, in some cases the operation of the prosthesis may be disrupted. If this happens, you will need to replace the prosthesis, but the decision is made individually in each specific case. There is a small risk that the prosthesis may become infected. We guarantee that when the prosthesis is implanted, it is absolutely sterile. The operation is also carried out under conditions of the greatest possible and strictest sterility. In very rare cases, infection can still spread to the prosthesis from your skin or from the air in the operating room. This may have no effect, but if the prosthesis becomes infected, it should be removed.
- Question: Can the prosthesis be affected by external energy influences, such as running engines, microwave ovens, airport security checks, sunbathing, etc.?
Answer: No
- Question: Should I reduce my activity level?
Answer: Only your attending physician can decide the level of individual restrictions. He knows your health condition and the location of the prosthesis. After implantation of a vascular prosthesis, as a rule, the patient can return to a completely normal and active life. However, when implanting a prosthesis, your doctor may restrict you from certain activities, such as sports, lifting weights, or gardening, until the prosthesis is fully integrated into the vascular system.
- Question: Should I limit my walking?
Answer: Dosed walking is not harmful, but even beneficial. Physical activity on the legs will prevent atrophy (reduction in volume) of the muscles through which small arteries pass. The greater the muscle mass, the more blood vessels will form. Set a walking rhythm for yourself (for example, 60 steps per minute) and try to walk a certain distance every day. Walk until pain appears in your leg muscles. There is no need to walk while overcoming the pain - the pain causes a spasm of the arteries. Record in the table the number of steps that you managed to walk without pain, and you will see that it gradually increases.
- Question: Can I smoke?
Answer: You should not smoke. It has been irrefutably proven that smoking has a negative impact on the long-term results of the vascular prosthesis, as well as on the condition of your own arteries in general.
- Question: Can I stop taking my medications for a while?
Answer: Some drugs used in the treatment of atherosclerosis are taken in courses of 2-3 months, others - continuously. Only your attending physician can decide in what dosage and according to what scheme they should be used. In some cases (for example, during an upcoming surgery), it is advisable to stop taking certain medications for a while or replace them with others. In any case, inform your attending physician about your illness and the medications you are taking.
- Question: How about reducing my sexual activity?
Answer: Only if the doctor recommends that you reduce sexual activity. In all other cases there is no need for any restrictions.
- Question: Can I continue to drive my car?
Answer: In most cases, yes. But you should always consult your doctor.
- Question: If I develop an infection or have surgery, do I need to take special precautions?
Answer: It has been proven that even with such ordinary manipulations as dental treatment, a temporary release of microbes into the blood can occur. If these agents come into contact with the prosthesis, it may become infected. Therefore, if you have an infectious disease, if you are undergoing a minor operation, for example, treatment or tooth extraction, cystoscopy, fibrogastroscopy or intestinal examination, you should definitely consult your doctor about taking antibiotics.
Stop bleeding
If the carotid artery is damaged, bleeding begins so severely that death can occur within 2-3 minutes. If at this moment you correctly apply pressure to the vessel and stop or at least slow down the blood loss, this can save a person’s life. However, the technique that allows you to clamp the SA without causing harm is quite complex, and its application requires clear practical skills.
You can make a tampon from gauze or fabric and try to clamp the artery in the place where the pulsation is detected. However, this method is unreliable and dangerous. Weak pressure will not give the desired effect, and if you put too much pressure on the vessel, it can kill a person.
Applying a tourniquet will be much more effective and safer. To do this, the arm opposite to the site of injury is raised up and positioned so that the forearm lies on the vault of the skull and the shoulder is pressed to the ear. A tourniquet is placed around the neck and this arm, which will prevent compression of the undamaged branch of the artery. However, as a rule, it is not possible to completely stop bleeding in this way - applying a tourniquet only slows down blood loss, allowing the victim to wait for qualified medical care, which should follow as quickly as possible. Otherwise, death becomes inevitable.