Forms of pancreatitis
Acute – characterized by acute girdling pain in the upper abdomen. Pain often appears after eating fatty foods or alcohol. Unpleasant sensations can be either barely noticeable or unbearable, radiating to the scapula or sternum. Nausea, vomiting, and stool disturbances are observed. Due to the obstructed flow of bile, the skin takes on a yellowish color.
Chronic - the main localization of pain is on the upper part of the abdominal wall with irradiation to the back, chest (left side), lower abdomen. Unpleasant sensations occur after eating heavy fatty foods, alcoholic drinks, and constant stress.
The development of chronic pancreatitis is characterized by nausea, loss of appetite, bloating, bowel dysfunction, and sometimes vomiting.
The chronic form of the pathology differs from the acute form by periods of remission and exacerbation. As the disease progresses, periods of exacerbation become more frequent; intestinal disorders, disturbances in normal digestion, and weight loss are possible.
Chronic pancreatitis often causes complications (stomach bleeding, cancer, cysts and abscesses, liver damage, diabetes mellitus, enterocolitis). That is why you need to take the disease seriously and, at the slightest suspicion of the development of inflammation, consult a doctor.
What is the mechanism of connection between the pancreas and blood pressure?
At first glance, it may seem that the pancreas and blood pressure cannot be connected in any way, since completely different body systems are responsible for them. But everything in the human body is interconnected, and diseases of the gastrointestinal tract, including the pancreas, are a common cause of hypertension.
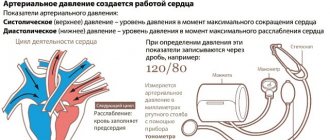
There are several mechanisms by which high blood pressure relates to pancreatitis. Hypertension in acute inflammation of the gland is characteristic of the initial stage. Against the background of a severe pain attack, stress hormones are released and the autonomic nervous system is activated. As a consequence, vasospasm occurs and a violation of adequate blood circulation in all internal organs. It is even possible to develop a hypertensive crisis with all the ensuing complications. In the acute stage, the increase in pressure is not long-term and is replaced by persistent hypotension.
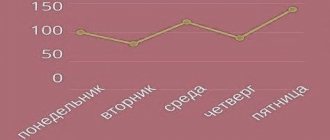
In the chronic course of pancreatitis, the pressure has an abrupt character, but more often patients suffer from hypertension. Since the affected pancreas cannot fully cope with its functions, nutritional deficiency occurs; micro- and macroelements necessary to strengthen the walls of blood vessels, the heart, and nourish the nervous system are not absorbed. With periodic exacerbations, intoxication of the body with decay products increases.
In addition, the inflamed gland swells, squeezing nearby lymph nodes, blood vessels, nerve endings and plexuses. Autonomic innervation is activated and blood pressure increases.
Also in the pancreas are cells that produce insulin, a hormone responsible for the utilization of glucose. If an organ suffers from chronic inflammation, pancreatogenic diabetes mellitus may begin to develop over time. In this disease, insulin production is affected, leading to persistent hyperglycemia (high blood sugar). Due to the pathology, kidney function is impaired (diabetic nephropathy), sodium is not excreted from the body and retains water, which leads to an increase in the volume of circulating blood and an increase in blood pressure.
Reasons for the development of pancreatitis
The disease develops due to damage to pancreatic tissue. This happens for the following reasons:
- alcohol and tobacco abuse
- abdominal trauma, surgery
- uncontrolled and long-term use of medications: antibiotics, hormonal drugs, corticosteroids, some diuretics
- intoxication with food products, chemicals
- genetic predisposition
- improper diet with a predominance of spicy and fatty foods and long breaks between meals
Symptoms of pancreatitis
Manifestations of pathology vary depending on the form - acute or chronic pancreatitis. In acute pancreatitis the following are observed:
- The pain is intense, constant, the nature of the pain is described by patients as cutting, dull.
- High body temperature, high or low blood pressure - the patient’s well-being quickly deteriorates due to the rapid development of the inflammatory process.
- Pale or yellowish complexion.
- Nausea and vomiting - dry mouth and a white coating appear, attacks of vomiting do not bring relief. The most correct step at this moment is to fast; any food intake can only worsen the situation.
- Diarrhea or constipation - stool in acute pancreatitis is most often foamy, often with a foul odor, with particles of undigested food. On the contrary, there are constipation, bloating, and hardening of the abdominal muscles, which may be the very first signal of an acute attack of pancreatitis.
- Bloating – the stomach and intestines do not contract during an attack.
- Shortness of breath - appears due to loss of electrolytes during vomiting.
Chronic pancreatitis is characterized by the following symptoms:
- Abdominal pain - may be girdling or have a clear localization radiating to the back. Appears after eating.
- Intoxication of the body - general weakness, loss of appetite, tachycardia, increased body temperature, and decreased blood pressure appear.
- Endocrine disorders - ketoacidosis, diabetes mellitus, tendency to hypoglycemia. Bright red spots may also appear in the abdomen, back, and chest, which do not disappear with pressure.
With a long course of the disease, the patient gradually develops anemia, weight loss, dry skin, brittle hair and nails, symptoms of vitamin deficiency, and increased fatigue.
What is pancreatic hypertension and why does it occur?
In medicine, pancreatic hypertension is the name given to increased pressure in the main duct of the pancreas (PG) due to obstructed outflow of its juices or additional reflux of bile along the biliary tract.
This condition is a complication of the chronic course of the disease and most often causes severe pain during an attack. But this is what people call a pathology in which blood pressure rises against the background of exacerbation of pancreatitis. A change in blood pressure may well be a sign of inflammation of the pancreas. In the initial stages of the disease, hypertension is sometimes diagnosed, even in the form of crises. Later, when the body is depleted due to enzyme intoxication, persistent hypotension sets in, which is difficult to combat.
It is believed that the cause of hypertension is the development of pain shock, in response to which the body reacts by increasing pressure. Elderly people with problems with the cardiovascular system are especially prone to this variant of the disease.
Symptoms of pathology
The main symptoms of a combination of hypertension and pancreatitis are:
- dizziness attack;
- headache;
- decreased visual acuity, blurred vision;
- numbness of fingers, feeling of “crawling goosebumps”;
- insomnia;
- increased irritability;
- noise or ringing in the ears;
- nosebleeds;
- the appearance of swelling on the face and limbs;
- increased sweating;
- pain in the heart area.
First aid for an attack of pancreatitis
To reduce pain, you can use a heating pad filled with cold water. It needs to be applied to the abdominal area, namely to the epigastric region (the area under the xiphoid process, corresponding to the projection of the stomach onto the anterior abdominal wall). This allows you to reduce the intensity of pain, slightly reduce swelling and inflammation.
The patient must comply with the hospital regime. This will reduce blood flow to the organ, and therefore reduce inflammation.
Eating is prohibited. The digestion process can cause more severe pain, nausea and vomiting. And the diet will reduce the production of enzymes that increase the inflammatory response and pain. You need to fast for 3 days. You can drink clean water without gases.
It is imperative to call a doctor for an examination, even if the patient is not exactly sure that this is an attack of acute pancreatitis. As we already know, this pathology can subside and then rapidly recur. At this time, you can take a painkiller to reduce discomfort.
Diagnosis of the disease at the private medical clinic “Medunion”
Diagnosing this disease is not difficult, since the first signs speak for themselves. However, in order to prescribe adequate treatment, it is necessary to determine the form of the disease. To do this, the doctor performs laparoscopy - a method that allows you to examine the abdominal cavity from the inside using a special instrument.
If acute pancreatitis is suspected, laboratory tests are performed:
- General blood analysis
- Blood chemistry
- Analysis of urine
- Stool analysis
- Ultrasound, MRI or radiography of the abdominal organs
- Computed tomography according to indications
In the chronic form, the same studies are carried out, but it is better to take tests during the period of exacerbation of the disease.
What diseases of the cardiovascular system and gastrointestinal tract mutually aggravate each other?
The combination of non-alcoholic fatty liver disease (fatty hepatosis) with heart and vascular diseases significantly increases the risk of developing cardiovascular accidents. Cardiovascular disease is the leading cause of death in patients with fatty liver disease.
In people with hypertension combined with non-alcoholic fatty liver disease, hypertension is unstable and may develop a form of hypertension that is resistant to treatment.
Erosive and ulcerative lesions of the stomach and duodenum are quite often complicated when taking drugs to prevent the formation of blood clots in the coronary arteries, which contain acetylsalicylic acid. They are prescribed for the treatment of coronary heart disease, angina pectoris, and myocardial infarction.
Pathological changes in the intestinal microflora are currently considered as an independent risk factor not only for intestinal diseases, but also for the development of lipid metabolism disorders, systemic inflammation, obesity and type 2 diabetes mellitus, which increase the risk of developing cardiovascular diseases and their complications.
Treatment of acute pancreatitis
If acute pancreatitis is detected, the patient should be hospitalized immediately. Treatment should take place in a hospital setting, as this condition is very dangerous.
To relieve pain, antispasmodics are taken; in difficult cases, the contents of the stomach are pumped out to relieve the load on the gland.
In case of exacerbation of pancreatitis, patients require hospitalization with daily monitoring of blood parameters, water balance, leukocyte count, and enzyme levels in the blood serum during the first week. In the first 1–3 days, fasting and taking alkaline solutions every 2 hours are recommended.
During an exacerbation of chronic pancreatitis, the patient is shown therapy similar to the acute process. The patient must follow a diet throughout his life and take drugs from the group of antispasmodics and drugs that normalize the secretory function of the organ.
The most important thing in the chronic form of the disease is to maintain a diet that involves excluding fatty and fried foods from the diet. At the slightest violation of the regimen, the patient may experience discomfort and nausea. For intense pain, the doctor prescribes antispasmodics. Antisecretory therapy can be used for a short course.
How to distinguish cardiac pain from non-cardiac pain?
The heart and organs of the digestive system are located quite close to each other, therefore, when pain occurs in the left half of the chest, both a gastroenterologist and a cardiologist are involved in the examination and diagnosis. The complaint of chest pain is one of the most common and alarming symptoms for both the doctor and the patient. Differential diagnosis is most often carried out between gastroesophageal reflux disease (GERD) and angina or coronary heart disease, and in case of an acute painful attack, between exacerbation of GERD and myocardial infarction.
In addition to gastroesophageal reflux disease, chest pain can be caused by
- esophageal spasm;
- reflux esophagitis;
- hiatal hernia (hiatal hernia);
- stomach ulcer;
- biliary or intestinal colic;
- cholecystitis;
- pancreatitis.
In addition, there are cases when a patient has both pathologies: gastrointestinal disease and heart disease. In such cases, it must be taken into account that drugs used to treat coronary heart disease and hypertension have a relaxing effect on the smooth muscles of the esophagus and may lead to aggravation of reflux symptoms.
Diet for pancreatitis
For any form of the disease, the patient is prescribed a strict diet “Table No. 5p”, according to which it is forbidden to eat spicy and fried foods. All dishes are steamed, boiled or baked. Alcohol and smoking are also prohibited.
It is also necessary to limit salt intake and eat small portions 6 times a day. Dishes should always be served warm. It is necessary to exclude all products with a high content of extractives or essential oils (fish, meat broths, cocoa, coffee, etc.), fresh berries, vegetables, herbs, fruits, sour juices, carbonated drinks, marinades.