Heaviness in the legs is a familiar feeling to many people, regardless of gender, age and type of activity. Heaviness in the legs is a subjective characteristic of such manifestations as: discomfort and a feeling of heaviness in the legs, a feeling of fullness and nagging pain in the calf muscles, swelling.
This feeling may be experienced by:
- children and young people who are in a period of active growth of the musculoskeletal system,
- elderly people and old people,
- athletes after long training sessions,
- pregnant women,
- overweight people.
Very often, heaviness in the legs bothers people whose profession involves heavy physical exertion and heavy lifting, staying in one position for a long time, sitting or standing, for example, office workers, doctors, teachers, drivers, and so on.
Heaviness in the legs can be a transient condition: the discomfort disappears after a night's rest, massaging the legs, a contrast shower, a short stay in the “legs above the body” position, or permanent. Regular complaints of heaviness in the legs are an “alarm bell” signaling problem veins and a serious reason to consult a phlebologist. Diagnosis of venous insufficiency at an early stage, individually selected therapy, carried out under the supervision of a specialist, is the only way to avoid further development of varicose veins.
What is heaviness in the legs
The feeling of heaviness in the legs is quite common. After a day spent on their feet, many noted the appearance of this symptom. According to modern statistics, for 30% of the world's population, heavy legs are a constant companion. The legs “hum”, “ache”, there is constant fatigue in the lower extremities; these symptoms also occur in most patients with venous pathology.
Heavy legs
When the ground disappears from under your feet
Often, pain in the legs is a manifestation of diseases of the arteries or veins of the lower extremities (diseases of “inflow” and “outflow”), but it can also be caused by diseases of the spine, nervous system and metabolism. Pain can occur when bones and joints, muscles and tendons, lymph nodes and blood vessels are affected. Such a dangerous disease as diabetes sometimes begins with pain in the legs. And only then are elevated blood sugar levels and other manifestations of diabetes detected. At the beginning, the legs hurt, muscle cramps, weakness in the legs, and dry skin occur. But a terrible complication is not far off - “diabetic foot”. But in advanced cases, this pathology can lead to amputation of the lower limb.
The legs swell, the skin on the legs becomes dry, irritated, constantly itchy and flaky. It happens that pain in the calf muscles and cramps bother you, especially at night. Often the legs become numb, cold, and so-called paresthesia occurs - abnormal sensations associated with damage to nerve endings. This may be a feeling of “crawling goosebumps”, tingling, pinching, etc. The greater the vertical load during the day, the more pronounced the painful manifestations in the evening. But the pain can also be constant, regardless of the time of day. It happens that pain, having already become a familiar companion of life, suddenly suddenly changes its character. Acute pain in the leg may indicate a vascular accident when a blockage of a large artery develops. In this case, there are only a few hours during which there is a chance to save the leg deprived of nutrition and oxygen.
Causes of heaviness in the lower extremities
The cause of heaviness in the legs is congestion due to impaired venous outflow. The most intense symptom of heaviness in the legs appears in the evening.
Why does heaviness appear in the legs:
- Continuous static load. This is relevant for those professions where a person is forced to stand most of the time (surgeons, teachers, hairdressers). Also, office workers, where a person spends a long time in a sitting position, are susceptible to the symptom of heaviness in the legs.
- Physical inactivity and increased body weight.
- Hormonal changes. This situation concerns, first of all, women.
- Pregnancy. Increased pressure in the abdominal cavity due to fetal growth often leads to a slowdown in venous outflow of the lower extremities.
The leading cause of heaviness in the legs is varicose veins. Violation of the outflow of venous blood leads to its stagnation in the distal parts of the lower extremities. The feeling of heaviness with varicose veins is long-lasting. The heaviness does not go away even after a night's rest and the legs do not fully recover. Elastic compression will have a good effect in relieving the severity of varicose veins. However, this effect will be temporary. For a good long-term solution to the problem of heaviness in the lower extremities, you need to consult a specialist, a phlebologist.
Varicose veins are the main, but far from the only reason for the development of heaviness in the legs. Heaviness in the legs can also be a symptom of the following pathological conditions:
- Lymphedema. This pathology of the lower extremities is caused by a violation of the outflow of lymphatic fluid.
- Violation of the arch of the foot (longitudinal and transverse flat feet). Due to a non-physiological setting, the musculoskeletal and vascular systems of the lower extremities experience additional stress. This leads to a feeling of heaviness and swelling in the lower extremities.
- Cardiac pathology. This group of diseases affects both arterial and venous blood flow. Most patients with heart pathology note increased heaviness in the legs. Heart diseases.
- Kidney diseases. Heaviness in the legs is caused by excess fluid in the soft tissues, including the lower extremities.
Let's take our feet in our hands soon!
Traditional medicine is replete with advice that is mainly aimed at reducing swelling and improving nutrition of the skin of the legs. Unfortunately, in most cases, this helps only in the very initial stages of the disease. But the early manifestations of the disease are the “golden” time for its timely, correct and complete treatment. What a shame that in almost 95% of cases this moment is missed!
Before trying out a new foot cream, you need to ask yourself: “Isn’t it time to see a specialist?” After all, the sooner the examination is started and the true cause of “heavy” legs is established, the greater the chance of quickly starting treatment for the underlying disease and thereby preventing the development of serious complications.
The most effective diagnosis for discomfort or pain in the legs is a comprehensive examination that takes into account all possible causes of the disease. In addition to examinations of internal organs and laboratory tests, ultrasound scanning of the arteries and veins of the lower extremities is mandatory. With this study, the doctor can identify atherosclerotic damage to the arteries, determine the degree of narrowing of the lumen of the vessel, and identify areas of “blockage” of the arteries. Angioscanning allows you to visualize veins (superficial and deep) along their entire length, determine the degree of “blockage” of the vein, and identify the presence of such a dangerous complication of thrombophlebitis as “floating thrombosis,” in which there is a high probability of a blood clot breaking off with the development of pulmonary embolism.
It is also advisable to conduct a study of the endocrine system responsible for regulating calcium levels. After all, the lack of calcium in the blood is replenished by bones and teeth, which can lead to severe osteoporosis, cramps, pain in muscles and joints. An ultrasound examination of the pelvic organs (uterus, ovaries) and prostate gland (in men) is also necessary. Ultrasound allows us to exclude diseases of these organs, because their enlargement can lead to compression of large vessels responsible for blood circulation in the lower extremities. A blood test for nonspecific inflammatory factors will help the doctor identify the presence of inflammatory processes in the veins (phlebitis) and arteries (arteritis).
Frequently asked questions from patients about heavy legs
Heaviness in the legs, reasons why it occurs?
There are many reasons known to modern science for the feeling of heaviness in the legs. In addition to diseases, the cause may be uncomfortable shoes and prolonged static loads. The main cause of pathological severity in the lower extremities is varicose veins.
Swelling and heaviness in your legs appear, what should you do?
If you have swelling and heaviness in your legs, you need to visit a phlebologist and perform a duplex ultrasound examination of the venous system of the lower extremities. Evening swelling and a feeling of heaviness may be the first signs of serious venous pathology.
What is the cause of heaviness in the legs below the knee?
The most likely cause of heaviness in the legs is chronic venous insufficiency, as a consequence of varicose veins. It is this pathology of the venous system that causes a feeling of heaviness in the lower extremities in hundreds of millions of people around the world every day.
How to get rid of heavy legs?
In order to get rid of heaviness in the lower extremities, you need to eliminate the cause of this condition. Any treatment must begin with diagnosis. You need to go to a good phlebological center, see a competent phlebologist and follow the specialist’s recommendations.
Diagnostics
Considering that most cases of heaviness in the legs are associated with venous circulation disorders, an examination by a phlebologist is necessary. Often, a preliminary diagnosis is made during an objective examination, when varicose veins, edema, hyperpigmentation, and other typical manifestations are detected. To clarify the diagnosis and identify other etiological factors causing heaviness in the limbs, the following is carried out:
- Doppler ultrasound of veins
Duplex scanning of vessels is used to study the anatomical structure of the venous bed, assess the tone and function of the valves. Chronic venous insufficiency is manifested by slow blood flow, pathological blood reflux, and phlebothrombosis. - Rheovasography of the lower extremities.
A modern diagnostic method that shows even minor changes in hemodynamics and microcirculation. Based on the results of the study, the doctor gives an opinion on the condition of the peripheral veins during stress tests and at rest. Sometimes venography is prescribed for additional examination of blood vessels. - Lymphangiography.
Visualization of lymphatic vessels using a contrast agent is required to determine their patency and the functioning of the valve apparatus. The difference in diameter in different parts of the vessels and uneven contrast indicate pathology. For dynamic assessment of lymph circulation, lymphoscintigraphy is indicated. - X-ray of the foot.
If flat feet are suspected, an orthopedic traumatologist joins the diagnostic search. Based on X-ray images, the doctor measures the height of the arches and pathological angles between bone structures, establishes the type and severity of the disease. The diagnosis is clarified using plantography. - Additional research
. To diagnose osteochondrosis, which causes heaviness in the legs, an x-ray or computed tomography scan of the spine is performed. To confirm cardiac diseases, ECG, echocardiography, and chest X-ray are recommended. Survey and excretory urography are informative for excluding renal causes of edema.
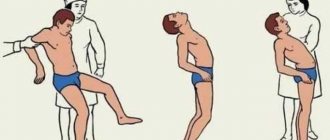
Phlebologist consultation
Contrast for fatigue: contrast baths
Everyone has heard that a contrast shower invigorates the body.
But this technology can also be applied locally. Contrast foot baths are a great way to relieve fatigue, improve blood circulation, and cleanse the skin. In addition, contrasting temperatures help to increase the tone of the body as a whole, activating the central nervous system and boosting the immune system. How to make foot baths:
- Pour two basins of water at different temperatures: warm (no more than 42°C) and cool (no less than 10°C). It is recommended to start with medium temperatures: 36 °C and 22 °C.
- Immerse your feet up to your ankles, first in warm (50-60 seconds), then in cold (20-30 seconds) water.
- Repeat the procedure at least 10 times.
You can also use hot and cool baths separately. Hot ones are suitable if your feet are cold or heavy, and cool ones are suitable when you need to relieve fatigue and pain. It is better to increase the temperature of the hot bath gradually, this way you will contribute to the gradual dilation of blood vessels.
Preventing the development of heavy leg syndrome
food
Useful foods to prevent heavy leg syndrome
If you have the first signs of varicose veins, correct lifestyle and nutritional adjustments, combined with adherence to medical recommendations, will help return your legs to normal health. To achieve this, follow a few simple rules:
- Avoid wearing high heels frequently.
- It is recommended to make it a rule to do feasible physical exercises every day: stand on your toes, do “bicycle” and “scissors”, go swimming. At the same time, strength exercises with large weights, squats and jumps should be abandoned.
- If you are forced to spend a long time in a static position (for example, during a long air flight), periodically strain your calf muscles and lift your heels and toes off the floor. Literally a few of these mini-exercises can improve blood flow in the veins of the legs.
- Adjust your daily diet so that it contains foods rich in coarse plant fibers: these can be fresh vegetables, herbs, and fruits.
- Don't forget about your drinking regime: you need to drink at least 2 liters of clean water every day (this does not include tea, juices, broths).
- Avoid drinking alcohol, strong coffee, smoked and salty foods, trans fats, baked goods and bread, milk and dairy products, and sugar. Instead of these products, include vegetables, fruits and berries, legumes, sea fish and seafood, vegetable oils, nuts and seeds in your diet.
- Normaven® can be used to prevent the development of heavy leg syndrome. For example, Normaven® Foot Tonic is a great help for tired feet. The product has a beneficial effect on the blood vessels of the lower extremities, helping to cope with the feeling of heaviness and fullness that appears at the end of the day or during prolonged sitting. The toner contains natural ingredients: extracts of chestnut, witch hazel, butcher's broom, as well as menthol and panthenol. Highly qualified specialists, employees of the pharmaceutical company VERTEX, worked on the development of the product. Leg tonic Normaven® has a full package of relevant documents and certificates and is recommended for use in the initial stages of varicose veins development.
Heavy Leg Syndrome: Treatment
Heavy leg syndrome, treatment
If you experience the symptoms described above, do not delay a visit to a phlebologist. Self-medication is highly discouraged - it is better to trust specialists in the matter of therapy. The diagnosis is made based on a visual and physical examination of the patient, as well as data obtained from vascular ultrasound and duplex angioscanning.
To return blood vessels to normal tone and normalize valve function, the following methods are used:
- The use of phlebotropic drugs. These products help strengthen the walls of blood vessels and increase their elasticity, reduce swelling of the lower extremities and reduce their pain.
- Wearing compression garments. Special stockings, stockings and tights exert graduated pressure on the veins of the legs, normalizing the speed of blood flow and reducing swelling of the lower extremities.
- Surgical intervention. If the disease is at an early stage of development, laser or sclerotherapy is used to eliminate spider veins and spider veins. If the pathological process has reached an advanced stage, the patient may be recommended to undergo phlebectomy - surgical removal of areas of altered veins. Elective surgery is not performed in pregnant women, with severe arterial hypertension, deep vein thrombosis and certain heart diseases.
- Minimally invasive methods for treating heavy leg syndrome. If open surgery is not performed for any reason, and drug therapy has proven to be ineffective, methods for treating varicose veins without surgery are prescribed. For example, this could be sclerotherapy or radiofrequency ablation.
Video: Restless legs syndrome
is not responsible for the accuracy of the information presented in this video clip. Source – JitZdorovo
Sources:
- RESTLESS LEGS SYNDROME: PATHOGENESIS, DIAGNOSIS, TREATMENT. LITERATURE REVIEW. Kovalchuk M.O., Kalinkin A.L. // Neuromuscular diseases. – 2012. – No. 3. – P. 8-19.
- RESTLESS LEGS SYNDROME. Chamsaev M.A., Ivanichev G.A., Boyko S.P., Gainutdinov A.R., Staroseltseva N.G. // Kazan Medical Journal. – 2003. – No. 3. – pp. 186-193.
- MEDICAL REHABILITATION OF PHLEBOLOGICAL PATIENTS. Zhukov B.N., Katorkin S.E., Kostyaev V.E., Kostyaeva E.V. // Bulletin of new medical technologies. – 2009. – No. 4. – pp. 76-79.
- https://www.medicalnewstoday.com/articles/321670.php
- https://ru.scribd.com/document/13164531/Heavy-Leg-Syndrome-Article
For an accurate diagnosis, contact a specialist.