In the Russian Federation, 7% of adults suffer from chronic heart failure (CHF). Every year, even in conditions of treatment in a specialized hospital, up to 12% of patients with clinically significant CHF die. The only thing that can help a patient in the terminal stage of this disease is a heart transplant.
Not everyone who needs surgery lives to see it, but since Dr Christian Barnard's team performed the world's first human-to-human heart transplant 46 years ago, there has at least been hope for recovery.
Why is there not enough donors in Russia?
And even with the existing presumption of consent, Russia has a catastrophic shortage of donors.
The wait for a kidney can last for many years. On an artificial heart, which is suitable only for a few, a person can survive for a year, two or even three. And severe complications result in high mortality. At the same time, lung and pancreas transplants still remain very rare operations. But one donor can save at least eight lives. “We have only 32 regions involved in transplantation, and we are now bending over backwards to increase their number. We travel around the regions, talk with hospitals and administrations. We say that the organ resource is disappearing - people are waiting for these organs. We cannot talk about deficit as such. It is correct to talk about the lack of administrative resources for organizing donor programs,” assures Sergei Gauthier, director of the National Medical Research Center for Transplantology and Artificial Organs.
There is no liability for hospitals where donors appear. No one will suffer any punishment if a person does not become a donor, although he could become one.
— Transplantologists are people who would like to have this resource to save the population. But we cannot organize this process. This is the responsibility of the chief doctors of hospitals where the death of certain patients is declared. This mechanism works with great difficulty,” says the doctor.
His colleague Alexander Chernyavsky is convinced that the reason lies in the fact that such hospitals have no interest in developing donation.
— There are laws, the regulations have been adopted. But failure to comply with them is not punishable by anything, no one is responsible for this - for the fact that we do not have enough donor organs,” Alexander Chernyavsky is dissatisfied. — We calculated how many potential donors there could be in Novosibirsk, for example. There are certain formulas that are known all over the world and are used for calculations. And in Novosibirsk we have approximately 50 to 70 real donors per year. I think in this case we could generally solve the problems with providing care to patients with kidney failure. This is approximately 140 kidney transplants per year.
If we consider this issue only from a financial point of view, then experts convince us that organ transplantation is much more profitable for the state than the same dialysis that patients with kidney failure must undergo.
“If our donor bases worked effectively and efficiently enough, we could abandon dialysis altogether. We think only about immediate costs, and when we look at the fact that this patient needs to undergo dialysis for 10–15 years, we understand that these are huge sums. They add up to billions of rubles. A patient who receives a kidney transplant costs the state several times less. And this has been calculated for a long time. We don't know how to count money at all.
Modern statistics
To date, more than 15,000 heart transplants have been performed worldwide. The 10-year survival rate for patients is about 50%. The highest mortality rate is in the first year after surgery (in different clinics - from 15 to 25%). The main causes of death are infectious diseases and Kaposi's sarcoma, which develop during immunosuppressive therapy.
Happy cases have also been described in which patients with a transplanted heart lived for more than 25 years. The world record holder was Tony Huseman, a patient at the Stanford University Clinic. He was operated on in 1978, the indication was dilated cardiomyopathy. After the transplant, he lived for 30 years and died at 51 from skin cancer.
From 2.7 to 4.5 thousand heart transplants are performed annually in the world. Of these, only about 100 operations are in Russia. The leader in the number of transplants is the United States: up to two thousand heart transplants are performed there annually.
Today in Russia there are 10 centers performing heart transplantation (all data are presented in accordance with information published in the journal “Bulletin of Transplantology” for 2009–2013).
Indications for heart transplant surgery
Diagnosis:
— cardiomyopathies of various origins;
- benign heart tumors;
- inoperable congenital heart defects (for example, left ventricular hypoplasia).
Clinical and functional characteristics of patients:
— chronic heart failure of NYHA class III-IV, resistant to drug therapy;
— ejection fraction of LVS < 30%;
— end-diastolic size of the left ventricle > 7 cm;
— LVA end-diastolic pressure > 20 mm Hg. Art.
— cardiac index (CI) < 2.5 l / (min × m2);
- refractoriness of ventricular tachyarrhythmias;
— expected survival of a potential recipient without heart transplantation < 6–12 months;
- age up to 55 years.
Absolute contraindications:
- persistent pulmonary hypertension (transpulmonary pressure gradient > 15 mm Hg, total pulmonary resistance (TPR) > 5 Wood units, systolic pressure in the pulmonary artery more than 60 mm Hg);
- acute infectious diseases and/or exacerbation of chronic ones;
- irreversible multiple organ failure;
- history of malignant neoplasms;
- thrombophlebitis;
- systemic diseases;
— obesity (> 30% of proper body weight);
- mental illness, alcoholism, drug addiction;
— lack of discipline in taking medications, non-compliance with hospital regulations.
Relative contraindications
- active diffuse myocarditis;
- insulin-dependent diabetes mellitus;
- peptic ulcer of the stomach and duodenum in the acute stage;
- history of cerebrovascular accident;
— infection with hepatitis C and hepatitis B viruses;
- atherosclerosis of the vessels of the lower extremities;
- limited family support.
Pediatric transplantation and minor donors
The most difficult issue of transplantation in Russia remains child donation. By law, it is permitted with parental consent, but so far there has not been a single minor donor in our country. If a child needs a liver or kidney, doctors can transplant them from an adult donor or even from relatives. But in the case of a heart transplant, everything is much more complicated. The child must grow to the point where he can be saved with the help of an adult organ. And this is an age of approximately 12–14 years and older.
— During heart transplantation, we greatly depend on anthropometric parameters. If we have a teenager weighing more than 30 kilograms, this usually allows us to place the heart of an adult deceased in the chest and solve the problem,” says Sergei Gauthier, chief freelance transplantologist at the Ministry of Health of the Russian Federation. “But if we are talking about a small child, then we are simply powerless.” Despite the fact that everything is spelled out in the law and there is an order from the Ministry of Health, we are absolutely blocked by the actions of pediatric resuscitators. Many parents understand the need for organ removal. You can talk to them about it. But pediatric resuscitators experience mental frustration about this. They cannot cross the threshold of declaring the death of a child for subsequent donation.
Taking an organ or part of it from relatives, although it saves lives, can be dangerous for the donor himself. He will have to live without one kidney or part of his liver. According to doctors, such operations cannot take place without leaving a trace. That is why experts insist on the development of posthumous donation.
— The biggest advantage of related transplantation is the independence of this procedure from the presence of an organ from a person who has died. This operation can be planned and carried out within a specific time frame. This is the biggest plus,” explains Ivan Porshennikov, head of the organ transplantation department of the Novosibirsk Regional Clinical Hospital. — The biggest disadvantage is that a living, healthy, innocent person can die during the removal of a fragment of an organ. The risks of this event are extremely low, but nevertheless, this has happened in world practice. This is a statistic and there is no escaping it. The most correct way in transplantation is the development not of related transplants, but of organ donation.
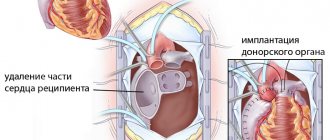
Preparing the patient for surgery
Heart transplantation is a complex procedure that requires careful preparation. The patient undergoes a multi-stage examination before a decision is made about the possibility of organ transplantation. Necessary:
- carefully collect anamnesis of the disease;
- perform a chest x-ray;
- take a maximal oxygen uptake (VO2) stress test;
- undergo a series of tests for infections to exclude hepatitis, HIV and a number of other diseases that may be a contraindication;
- undergo routine urine and blood tests to assess the general condition of the body;
- undergo cardiac catheterization with tonometry of the right side (necessary to exclude pulmonary hypertension, which will be a contraindication to transplantation);
- take a test to evaluate human lymphocyte antigen (HLA);
- undergo an ECG, EchoCG.
The examination may reveal both absolute and relative contraindications that exclude the patient from being placed on the waiting list for a donor heart.
Is there a chance for change? What will the new law change?
The current law on transplantation was adopted almost 30 years ago. And there are many gaps in it, which also turn people against transplantation. The new law should create a single waiting list throughout the country, as well as a register of refusals and consent for posthumous donation. This should make the system more transparent - both for patients and doctors. And also the law should completely exclude situations where an organ was taken after the death of a person who did not want it.
The document also defines the time during which relatives must make a decision whether or not to authorize the transplantation. An entire chapter is devoted to posthumous donation - No. 3. Article 14 states that relatives can declare that they disagree with the removal of organs from the deceased. They are given two hours to do this, and with such a statement the body will not be touched.
At the same time, to resolve disputes on this issue, when a person agreed to donation while still alive, and relatives opposed it, a separate article No. 15 was prescribed. It states that if a relative does not agree that the organ be taken away from the deceased, and In this case, the patient himself gave such consent during his lifetime, then the opinion of the relative will not be taken into account. They will take the organ. And vice versa.
The new law specifies in detail the mechanism of child donation. Doctors will have to obtain the consent of one of the parents. Moreover, if the opinions of the father and mother differ, then the transplant will be impossible. It is also prohibited if the possible donor is an orphan. The new law has been discussed for more than five years. But it has not yet been accepted.
— The new law, if adopted, will contain elements of control over all components of transplantation. We are talking about including waiting lists in such a control system and what we constantly talk about is the register of lifetime expressions of will. In fact, we need a failure register,” explains Sergei Gauthier.
No matter how many problems there are in transplantology, doctors in Russia save hundreds of lives. While waiting for the new law, they are trying to convince people that a transplant is the only chance for life for many.
“They often say that it’s terrible, that people hope for the best and expect someone’s death. Of course this is not true. They don't expect any death. They are waiting for the opportunity to be helped. It is impossible to influence the mortality of other people with such expectations. We can all find ourselves in a situation where today we are alive and well, and tomorrow we suddenly need a transplant, God forbid. Therefore, we need to treat each other with respect and try to help each other,” says Alexander Bykov, chief transplantologist of the Novosibirsk region.
Postoperative period
After the operation, the patient is under medical supervision for a long period of time. During this period, immunosuppressive therapy with the help of hormones and cytostatics is selected, thanks to which it is possible to avoid rejection processes, the condition of the postoperative wound is assessed, and complications are corrected if they arise.
In the first month after surgery, a myocardial biopsy is performed every 1.5-2 weeks. This is necessary to assess the condition of the donor heart. Over time, this procedure is performed less and less often.
Three more important texts about organ transplantation
Almost 500 people with organ transplants now live in the Novosibirsk region. We talked to three Siberians and found out how their worldview changes after walking on the very edge, whether it’s hard to take pills by the handful, and what they believe.
In March, the NHS told how, thanks to one donor, four people received a chance at a new life. The child received part of the liver, the man received the heart, and the elderly received the cornea and the ability to see. At the Novosibirsk Regional Hospital, patients got to know each other, thanked the doctors and told their difficult stories.
In early August, Novosibirsk resident Tatyana Mankova went to a party, after which she felt unwell. The last thing she remembers is how she ended up in an infectious diseases hospital. The next memory is how she woke up in the Meshalkin clinic and heard from the doctors that she had received a heart transplant. Tatyana was shocked and couldn’t believe it. Then she found out that she miraculously survived. We talked to her about what it was like to accept a “strange” heart, what difficulties she is currently facing and how her attitude towards life has changed.
conclusions
Transplantation is an operation that allows you to replace a weakened heart that does not perform its functions with an organ from a healthy donor. The intervention requires highly qualified medical personnel, multifaceted and lengthy rehabilitation, and large financial costs. Patients are required to take cytostatic drugs for life, which results in a high risk of postoperative complications. Nevertheless, the transplant made it possible to prolong the lives of people with terminal heart failure and therefore found wide application in modern cardiac surgery, certainly saving humanity.