- What does upper and lower pressure show?
- What can lead to a decrease in lower pressure?
- Types of arterial hypotension
- Causes
- Mechanisms of reduction in systolic and diastolic pressure
- Symptoms
- Diagnostic procedures
- Treatment methods
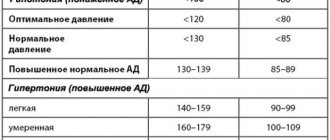
The state of low blood pressure is called arterial hypotension. It occurs if the readings fall below 100/60 mmHg. In some patients, upper and lower pressure (systolic and diastolic) decreases. Sometimes a situation arises when the upper indicator is normal, and the lower indicator falls below normal. This is regarded as isolated arterial hypotension and requires the attention of specialists.
What does upper and lower pressure show?
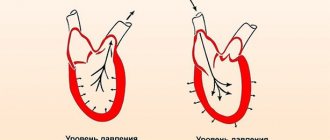
The upper pressure is called systolic. It refers to the force with which blood is pushed out of the heart and moves through the vessels, saturating organs and tissues with oxygen. Diastolic - lower pressure, indicates the pressure of blood on the walls of blood vessels at the moment between heartbeats.
As a rule, as people age, they experience an increase in upper blood pressure. Elevated lower levels are more common in patients under 50 years of age and then begin to decline. Problems with diastolic pressure begin due to deterioration in the elasticity of blood vessels. The capillaries narrow, become stiffer, and this leads to excess blood pressure on their walls. This phenomenon is observed even at rest.
Why is this condition dangerous?
The dangers are identical to those of classic hypotension. Possible risks include:
- Stroke. As a result of insufficient blood circulation in the brain. Weak heart function simply does not allow sufficient oxygen and nutrients to be provided to the tissues.
It can develop independently or as part of Morgagni-Adams-Stokes syndrome (in approximately 10% of clinical cases in patients with a decent history of hypotension).
- Impaired cognitive functions up to severe dementia of the schizophrenic type, when the intellect remains intact, but the patient cannot use it.
- Mental disorders such as vascular psychoses with hallucinatory and hallucinatory-delusional syndromes. They are similar in nature to schizophrenic or alcoholic syndromes.
- Increased risk of heart attack due to congestive heart failure in patients with similar phenomena.
Other pathological consequences are also possible. It all depends on the duration of the disease.
What can lead to a decrease in lower pressure?
Arterial hypotension can act as an independent disease (primary form) or one of many symptoms (secondary form). According to statistics, low upper and/or lower blood pressure is more common in women than in men. This phenomenon can also occur in adolescents.
In older people, lower blood pressure decreases due to decreased vascular tone. The main culprit of the problem is atherosclerosis. Secondary hypotension can occur against the background of neurological and cardiac diseases, and hormonal disorders.
Prevention
Preventive methods consist of preventing stressful, nervous and emotional situations, and excessive overexertion. It is recommended to avoid nervous shock if possible. Using supplements rich in vitamin B will help reduce the risk of the problem. These vitamins strengthen blood vessels and help cope with stressful situations. To strengthen the heart, magnesium and ascorbic acid preparations are prescribed.
If a problem with low blood pressure occurs, it is necessary to adjust your diet and lifestyle. It is necessary to include foods with a high sodium content in the menu. These include sauerkraut, sea fish, and seafood. It is recommended to include chocolate, cocoa, hot spices, fresh fruits and vegetables in your diet. It is worth using physical activity. For better sleep and strengthening the body, a 30-minute walk in the fresh air is recommended.
Types of arterial hypotension
There are three types of arterial hypotension:
- physiological;
- pathological;
- symptomatic.
Low blood pressure as a physiological norm may be a congenital feature characteristic of a particular person due to his constitutional type. A similar situation is observed among professional athletes, residents of high mountain areas and tropical latitudes. Thanks to the decrease in pressure, the body adapts to physical activity and climate conditions. In this case we are talking about a compensatory function.
The pathological form of the disease is of two types: orthostatic and neurocirculatory. Orthostatic hypotension occurs when there is a change in body position when a person gets up after resting or sleeping. The neurocirculatory form is associated with disruption of the autonomic nervous system. The patient may periodically experience low blood pressure or have hypotension, in which diastolic pressure is chronically low.
Symptomatic hypotension is secondary. Its causes are disruption of the functioning of various organs and systems, intoxication.
Normalization of indicators
If there is a constant decrease in blood pressure, you should contact a cardiologist or therapist for a general diagnosis. Most often, treatment is based on preventive methods and is rarely supplemented with drug therapy. Help normalize low blood pressure:
- caffeine;
- strong tea;
- cold and hot shower;
- healthy sleep;
- proper nutrition;
- morning exercises.
The following drugs are effective:
- "Citramon";
- "Heptamil";
- "Regulton".
The use of any tablets to increase blood pressure should be done only after consultation with the attending cardiologist.
Causes
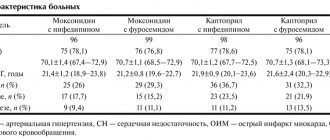
According to statistics, the main cause of primary hypotension is neurocirculatory dystonia (NCD). It is otherwise called heart neurosis. With neurocirculatory dystonia, various disorders of autonomic regulation are observed, and this condition is not associated with damage to the endocrine or nervous systems.
NCD and the resulting decrease in diastolic pressure are most often observed in women during puberty and at the onset of menopause, with impaired ovarian function. In young people and middle-aged patients, hypotension occurs against the background of chronic fatigue, stress, psycho-emotional and physical overload. The high-risk group includes people with alcohol and tobacco addiction, patients who have recently experienced psychological trauma, and who are depressed.
Secondary arterial hypotension can be acute or chronic. Low diastolic pressure is encountered by patients with stomach ulcers, diabetes, low thyroid function, osteochondrosis, arrhythmia, heart failure, and chronic infectious processes. In people with such diseases, blood pressure may be constantly low, but due to the body's ability to adapt, the disease does not manifest itself with pronounced symptoms.
A sharp drop in upper and lower blood pressure occurs with significant blood loss, dehydration, anaphylactic shock, or poisoning. These conditions are extremely dangerous for health and life, as they lead to serious circulatory disorders.
One of the possible reasons for a decrease in diastolic blood pressure is a lack of vitamins B, C and E in the diet. The body can also respond to a strict diet or an overdose of drugs (adrenergic blockers, anti-hypertension drugs) with arterial hypotension.
Features of treatment at home
Doctors consider the main way to correct hypotension to be the correct daily routine, a balanced diet, physical activity, and everything that is commonly called a healthy lifestyle. Let's figure out how to quickly raise low heart pressure and what medications are used at home. Dietary supplements, adaptogens, herbs in this case play a supporting role.
Medications
We offer you the top nine medications that increase cardiac (systolic or upper) blood pressure:
| Drug name | Blood Pressure Promoting Properties |
| Caffeine-containing: Acepar, Citramon, Pentalgin-N | Tones blood vessels, increasing blood pressure |
| Psychotonics: Sydnofen, Mesocarb, Mexidol, Sydnocarb | Activate the adrenergic system |
| Analeptics: Cordiamine, Centedrine | Stimulates the vascular center |
| Adrenergic agonists: Gutron, Regulton, Fetanol, Mezaton | Stimulate adrenergic receptors, narrowing arteries, reducing blood flow |
| Spinal cord stimulants: Securinine, Strychnine | Affect the centers that control the lumen of the arteries |
| M-anticholinergics: Bellaspon, Belloid | Block the interaction of cholinergic receptors with acetylcholine |
| Nootropics: Piracetam, Pantogam | Improves metabolism in the central nervous system and regional blood circulation |
| Energizers: Potassium orotate. L-carnitine, Lipocerebrin | Reanimate cells, activate redox processes |
| Vitamins: C, A, group B, Pikovit, Alphabet, Vitrum, Complivit | Improves metabolic processes, exhibits antioxidant effects |
Mechanisms of reduction in systolic and diastolic pressure
A decrease in blood pressure is caused by one of four possible reasons:
- the stroke and cardiac output decreases;
- the flow of blood to the heart through the veins decreases;
- vascular resistance decreases;
- the volume of circulating blood decreases.
A decrease in cardiac output and stroke is observed in cases of disturbances in myocardial function caused by infarction or myocarditis. The same situation occurs with an overdose of adrenergic blockers.
Vascular tone can decrease with infectious diseases, intoxication, and anaphylactic shock.
A decrease in the volume of circulating blood occurs against the background of bleeding due to trauma to tissues and blood vessels, rupture of the spleen, and ulcerative lesions of the stomach.
A decrease in venous return of blood to the heart occurs with massive ascites or pleurisy due to blood retention in the smallest vessels.
Symptoms
With a physiological decrease in lower pressure, patients do not experience a deterioration in their well-being. If the problem is caused by pathology, then oxygen starvation gradually develops. It is characterized by the following symptoms:
- weakness and dizziness;
- colored spots before the eyes;
- pallor;
- fainting state.
Patients with chronic arterial hypotension constantly feel fatigue, drowsiness, and a desire to rest. A person with low blood pressure experiences increased sweating and may experience headaches. Low blood pressure makes it difficult to concentrate on work or study and makes a person emotionally unstable. Women with chronic hypotension may experience menstrual irregularities, and men have reduced potency.
In severe forms of arterial hypotension, patients experience vegetative crises. They are accompanied by a decrease in temperature, sweating, difficulty breathing, chest pain, nausea and vomiting, slow pulse, and loss of consciousness.
conclusions
Hypotension is determined when the pressure drops below 120/80 mmHg; it can be either normal or pathological. There are possible cases when only one indicator decreases - SBP, while the upper pressure is low and the lower pressure is normal. Symptomatically manifested by general weakness, increased fatigue, attacks of headache and dizziness. Often occurs after physical or psycho-emotional fatigue. It may be a sign of a cardiac or concomitant disease, and requires a comprehensive examination. Based on the conclusion, the doctor prescribes drug therapy and gives recommendations on normalizing the daily routine and rest.
Diagnostic procedures
To normalize blood pressure, it is important to identify the reasons for its decrease. The approach to diagnosing arterial hypotension is complex. First of all, the doctor needs to assess the blood pressure level. Daily monitoring is best suited for these purposes. The procedure helps to identify how pressure readings change during the day. A technique for measuring blood pressure three times with an interval of 3-5 minutes is also used.
To choose treatment, you need to determine whether a decrease in lower pressure is an independent disease or a symptom of another disease. The patient is prescribed laboratory tests for hormones, electrolytes, glucose and other indicators. Among the hardware methods for diagnosis, electroencephalography, ECG, and orthostatic test are used.
A person with chronic arterial hypotension needs to consult a neurologist, cardiologist, or endocrinologist.
Diagnostics
Cardiology specialists are involved in the examination and management of patients with low upper blood pressure.
In case of non-cardiac origin of the pathology, consultation with an endocrinologist or neurologist is recommended. In extreme cases - a nephrologist.
Diagnostic methods include:
- Study of complaints and anamnesis to make a primary diagnosis and its further verification (confirmation).
- Assessing the state of cardiac activity by studying the frequency of contractions of the organ. The old ancient method with a stopwatch or the modern one with an automatic tonometer is used.
- Measuring blood pressure on both arms. Assessment of cardiac activity using an electrocardiograph. Most informative
- method.
- Daily monitoring of Holter pores. Shows how pressure changes over 24 hours.
- It is important to examine the blood for the amount of hormones of various origins.
- Urinalysis, general blood test, venous blood test, these methods are necessary to assess the general condition of the body. Specific indicators are possible.
- Ultrasound of the kidneys.
Other studies are also possible at the discretion of the group of specialists.