Hypertensive crisis is a severe form of arterial hypertension. Can occur at any time. More often observed in women than in men. The cause of the occurrence lies in the disruption of blood pressure regulation. If arterial hypertension is common in 40% of the population, then in only 1% of cases there may be a sudden jump from baseline values, which leads to a sharp deterioration in health with a high risk of death.
What exactly are the symptoms of a hypertensive crisis should be known not only to hypertensive patients, but also to their loved ones. Normal and elevated blood pressure values are individual for each person. When a crisis occurs, signs of impaired cerebral or coronary blood supply are observed.
Symptoms and signs of their manifestation
When a hypertensive crisis occurs, the following symptoms appear:
- nausea, vomiting, suffocation;
- convulsions and loss of consciousness;
- intense headache;
- clouding of consciousness and disturbances in speech and vision;
- heart pain and palpitations;
- trembling, sweating, chills;
- feeling of lack of air;
- Possible loose stools.
Are you experiencing symptoms of a hypertensive crisis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
GBUZ NO "Pavlovsk Central District Hospital"
Emergency care for acute life-threatening conditions
In our country, up to 80% of deaths occur outside of medical organizations - at home, at work, in the country, in public and other places. Most of them occur suddenly or by the mechanism of sudden death. Statistics show that many patients (or their relatives) call an emergency doctor late, which reduces the likelihood of rescue.
By mastering the necessary first aid skills in the form of self- or mutual assistance (on the part of people surrounding a person who finds himself in such a critical condition), in most cases the patient’s life can be saved.
Often, up to 30-50%, a life-threatening complication with a dangerous fatal outcome may be the first and last manifestation of these diseases (complications).
FIRST AID for a heart attack
Characteristic signs (symptoms) of a heart attack (myocardial infarction):
• sudden (paroxysmal) pressing, squeezing, burning, aching pain in the chest (behind the sternum) lasting more than 5 minutes;
• similar pains are often observed in the left shoulder (forearm), left shoulder blade, left half of the neck and lower jaw, both shoulders, both arms, the lower part of the sternum along with the upper abdomen;
• lack of air, shortness of breath, severe weakness, cold sweat, nausea often occur together, sometimes follow or precede discomfort/pain in the chest; often these manifestations of the disease develop against the background of physical or psycho-emotional stress, but more often with some interval after them.
Uncharacteristic signs that are often confused with a heart attack:
• stabbing, cutting, pulsating, boring, constant aching pain for many hours and not changing its intensity in the heart area or in a specific clearly defined area of the chest
Algorithm of emergency actions in case of a heart attack (advice to the patient) - a reminder for the patient
If you or someone else suddenly has the above characteristic signs of a heart attack, even with weak or moderate intensity, which last more than 5 minutes, do not hesitate, immediately call an ambulance team. Do not wait more than 10 minutes - in such a situation it is life-threatening.
Remember that being intoxicated in this life-threatening situation is not a reasonable excuse for delaying calling an ambulance. If you have symptoms of a heart attack and there is no way to call an ambulance, then ask someone to take you to the hospital - this is the only right decision. Never drive yourself unless you have no other choice.
In the most optimal scenario, if a heart attack occurs, you must follow the instructions received from your attending physician; if there are no such instructions, then you must act according to the following algorithm:
• Immediately after an attack occurs, sit down (preferably in a chair with armrests) or lie down in bed with the head of the bed raised, take 0.25 g of acetylsalicylic acid (aspirin) (chew the tablet, swallow) and 0.5 mg of nitroglycerin (spray one inhalation dose into the cavity mouth while holding your breath, place one tablet/capsule under the tongue, first bite the capsule, do not swallow); free your neck and provide fresh air (open the vents or windows).
• If after 5-7 min. After taking acetylsalicylic acid (aspirin) and nitroglycerin, pain persists, it is imperative (life-saving) to call an ambulance and take nitroglycerin a second time.
• If pain persists 10 minutes after taking the second dose of nitroglycerin, it is necessary to take nitroglycerin a third time.
• If after the first or subsequent doses of nitroglycerin there is severe weakness, sweating, shortness of breath, you need to lie down, raise your legs (on a bolster, etc.), drink 1 glass of water and then, as with a severe headache, do not take nitroglycerin.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvoastatin), give the patient his usual daily dose and take the drug with you to the hospital.
Attention ! A patient with a heart attack is strictly forbidden to get up, walk, smoke or eat until the doctor’s special permission;
You should not take aspirin (acetylsalicylic acid) if you are intolerant to it (allergic reactions), as well as with obvious or worsening peptic ulcers of the stomach and duodenum;
Nitroglycerin should not be taken if there is severe weakness, sweating, or if there is severe headache, dizziness, or acute impairment of vision, speech, or coordination of movements.
FIRST AID for acute cerebrovascular accident
The main signs (symptoms) of acute cerebrovascular accident:
• numbness, weakness, “disobedience” or paralysis (immobilization) of an arm, leg, half of the body, distortion of the face and/or drooling on one side;
• speech disorders (difficulties in choosing the right words, understanding speech and reading, slurred and unclear speech, up to complete loss of speech);
• disturbances or loss of vision, double vision, difficulty focusing;
• imbalance and coordination of movements (feelings of “swaying, sinking, body rotation, dizziness”, unsteady gait up to falling);
• unusual severe headache (often after stress or physical exertion);
• confusion or loss of consciousness, uncontrollable urination or bowel movements.
If any of these signs suddenly appear, call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
Patient Reminder
1. Call an ambulance immediately, even if these manifestations of the disease were observed for only a few minutes
2. Before the arrival of the emergency medical team:
• If the patient is unconscious, place him on his side, remove removable dentures (food debris, vomit) from the mouth, make sure that the patient is breathing.
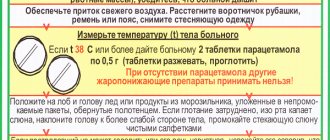
• If the victim is conscious, help him to a comfortable sitting or semi-sitting position in a chair or on a bed, placing pillows under his back. Provide fresh air. Unbutton your shirt collar, belt, waistband, and remove tight clothing.
• Measure your blood pressure if its upper level exceeds 220 mmHg. Art., give the patient a drug that lowers blood pressure, which he took before.
• Measure your body temperature. If the temperature is 38° or more, give the patient 1 g of paracetamol (2 tablets of 0.5 g, chew, swallow), (if paracetamol is not available, do not give other antipyretic drugs!).
• Put ice on your forehead and head, you can take food from the freezer, put in waterproof bags and wrapped in a towel.
• If the patient has previously taken medications that lower cholesterol levels in the blood from the statin group (simvastatin, lovastatin, fluvastatin, pravastatin, atorvastatin, rosuvastatin), give the patient the usual daily dose.
• If the victim has difficulty swallowing and saliva drips from his mouth, tilt his head towards the weaker side of the body and blot the dripping saliva with clean tissues.
• If the victim is unable to speak or has slurred speech, reassure and reassure him that the condition is temporary. Hold his hand on the non-paralyzed side, stop him from trying to talk, and don't ask questions that require an answer. Remember that although the victim cannot speak, he is aware of what is happening and hears everything that is said around him.
FIRST AID for hypertensive crisis
Hypertensive crisis is a condition manifested by high blood pressure (BP) (systolic or “upper” blood pressure, usually more than 180 mm Hg; diastolic or “lower” blood pressure - more than 100 mm Hg) and the following main symptoms:
• headache, often in the occipital region, or heaviness and noise in the head;
• flashing “flies”, a veil or a net before the eyes;
• nausea, feeling of exhaustion, overwork, internal tension;
• shortness of breath, weakness, constant monotonous aching pain/discomfort in the heart area, sometimes the appearance or increase of pastiness/swelling of the skin of the face, arms, legs.
Algorithm for emergency actions in case of hypertensive crisis
(advice to the patient) – a reminder for the patient
If symptoms of a hypertensive crisis appear, you must:
• remove bright light, ensure peace, access to fresh air (unbutton your shirt collar, ventilate the room, etc.);
• measure blood pressure (see the method for measuring blood pressure at the end of this section) and if its “upper” level is higher than or equal to 160 mm Hg, you must take an antihypertensive drug previously recommended by your doctor. In the absence of an antihypertensive drug recommended by a doctor or when a blood pressure level is registered above 200 mm Hg. urgently need to call an ambulance.
• before the arrival of emergency medical services, it is necessary, if possible, to sit in a chair with armrests and take a hot foot bath (put your feet in a container of hot water).
Attention! A patient with a hypertensive crisis is prohibited from any sudden movements (suddenly standing up, sitting down, lying down, bending over), pushing hard or any physical activity.
• 40-60 minutes after taking the medicine recommended by the doctor, it is necessary to re-measure blood pressure and if its level has not decreased by 20-30 mm Hg. from the initial state and/or the condition has not improved - urgently call an ambulance.
• If you feel better and your blood pressure decreases, you need to rest (lie in bed with the head of the bed raised) and then contact your local (family) doctor.
When talking with your doctor, you need to clarify which medications you need to take if a hypertensive crisis develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with your doctor for what manifestations of the disease you need to urgently call an ambulance.
All patients with hypertension need to create an individual mini-first aid kit for a hypertensive crisis and carry it with them at all times, since a hypertensive crisis can develop at any time and anywhere.
FIRST AID for acute heart failure
Acute heart failure (AHF) is a severe pathological condition that develops in patients with various heart diseases and hypertension. This is one of the most common reasons for calling an ambulance and hospitalization of patients, as well as mortality in our country and around the world.
The main manifestations (symptoms) of acute heart failure are:
• heavy, frequent (more than 24 per minute) noisy breathing - shortness of breath, sometimes reaching the level of suffocation, with predominant difficulty in inhaling and a clear increase in shortness of breath and cough in a horizontal position. A sitting position or a lying position with the head of the head raised up alleviates the patient's condition;
• often when breathing, wet, squelching wheezing/sounds, interrupted by coughing, become audible; in the terminal stage, breathing takes on a bubbling character with the appearance of foam at the patient’s mouth;
• characteristic sitting posture of the patient, resting his straight arms on his knees or on the seat (to facilitate breathing)
Acute heart failure can develop very quickly and lead to the death of the patient within 30-60 minutes. In most cases, 6-12 or more hours pass from the first clinical signs to severe manifestations of AHF, but without medical care, the vast majority of patients with AHF die.
Algorithm of emergency actions for acute heart failure
(advice to the patient) – a reminder for the patient
When the above symptoms of AHF appear in patients with hypertension or heart disease (but not the lungs or bronchi), it is necessary:
• call an ambulance
• give the patient a sitting position, preferably in a chair with armrests on which he can lean and engage the intercostal muscles in the act of breathing
• provide physical and psycho-emotional peace and fresh air by ventilating the room
• place your feet in a large container (basin, tank, bucket, etc.) with hot water
• in extremely severe cases, tourniquets are applied to the legs in the groin area, compressing the superficial veins, but not the deep arteries, which reduces blood flow to the heart and thereby facilitates its work
If the patient or the person providing first aid has experience in the use of nitroglycerin, it is prescribed in a dose of 0.4 (0.5) mg (inhalation into the oral cavity is carried out under the root of the tongue, the tablet/capsule is placed under the tongue, the capsule must first be bitten, do not swallow). If the patient’s well-being improves after using nitroglycerin, it is reapplied every 10-15 minutes until the arrival of the emergency medical team. If there is no improvement in the patient’s well-being after the next dose of nitroglycerin, it is no longer used.
Attention! A patient with AHF must exclude all physical activity; it is strictly forbidden to walk, smoke, drink water and take liquid food until special permission from the doctor; Nitroglycerin should not be taken if blood pressure is less than 100 mm Hg. with severe headache, dizziness, acute impairment of vision, speech or coordination of movements.
All patients with hypertension or heart disease with shortness of breath and swelling in the legs should discuss with their doctor what medications should be taken if AHF develops, clearly write down their names, dosage and time sequence (algorithm) for taking them, and also check with the doctor for which manifestations of the disease, it is necessary to urgently call an ambulance.
Each such patient needs to create an individual first aid kit for AHF and constantly have it with him.
FIRST AID for sudden death (advice to eyewitnesses)
Most often, sudden death occurs due to cardiac arrest.
activities.
The main signs (symptoms) of sudden death:
• Sudden loss of consciousness, often accompanied by agonal movements (a standing or sitting person falls, convulsive muscle tension, involuntary urination and defecation are often observed; a lying person sometimes makes a convulsive attempt to sit up or turn on his side)
• Sudden complete cessation of breathing, often after a short period (5-10 seconds) of agonal pseudobreathing: the patient makes wheezing and/or gurgling sounds, sometimes similar to a convulsive attempt to say something.
Algorithm for urgent actions of eyewitnesses to the sudden death of a person
• If a person suddenly loses consciousness, immediately call an ambulance team (if there are other people nearby, they call an ambulance). Next, shake the patient by the shoulder and ask loudly, “What’s wrong with you?” If there is no response, active patting is performed on the patient’s cheeks; if there is no reaction, immediately begin closed cardiac massage.
• The patient is placed on a hard, flat surface (floor, ground, flat hard area and similar places, but not on a sofa, bed, mattress and other soft surfaces), and the front part of the chest is freed from clothing. Determine the location of the hands on the patient’s chest as indicated in the figure. One palm is placed in the place indicated in the figure, and the palm of the second hand is placed on top of the first in exact accordance with the image of the hands in the figure.
Rice. Illustration of the technique of closed cardiac massage
• With straight arms (not bent at the elbows), vigorous rhythmic compression of the victim’s chest is performed to a depth of 5 cm with a frequency of 100 compressions on the chest per minute
• When signs of life appear (any reactions, facial expressions, movements or sounds made by the patient), cardiac massage must be stopped. If these signs of life disappear, heart massage must be resumed. Stops of cardiac massage should be minimal - no more than 5-10 seconds. When signs of life resume, the heart massage stops, and the patient is provided with warmth and peace. If there are no signs of life, cardiac massage continues until the arrival of an emergency medical team.
If the first aid provider has special training and experience in performing cardiopulmonary resuscitation, he can perform artificial ventilation in parallel with closed cardiac massage. In the absence of special training, artificial ventilation of the lungs and determination of the pulse in the carotid artery should not be performed on the patient, since special scientific studies have shown that such procedures in inexperienced hands lead to an unacceptable loss of time and sharply reduce the frequency of revival of patients with sudden cardiac arrest.
remember, that
- emergency medical care only called in the first 10 minutes from the onset of a heart attack or stroke allows full use of modern highly effective methods of inpatient treatment and many times reducing mortality from these diseases
- acetylsalicylic acid (aspirin) and nitroglycerin taken in the first minutes can prevent the development of myocardial infarction and significantly reduce the risk of death from it
- state of alcohol intoxication is not a reasonable basis for delaying calling an ambulance in the event of a heart attack and acute cerebrovascular accident - about 30% of people who suddenly (within an hour from the onset of symptoms) died at home were intoxicated.
- closed cardiac massage performed in the first 60-120 seconds after sudden cardiac arrest allows up to 50% of patients to be brought back to life.
Print Email
Types of pathology
Types of hypertensive crisis are classified depending on the manifestation of symptoms. Medical care is selected individually according to indications and clinical manifestations. Hypertensive crisis types I and II, complicated and uncomplicated forms are types of pathology. Hyperkinetic crisis or type I is characterized by rapid development. Acute headache and dizziness, nausea, and vomiting occur. The state is close to fainting. Blood pressure rises above 200 mm Hg. Art. (systolic - upper), which is why red spots appear in the face, neck, chest, feeling of heat, tachycardia, moist skin.
Hypokinetic crisis or type II occurs when there is a violation of the treatment regimen or rhythm of life in patients with stage III arterial hypertension. Deterioration in well-being develops more slowly, although the intensity remains noticeable. The severity of the headache increases exponentially. Diastolic (lower) pressure remains in the range of 140-160 mmHg. Art. Symptoms include nausea and vomiting, lethargy, blurred vision and hearing, and a tense pulse.
A complicated hypertensive crisis has several vectors of development, which affects the type of complications. There are such subtypes: coronary, asthmatic, cerebral. Against this background, pulmonary edema or cardiac asthma, acute left ventricular failure may develop. Cerebrovascular accidents, ischemic stroke and other pathologies may occur. An uncomplicated hypertensive crisis requires pressure correction in the next 24 hours, but it has an important nuance - there is no risk of target organ damage.
First aid
Understanding what a hypertensive crisis is, you need to know how to properly provide first aid to a person with the development of a severe, life-threatening condition. First of all, if there is a sharp jump in blood pressure, you need to urgently call an ambulance team. But before the arrival of specialists, it is necessary to try to stabilize the patient’s condition in order to minimize the risks of dangerous consequences.
It is necessary to reduce blood pressure using medications. It should be remembered that it is necessary to lower blood pressure gradually when a hypertensive crisis develops. You should also take a sedative (valerian or corvalol) to relieve anxiety.
It is important that the patient is in a sitting position that is as comfortable as possible. It is imperative to ensure the supply of fresh air. A cold compress should be applied to the patient's forehead. Additionally, you can make hot foot baths with a water temperature of 40°C or apply mustard plasters to your calves.
With the development of a complicated hypertensive crisis, treatment is possible only in intensive care conditions. Patients are kept in the intensive care ward until their condition is completely stabilized. After this treatment, a certain period of time continues in the hospital therapeutic department.
Preventive measures
The best prevention of a hypertensive crisis is awareness of the peculiarities of the occurrence of attacks, an understanding of how an increase in blood pressure occurs and the causes of this phenomenon.
Timely diagnosis and interaction with a doctor, following medical recommendations is an opportunity to prevent the development of crises of varying degrees. Hypertension can be controlled if:
- avoid drinking alcohol;
- stop smoking;
- reduce salt intake to 5 g per day;
- normalize body weight;
- adhere to antihypertensive therapy;
- reduce stress levels;
- avoid overwork.
Prevention of hypertensive crisis
This is a dangerous condition that can be fatal. It is important to start treatment in a timely manner, to strive to prevent further progression of the disease that caused a sharp increase in blood pressure, following simple recommendations:
- control blood pressure;
- normalize nutrition (follow a regimen, diet);
- maintain normal weight;
- eliminate heavy physical and emotional stress;
- eliminate harmful addictions;
- be examined by a doctor.
Information about the diagnosis and treatment of patients
Regardless of the causes of a hypertensive crisis in a man or woman, diagnosis comes first to determine the further course of treatment. Symptoms may coincide with other pathological conditions. Diagnosis of hypertensive crisis includes the following procedures and studies:
- Analysis of urine;
- ECG, CT, radiography;
- heart rate measurement.
The doctor needs to collect a detailed history of the patient's condition. When the attacks began, the frequency of their occurrence, symptoms, whether the patient receives regular antihypertensive therapy, what methods were used to reduce blood pressure, whether there was experience in independently stopping the crisis, the presence of concomitant diseases - basic information for the doctor during the diagnosis.
Rehabilitation
Rehabilitation includes not only drug therapy and dietary nutrition, but also a number of other mandatory rules that can be followed subsequently to avoid relapse:
- It is impossible to recover from a hypertensive crisis without giving up bad habits. You will have to forget about coffee, cigarettes, and alcoholic drinks for a long time, or better yet, forget about them forever.
- Stressful situations should be kept to a minimum. Nervous stress, depression, conflicts - all this negatively affects the health of every hypertensive patient.
- After a crisis, it is important to maintain a work-rest schedule, not to overdo it at work, to rest on time, to wake up and go to sleep at the same time.
- Do you trust traditional medicine? Some recipes can help improve your condition during recovery from a crisis. But before taking medicinal decoctions and tinctures, you must consult a doctor, since not all herbs are compatible with medications.
- Moderate physical activity will help improve blood circulation impaired by an attack or prolonged course of hypertension. The intensity and type of exercises are selected together with the doctor, taking into account the current condition of the patient.
For one person, the optimal solution would be short walks in the park, for another - yoga or swimming.
Even if the condition has completely stabilized, you cannot independently refuse to take the hypertensive medications recommended by your doctor. This can lead to a relapse of the hypertensive crisis with renewed vigor.
Treatment and its features
Treatment for a hypertensive crisis is prescribed depending on the medical history and the presence of other conditions in acute form or chronic pathologies (cardiac percussion, auscultation of the heart, lungs, large vessels, hemorrhagic stroke, renal failure, severe myocardial ischemia). At the time of the attack, the patient needs medical attention. It consists of lowering blood pressure.
Afterwards, drug therapy is prescribed. When prescribing drugs, it is important that they act after a maximum of 20-30 minutes, and the effect lasts for at least 4-6 hours. When treating crises, the danger is the occurrence of uncontrollable hypotension. For this reason, self-medication with such a diagnosis carries the risk of drug collapse. Special medical supervision is necessary for patients with a history of concomitant diseases. It is important to understand that with proper treatment of arterial hypertension, crises occur extremely rarely.
Recovery and relapse prevention
Patients who have experienced a hypertensive crisis need time to recover. How long this period lasts depends on the type of attack, the presence of concomitant disorders, and the stage of hypertension. Rehabilitation includes compliance with a number of rules and recommendations:
- The patient is strictly prohibited from smoking and alcohol. These bad habits impair blood circulation, which aggravates the condition of the cardiovascular system and provokes new attacks.
- Salt, which contributes to fluid retention in the body, is excluded or minimized from the diet.
- You should not drink drinks containing caffeine, or eat hot, spicy foods that increase blood pressure.
- You should avoid physical activity. In this case, bed rest is necessary only in the acute period. Patients after a hypertensive crisis benefit from leisurely walks and special exercises approved by the attending physician.
- It is important to stop being nervous about it and without it. It is stress and depression that last a long time that often become provocateurs for an attack. If you cannot limit yourself from unpleasant situations, you should take sedatives.
- It is impossible to prevent the next attack without treating hypertension. You should listen to your doctor’s recommendations and start taking medications that stabilize blood pressure for a long period. Long-acting tablets will not be able to cope with the crisis, but they are indispensable for normalizing blood pressure.
Healthy eating is an essential part of recovery after a crisis
The recovery period continues until the patient’s condition is completely stabilized. But a hypertensive person should not relax, immediately going to the nearest store for cigarettes and leaning on homemade pickles. A person who is faced with a crisis and knows the dangers of such an attack must make every effort to protect himself from a repetition of the situation.
Answers to frequently asked questions from patients
How long does a hypertensive crisis last?
On average, an attack lasts about 2-3 hours. Symptoms develop either quickly or progressively, depending on the form of the crisis.
What should not be done during a hypertensive crisis?
You cannot endure and wait for the crisis to pass. It is necessary to carry out first aid measures that involve a gradual decrease in blood pressure. During an attack, the patient should not stand, stand up sharply, bend over, push, or take physical action. When blood pressure decreases, the patient can rest in a horizontal position, but with the head of the bed raised.
What is the hidden danger of a hypertensive crisis?
The consequences of a hypertensive crisis are widespread - stroke, myocardial infarction, disorders of the central nervous system, angina pectoris, and aneurysm. For this reason, hypertension should be monitored by a doctor, and the patient should take antihypertensive drugs regularly.
Reasons for development
Hypertensive crisis most often occurs with hypertension. It often develops against the background of other pathologies, in particular, patients who are diagnosed with:
- Kidney diseases: pyelonephritis, polycystic kidney disease, diabetic nephropathy, etc.
- Diseases of the endocrine system: pheochromocytoma, Itsenko-Cushing's disease, thyrotoxicosis, etc.
- Atherosclerotic lesion of the aorta and narrowing of its lumen.
The risk group includes people with hereditary complications and women during menopause. The development of a hypertensive crisis can be triggered by smoking, alcohol abuse, unbalanced diet, obesity, lack of physical activity, stress, and sudden refusal of antihypertensive drugs.
Diet
Diet 10th table
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of products: 1700-1850 rubles. in Week
Diet for hypertension
- Efficacy: therapeutic effect after 21 days
- Timing: constantly
- Cost of products: 1600-1700 rubles. in Week
Proper nutrition for hypertension, along with drug treatment, can serve as a preventive measure for the development of crises. Patients are advised to eat a nutritious diet with limited salt, refractory fats and foods rich in cholesterol .
- Salt can be consumed no more than 5 g per day.
- Alcohol, strong tea and coffee, which stimulate the central nervous system, are limited/excluded.
- Otherwise, pickles, spicy snacks, fatty foods, fatty meats, and rich broths are strictly limited.
- If you are overweight, limit flour products, sugar, cereal products, honey, grapes, raisins, and jam.
- Low fat dairy products.
- Whole grain products.
- Lean meat and poultry (boiled or baked).
- Vegetable side dishes, vegetable salads, vinaigrettes, seaweed.
Great importance is attached to the content of potassium and magnesium in products. Consumption of potassium and magnesium has a beneficial effect on the course of hypertension, the condition of blood vessels and the heart. Potassium is rich in baked potatoes, bananas, currants, tomatoes, pumpkin, carrots, cabbage, zucchini, cucumbers, beets, melons, beans, oranges, figs, raisins, dried apricots, and nuts. Magnesium is found in seaweed, rice, buckwheat, bran, bananas, rolled oats and nuts. The diet must contain foods containing polyunsaturated fatty acids: fatty sea fish, fish oil, seeds, nuts and vegetable oils (linseed/rapeseed/olive).