A heart murmur is a pathological sound that occurs when blood passes from the atrium to the ventricle and vessels of the heart, and vice versa. This symptom should not be ignored, since in most cases it is associated with disease of the heart or other organs.
Only a doctor can detect the noise by listening to the chest. The patient himself hears noise only in cases where pathological changes are extremely pronounced. Therefore, it is important to regularly see a cardiologist to identify initial deviations in health, in which the success of therapy is high.
Causes of heart murmur
The appearance of a heart murmur is associated with a disruption in the movement of blood through the vessels. This occurs in various diseases. The main mechanisms causing noise are:
- accelerating the speed of blood flow while reducing the number of red blood cells and other cells in it;
- reverse movement of blood through a valve that should normally be closed (valvular insufficiency);
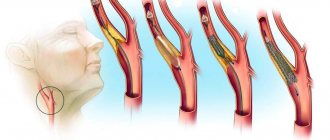
- the appearance of obstacles to the blood flow (narrowing of the valve, the presence of atherosclerotic plaques in large vessels).
The main and most common causes of noise:
- aortic valve insufficiency or narrowing;
- mitral valve insufficiency or narrowing;
- pulmonary valve insufficiency or narrowing;
- tricuspid insufficiency or narrowing of the tricuspid valve;
- hypertrophy (enlargement) of the left ventricle;
- arterial hypertension;
- infective endocarditis;
- anemia;
- atherosclerosis;
- thyrotoxicosis;
- fever.
Thus, all the causes of heart murmurs are divided into 2 groups:
- cardiac, associated with heart disease;
- non-cardiac, associated with general (non-cardiac) disorders.
Heart murmurs in children: causes, diagnosis and treatment
Boo-tup, bu-tup... Having applied a phonendoscope to the child’s chest, the doctor hears two heart sounds. However, sometimes, in addition to these tones, noise can be heard.
What are the types of heart murmurs? Where do they come from? And what to do if such noise is detected?
With these and other questions, we turned to Tatyana Mikhailovna Frolova, a pediatric cardiologist and functional diagnostics doctor at the Expert Clinic Smolensk.
— Tatyana Mikhailovna, what is a heart murmur and where does it come from?
A heart murmur occurs when there are any obstacles to the flow of blood in the heart itself or in large vessels. Normal blood flow can be figuratively compared to a wide, full-flowing river that flows and murmurs regularly, and the movement of blood in the presence of obstacles can be compared to a mountain river flowing along an uneven path and therefore heard from afar.
Turbulence of blood movement is the main mechanism for the appearance of heart murmurs in both adults and children.
— Is a heart murmur a diagnosis or a syndrome?
Neither one nor the other. This symptom is one of many that occur in various pathologies.
— Many mothers associate heart murmurs in a child with defects. When is a heart murmur a temporary situation, and when should you worry?
It is difficult to conclude from noise alone and its characteristics whether this situation will be temporary or not. Therefore, the child’s condition, all sound characteristics of the noise, data from additional research methods are taken into account, and always in dynamics. For example, in some cases, even in the presence of a defect, the situation may resolve favorably after some time: the heart defect may self-destruct during the child’s growth, or the need for surgical correction of the heart defect will disappear.
— Are there physiological murmurs in the child’s heart?
Yes. Heart murmurs occur in newborns and are also observed in the first year of life. They are associated with intensive growth of the body, when the heart does not have time to grow as quickly. Heart murmurs can also occur between the ages of 4 and 7 years, during adolescence.
— Why do pathological heart murmurs occur in a child?
In most cases, the cause of pathological heart murmur in children is a heart defect (congenital or acquired).
The division of murmurs into pathological and functional, previously used (before the era of echocardiography/ultrasound of the heart), has lost its relevance today. Therefore, in order not to “miss” a defect, any noise - even one that meets the functional criteria - should be a mandatory reason for an in-depth study using echocardiography.
Heart ultrasound for adults and children: when is it prescribed and what will it show? Read more
— What age is critical for the occurrence of heart murmurs in children?
It is more correct to talk about the critical period for the occurrence of not the noise itself, but the reasons for its occurrence.
The first period is from the 3rd to the 8th week of pregnancy, when the heart is formed. At this stage, defects can form that lead to noise.
What can a fetal MRI reveal? Find out here
The second period is until the child is one year old. At this time, both physiological and functional and pathological (depending on the cause) noises can be heard.
All periods of intense growth of a child’s heart are also critical for the appearance of murmurs. Murmurs at this time can be observed even in the absence of heart pathology (physiological murmurs).
Infectious and colds in preschool age make an independent contribution, one way or another capable of causing changes in the heart, accompanied by murmurs.
How does ARVI manifest in children? Ulyana Vladimirovna Chemova, a pediatrician at the Expert Clinic Smolensk, tells the story.
— Is there a relationship between increased blood pressure and heart murmurs?
Rarely. A heart murmur is not the main manifestation of high blood pressure in a child, i.e. he may or may not be. And if it is present with high blood pressure, then it is mostly functional.
What should a child’s blood pressure be and how to measure it correctly? Neurologist at the Expert Tula Clinic, Anna Georgievna Sycheva, tells the story.
Perhaps the only serious reasons leading to murmur with high blood pressure are stenosis and coarctation of the aorta.
— Can a cold or infectious disease suffered by a baby cause a heart murmur?
Yes. In this case, different scenarios are possible. The infectious agent can affect the heart itself. In this case, the development of pericarditis, myocarditis, and endocarditis is possible. Against the background of illness, the child develops a heart murmur, which is considered a complication of infection.
In the presence of infection, a congenital pathology that had not previously manifested itself may appear. For example, a child has a slight narrowing of a large vessel leaving the heart. Infection, tachycardia, fever, intoxication lead to an acceleration of blood flow, and murmurs become obvious.
In addition, the acceleration of blood flow in itself can cause murmurs, even in the absence of any pathology in the heart.
— Can a baby’s heart murmur occur due to low hemoglobin?
A low hemoglobin level (anemia) by itself cannot cause murmur. However, with a lack of hemoglobin, one or another degree of oxygen starvation naturally develops. As a result, in order to deliver the required amount of oxygen to organs and tissues, the heart has to contract more often. Acceleration of blood flow, tachycardia, leads to noise.
— Can anemia be suspected by some external symptoms? What signs should alert a mother?
Symptoms of anemia are nonspecific and can occur with many other diseases. Their occurrence is caused by a lack of oxygen.
Signs of anemia include: fatigue, poor exercise tolerance, pale skin and mucous membranes, heart murmur, and frequent colds.
How many times a year should a child get colds? Ulyana Vladimirovna Chemova, a pediatrician at the Expert Clinic Smolensk, tells the story.
— Tatyana Mikhailovna, if a pediatrician listens to a child’s heart murmur at an appointment, is this always a reason for further examination by a cardiologist?
Absolutely yes, regardless of the noise characteristics. The assessment of noise by ear is quite subjective, therefore, in order not to “miss” the pathology, the pediatrician must refer such children to a cardiologist for further examination.
— If there is a heart murmur, what kind of diagnostics does the baby need to undergo so that the doctor can determine whether it is a functional murmur or a pathological one?
First of all, this is echocardiography, which allows one to evaluate the anatomical features of the heart, its layers, valve apparatus, and some functional features.
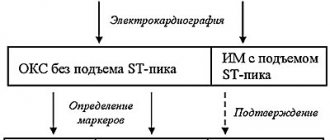
The second mandatory research method is electrocardiography. It makes it possible to find out the state of the myocardium, whether there are any rhythm disturbances, signs of overload of the heart, etc.
— Do any heart murmurs require treatment?
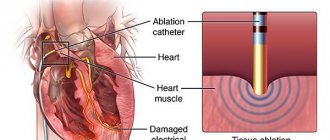
More precisely, talk about the reasons that cause them. Of course no. If these noises are physiological, they do not need treatment. If they are associated with another cause (anemia, viral infection, etc.), treatment of the underlying disease is necessary. In the case of significant heart defects, this is only surgical correction.
— Is a heart murmur a contraindication for playing sports?
In most cases, no. Physical activity commensurate with the state of health is allowed even with defects - of course, under certain conditions (for example, if it is compensated, there are no complaints or circulatory disorders). Observing such a patient over time (over time) is of great importance in order to determine the effect of sports on the child’s condition. All nuances must be discussed with the doctor in advance.
— How to protect a child’s heart from pathological murmurs? Tell us about prevention
If we equate pathological murmurs with congenital heart defects, then we need to talk, accordingly, about the prevention of defects.
Activities include proper pregnancy planning, correct behavior of a woman during pregnancy (optimal nutrition, infection prevention, taking vitamins).
How to properly prepare for pregnancy? The chief doctor of the Expert Tula Clinic, obstetrician-gynecologist Olga Evgenevna Malafeeva tells
If a woman takes any medications before a planned pregnancy, she should definitely consult with a doctor regarding their use and the possible effect on a future pregnancy and fetus.
After birth, it is necessary to perform an ECG and ultrasound of the heart for up to a year, especially in the presence of murmurs. This will make it possible to identify the defect at an early stage and make the right decision in each specific case.
If all these stages have passed without problems, then the prevention of acquired heart defects is carried out. It is carried out throughout a person’s life and includes the prevention of infections, primarily those directly affecting the heart. This also includes timely, competent treatment of acute and chronic foci of infection as prescribed and under the supervision of a physician.
Sports activities are important.
If any heart murmur occurs, consult a doctor promptly.
You can make an appointment with a pediatric cardiologist here
Please note: consultations are not available in all cities
For reference:
Frolova Tatyana Mikhailovna
Graduate of the pediatric faculty of the Orenburg State Medical Academy in 1997.
In 1998, she completed her internship in the specialty “Pediatrics”.
In 1999-2001 she completed postgraduate studies by correspondence and has an academic degree of Candidate of Medical Sciences.
In 2014 - professional retraining in the specialty "Pediatric Cardiology", in 2017 - in the specialty "Functional Diagnostics".
Currently he holds the position of pediatric cardiologist and functional diagnostics doctor at Clinic Expert Smolensk LLC. Receives at the address: st. 8 March, no. 20
Types of heart murmurs
Depending on what phase of blood circulation a heart murmur is observed, it is customary to distinguish:
- systolic murmurs, which are heard at the moment of ventricular contraction;
- diastolic murmurs heard when the heart muscle relaxes.
From the point of view of the nature of the appearance of noise, the following are distinguished:
- organic noise caused by a violation of the structure of the heart and its valves;
- functional noise associated with accelerated blood flow.
Based on localization, noises are divided into 2 classes:
- cardiac, or true, which are caused by circulatory disorders;
- extracardiac, appearing at the moment of heart contraction, but associated with pathological processes in nearby organs, including the aorta. Examples of such murmurs are those observed with pleurisy or atherosclerotic changes in the aortic wall.
Heart murmur in children
A heart murmur in children is not necessarily caused by heart or vascular disease. Most often, the reason is the rapid growth of the body or the presence of “extra” chords in the ventricles of the heart. With age, these features normalize and the noise disappears. However, doctors advise in any case to bring the child for diagnostics in order to rule out serious health problems. One of the diagnostic methods is Doppler ultrasound or echocardiography of the heart.
answers to some questions / 7. differential diagnosis / 104. differential diagnosis of heart murmurs
By origin S. sh. are usually divided into organic, associated with defects or aneurysm of the heart or vessels extending from it, and functional, caused, for example, by accelerating blood flow, reducing its viscosity, incl. and so-called innocent heart murmurs, often detected in healthy people, especially in children and young people.
In relation to the phases of the cardiac cycle ( Fig. 2, 3
) heart murmurs are divided into systolic, i.e. heard between the 1st and 2nd heart sounds (in the systole phase), and diastolic, heard in the diastolic pause between the 2nd and 1st heart sounds. S. sounds that occur during systole and continue after the second heart sound are called systolic-diastolic murmurs. Depending on what part of systole or diastole the noise occupies - initial, middle, final (late), it is designated as proto-, meso- and telesystolic (or proto-, meso- and telediastolic), respectively, and if it is heard from the beginning until the end of the pause - as pan-, or holosystolic (respectively, pan-, or holo-diastolic). Telediastolic murmur is more often called presystolic.
Listened S. sh. can be short and long, increasing, decreasing, increasing-decreasing (on a phonocardiogram - diamond-shaped, spindle-shaped), etc. In terms of pitch and timbre, the noise can be rough, gentle, blowing, scraping, sawing, rumbling, musical. The loudness of the murmur depends on many conditions, so in itself it cannot be a characteristic of the severity of a defect or other heart lesion. In thin people with a thin chest wall, as well as in children, murmurs are louder than in obese people. Pulmonary emphysema reduces the sonority of noises due to the air gap separating the heart from the anterior chest wall. In heart failure, the intensity of many murmurs caused by organic valve disease decreases, and sometimes these murmurs even disappear. Volume of diastolic S. sh. decreases with tachycardia (due to shortening of diastole); these noises usually disappear when the heart rate exceeds 100 per minute
. Due to respiratory fluctuations in cardiac output, the intensity of S. sh. may vary according to the phases of breathing; Intracardiac murmurs, both valvular and extravalvular, sharply weaken when straining after a deep breath. During physical exertion, mental excitement, fever, when the speed of blood circulation increases, the strength of S. sh. usually increases; in this case, it is often possible to listen to noises that are not detectable under normal conditions. S. sh. caused by valve defects, are best heard in a horizontal position of the patient, but in general they are less dependent on changes in body position than functional noises.
Diagnostic value of heart murmurs
. Murmurs that occur with heart defects have characteristics of origin and sound that reflect the nature of the pathology. Depending on the type of defect, the murmur is formed in certain phases of the cardiac cycle, so determining the phase of the cardiac cycle in which the murmur is heard has diagnostic significance.
Systole-diastolic murmurs occur when there is a septal defect in the heart or a shunt between large vessels. The most common cause of this noise is a patent ductus arteriosus.
.
The noise begins immediately after the first tone ( Fig. 3, f
) with a slight deviation from it. As the pressure in the aorta increases, the volume of the noise increases. The pressure gradient between the aorta and the pulmonary trunk reaches a maximum at the end of systole, and at the same time the maximum sound of the murmur is noted. It ends in the middle or at the beginning of diastole. The noise is often accompanied by shaking. Gromkiy S. sh. heard over the entire region of the heart, but has maximum intensity in the second left intercostal space, from where it radiates to the third intercostal space; When the patient is lying down, the noise intensifies. An aneurysm of the sinus of Valsalva, when it ruptures into the right ventricle, is accompanied by a systolic-diastolic murmur, which is heard to the left of the sternum. The diastolic component of the murmur is louder than the systolic component.
Systolic murmurs are heard most often, because formed in a variety of heart diseases, including myocarditis, cardiosclerosis, cardiomyopathy, as well as anemia and hyperkinetic syndrome; they make up the largest portion of “innocent” noises in practically healthy individuals and, in addition, can be important auscultatory symptoms of the most common valvular heart defects - insufficiency of the atrioventricular valves or stenosis of the aorta or pulmonary trunk (see.
Acquired heart defects
), as well as septal defect of the heart.
In mitral regurgitation, systolic murmur occurs due to regurgitation of blood from the left ventricle into the left atrium. It begins immediately after the weakened first sound and decreases towards mid-systole ( Fig. 3, a
), but often continues until the beginning of the second tone, i.e.
happens pansystolic. The noise may have the same intensity throughout the entire systole, but may intensify towards the end of it, often having a blowing character. Damage to the papillary muscles during acute myocardial infarction
, traumatic separation of the papillary muscles leads to the formation of acute mitral regurgitation; in this case, a rough and prolonged systolic murmur is heard, which begins with separation from the first tone, has a diamond shape, and is sometimes carried out to the vessels of the neck and into the interscapular space. Telesystolic (late) murmur is often heard in patients with atherosclerotic cardiosclerosis, with sclerotic degeneration of the papillary muscles, as well as with mitral valve prolapse.
The systolic murmur of tricuspid regurgitation is better heard at the base of the sternum, often intensifies at the height of inspiration and often has varying intensity, in contrast to the stable murmur of mitral regurgitation. Inconsistency of noise is more typical for relative tricuspid insufficiency. As the patient's condition improves, the sound of organic failure does not change or even intensifies due to increased contractility of the right ventricular myocardium, while the sound of relative failure becomes quieter or disappears.
A systolic murmur in the second intercostal space to the right of the sternum is characteristic of aortic stenosis (ejection murmur). Most often it has a diamond-shaped or spindle-shaped shape, it begins with some separation from the first tone ( Fig. 3, b
), ends before the beginning of the second sound, often radiating to the apex of the heart and carotid arteries.
The systolic murmur of aortic stenosis is usually accompanied by trembling of the chest wall determined by palpation (“cat purring”). The same systolic ejection murmur, but in the second left intercostal space, is heard with stenosis of the mouth of the pulmonary trunk ( Fig. 3, d
). Sometimes it is best heard in the third or fourth intercostal space, to the left of the sternum.
Systolic murmur with a ventricular septal defect is loud, prolonged, sharp and even rough, accompanied by tremors, the epicenter of which is in the third or fourth intercostal space, at the left edge of the sternum. The murmur usually covers the first sound and occupies the entire systole ( Fig. 3, c
), sometimes it is registered as increasing-decreasing. In a horizontal position, the noise is louder, often heard at a distance, and is carried into the interscapular space. After the introduction of mezatone, it becomes more intense; sublingual administration of nitroglycerin reduces its intensity.
With an atrial septal defect, the systolic murmur begins immediately after the first sound, it is not intense, blowing, and is accompanied by a bifurcation of the first sound. The intensity of the noise increases with physical activity, but does not reach the degree that occurs with ventricular septal defects.
Diastolic murmurs are almost always associated with organic heart pathology. Most often, diastolic murmurs are caused by insufficiency of the aortic valve or pulmonary trunk or stenosis of the atrioventricular orifices.
The diastolic murmur of aortic insufficiency begins at the very beginning of diastole, during the period of the second sound, which is often replaced or covered by this noise. The noise is high-frequency, gentle, usually blowing. The duration of the murmur depends on the severity of aortic insufficiency. With minor aortic insufficiency, the diastolic murmur is short (protodiastolic; Fig. 3, e
), it is difficult to detect, only in the absence of extraneous noise. With more severe aortic insufficiency, it occupies 1/2-2/3 of diastole and is characterized by decreasing intensity; with severe aortic defects, the murmur often occupies the entire diastole. Many researchers believe; that in severe aortic insufficiency the murmur is usually more intense. It is heard at the auscultation point of the aortic valve and at the fifth point, and is better heard with the patient lying on his stomach with calm, shallow breathing.
A fading diastolic murmur in the second (less often in the third) intercostal space to the left of the sternum is a sign of pulmonary valve insufficiency. With relative pulmonary valve insufficiency resulting from hypertension of the pulmonary circulation
, a quiet blowing diastolic murmur, called Still's murmur, is heard. It begins immediately after the second sound and is heard in a limited area in the second intercostal space on the left; in cases of bifurcation of the second tone, the noise begins from its second component.
The diastolic murmur of mitral stenosis occurs immediately after the second component of the bifurcated II tone, has presystolic amplification, often musical, and is accompanied by chest trembling. The murmur is usually low-frequency, better heard at the apex of the heart when the patient is horizontally positioned on the left side, and intensifies after physical activity. It can occupy the entire diastole; in this case, it first decreases, and then, approximately from the middle of diastole, continues with a constant amplitude until presystolic increase ( Fig. 3, e
), associated with atrial systole. This is explained by the fact that during the phase of rapid filling of the left ventricle, blood rushes at high speed through a narrow opening, creating a noise that subsides as the flow rate decreases and intensifies again with its additional acceleration associated with atrial systole. With atrial fibrillation, there is no presystolic increase in noise. Along with diastolic murmur, an increase in the first tone and a bifurcation of the second tone are detected, which creates the so-called melody of mitral stenosis.
Diastolic murmur with presystolic amplification is determined with myxoma of the left atrium (see Heart
), it is variable, its appearance and intensity depend on the position of the body and the speed of blood flow.
With severe organic aortic insufficiency, functional stenosis of the left atrioventricular orifice occurs due to the fact that the blood stream regurgitating into the left ventricle lifts the mitral valve leaflet. In this case, a diastolic murmur with presystolic amplification (Flint murmur) is heard at the apex of the heart. It is not as long and loud as with organic mitral stenosis, and is not accompanied by an increase in the first sound and the sound of the mitral valve opening.
Often, in children with mitral valve insufficiency and ventricular septal defect, with significant dilatation of the atria or ventricles, a fusiform diastolic murmur is detected,
separated by an interval from the second tone and lasting no more than 0.2 s
(Coombs noise); it is heard near the apex of the heart only in the presence of a third sound.
Diagnostic differentiation of cardiac murmurs is carried out primarily with extracardiac (paracardial) murmurs. The greatest similarity with S. sh. have pericardial friction rub, cardiopulmonary and pleuropericardial murmurs. Pericardial friction noise is detected in pericarditis, myocardial infarction, usually in the form of short scratching sounds during systole or diastole or in both phases. Cardiopulmonary (cardiopulmonary) murmurs occur in those parts of the lungs that are in contact with the heart. Changes in the size and position of the heart during systole cause rapid movement of air in the adjacent areas of the lungs, which generates high-frequency noise. Cardiopulmonary murmurs are often heard in persons with a reduced anteroposterior chest size, in young people with excited cardiac activity (the so-called hyperkinetic type of cardiac activity), as well as in cases of severe cardiac hypertrophy. They are usually heard during systole, and when breathing is held during exhalation, they usually disappear. Pleuropericardial murmurs, i.e. friction noises that occur with dry pleurisy in the areas of contact between the pleura and the pericardium intensify during inspiration. When differentiating the nature of murmurs, it is also necessary to remember about the various vascular murmurs.
Significant difficulties sometimes arise when differentiating organic and functional S. sh. To distinguish organic and “innocent” noises, various techniques (physical activity, change of body position) and pharmacological tests were proposed. Taking nitroglycerin causes an increase in the systolic murmur of aortic stenosis, a weakening of the murmur of mitral regurgitation and an increase in the systolic murmur of tricuspid regurgitation. Functional pulmonary systolic murmur is heard in the second intercostal space, at the edge of the sternum. The murmur usually has a spindle-shaped shape and occupies the first half of systole, always blowing, is better heard when the patient is lying down, and intensifies under the influence of stress and with fever. Exhalation improves the audibility of this noise. An “innocent” aortic systolic murmur occurs due to systolic vibration of the distended aortic root. It occupies mid-systole, is heard in the second intercostal space, and is usually carried out to the apex of the heart at the right edge of the sternum.
Diagnosis of the nature of the North. more accurate for dynamic noise estimation. As heart function improves, organic murmurs usually become more distinct. We can also assume that murmurs heard in the diastole phase and murmurs that occupy the entire systole are never “innocent”. If there is doubt about the nature of the noise, a comprehensive examination of the patient and dynamic observation is necessary.
Diagnosis of heart murmur
Listening to the chest is only half of the diagnosis. After it, it is necessary to determine whether there is a circulatory disorder, what its degree is and what the reason is. Therefore, the doctors at our clinic recommend undergoing the following examinations:
- electrocardiography;
- ultrasound scanning with Doppler;
- radiography, especially if left ventricular hypertrophy is suspected;
- analysis to determine hormonal status (primarily thyroid);
- general clinical blood test.
It should be remembered that only a competent doctor can identify a heart murmur, as well as determine the cause of its occurrence. Therefore, you need to contact clinics that employ doctors who are interested in innovations in cardiology, for example, the Med-Lite medical center on Narodnogo Opolcheniya Street 23k3.