Acrocyanosis is not a separate disease, but a pathological condition that accompanies the disease. When it occurs, the blood supply to small capillaries is disrupted and it becomes insufficient.
The skin acquires a bluish tint, which appears in places farthest from the heart. These are entire limbs or just the tips of the toes and hands, the upper parts or all of the ears, lips, and nose.
Such body problems occur against the background of chronic and acute diseases. This is one of the symptoms of a serious illness, which helps to identify it in time.
This condition was described at the end of the 19th century and described a form of disturbance of the tone of small vessels. Despite its long history, doctors have a lot of questions related to this phenomenon, the answers to which remain to be found.
It is now known about acrocyanosis that such a disorder is not always a sign of pathology. Bluish skin can be observed in premature babies and the phenomenon increases with stress, screaming, and hypothermia.
There are several forms of acrocyanosis. Highlight:
- Primary. It is not considered a consequence of any disease and occurs as a result of external factors (cold, stress).
- Secondary. This is a pathological type, which is a symptom of diseases - the cardiovascular system, nervous system or oncology.
In ICD-10, the condition is coded R23 – “Other skin changes” and I73 – “Other peripheral vascular diseases”.
Depending on what led to the disruption of the blood supply to the capillaries, there are:
- Idiopathic. This is acrocyanosis in women, which manifests itself during puberty and persists at rest, at normal ambient temperatures, intensifying with physical activity or hypothermia. With this type, the lips, hands, and nose have a bluish tint as a result of narrowing of small arteries during spasm.
- Spasmodic. It is observed in healthy adolescents of both sexes with a thin, asthenic body type. The skin turns blue under the influence of any external irritants.
- Anesthetic acrocyanosis is what is called cold blueness. It is common to all people and manifests itself when the surface temperature of the skin drops to 15 degrees.
- Diffuse. It develops when there is a lack of oxygen in the arterial blood due to impaired saturation in the lungs.
Information about primary acrocyanosis
Primary acrocyanosis, not related to diseases of the body, occurs in 34% of cases. Women notice causeless skin changes 8 times more often than men.
The primary type includes acrocyanosis in newborns; what it is, neonatological medical data will help explain: at birth, the child learns to breathe independently, adapts to the external, new environment. Oxygen first reaches vital organs, and only then to the skin. Blueness may appear when the newborn is restless and crying.
This condition is considered normal if no congenital life-threatening diseases are detected. The bluish tint to the extremities in infants goes away as the respiratory system adapts.
The primary type of appearance of cyanosis is also due to hormonal changes. Teenagers may have a persistent pale blue color to their fingertips for several months. Pregnant women may also notice this sign. According to medical data, the primary type of cyanosis is more common in women after 30 years of age. Their acrocyanosis goes away only during menopause.
General information
The term “acrocyanosis” was first used in 1896 by J. B. Crocq, who described a primary disorder of peripheral vascular tone and named one of its forms.
This disorder is not an independent disease, since it always occurs as a result of some disturbance in the body.
Acrocyanosis in newborns is not always a sign of the presence of pathology - it is often detected in the area of the feet, hands and nasolabial triangle in children born prematurely. Signs of acrocyanosis in infants become more pronounced with hypothermia, crying and severe anxiety.
Secondary acrocyanosis is no joke
The secondary type is more serious. The blue tint of the skin of the extremities indicates pathologies of the body, that is, it is a symptom of the following diseases:
- development of connective tissue at sites of trauma to internal and external organs;
- neurological problems;
- mental disorders;
- benign and malignant tumors;
- endocrine system disorders (diabetes mellitus, hypothyroidism);
- anorexia;
- hematopoietic disorders.
Diseases of the respiratory system are one of the likely causes of the development of cyanosis. Acrocyanosis most often occurs in bronchial asthma. Often, in patients with chronic pathologies of the lungs, bronchi and other respiratory organs, there is a pronounced blue tint to the fingertips, sometimes spreading to the entire hand or foot.
Acrocyanosis in chronic heart failure and valve defects occurs in 98% of cases. The “motor” cannot cope with filling the vessels with the required amount of blood.
A blue tint to the skin may appear due to digestive disorders or intoxication of the body. Sometimes cyanosis is a side reaction to taking medications: antidepressants, vasopressors (drugs to normalize blood pressure).
A blue tint to the tips of the toes and hands is a symptom of HIV, hepatitis C, and psittacosis. The causes of secondary acrocyanosis are also hereditary pathologies: Morphan's disease, Down syndrome, Sneddon syndrome.
Types of deviations
Four types of acrocyanosis can be observed:
- Central (permanent). This type is most often diagnosed in children with intracranial trauma received during childbirth. It can also manifest itself against the background of immature centers; most often, such diagnoses are made to premature or immature children. In adults, central acrocyanosis appears when respiratory depression occurs or when muscle layers are involved in the pathological process. Manifested by attacks of apnea, shallow breathing and convulsions.
With this disease, breathing may stop at night.
- Respiratory. With this type of acrocyanosis, the skin is affected mainly around the lips. A pronounced blue discoloration can be noticed when you are anxious. Most often occurs with disorders such as pneumonia, atelectasis, aspiration, developmental defects and others. Symptoms of respiratory cyanosis include shortness of breath, various respiratory syndromes, and skin changes.
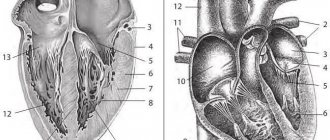
- Cardiovascular cyanosis appears with an increase in blood pressure in the pulmonary circle, but congestion is noted in the large circle. If a child is diagnosed with total cyanosis, then most likely the baby has congenital heart defects. This type is permanent, and its symptoms can intensify with tension.
- With swelling of the legs. Most often, this type of cyanosis can be seen in children born in the breech position, or in adults who have any damage to the spinal cord. As you might guess from the name, this type of cyanosis has its own specific symptom - swelling of the legs.
To read: Why does the lower blood pressure increase?
Heart failure can cause leg swelling
Symptoms of the disease
We looked at what acrocyanosis is from the point of view of the mechanism of its occurrence. How does it manifest itself:
- Blue discoloration of the tip of the nose, the upper parts of the auricles of the lips.
- Blue discoloration of the feet or hands when lowered, especially when it is cool.
- Minor swelling in the area of blueness (legs and arms).
- Cold, dry, non-elastic skin in the area of blueness.
- Increased blueness with cold, stress, physical activity and its weakening under the influence of heat.
- Weakening of the shade when raising the arms and legs upward.
In pathological forms the following is observed:
- Excessive sweating of the extremities, which is characteristic of heart disease.
- Painful sensations that occur with Raynaud's disease.
- A bluish color with a purplish-red tint is characteristic of heart diseases, with a gray tint - for pathologies of the lungs and respiratory system.
Causes
Physiological causes of acrocyanosis:
- Slowing down the linear speed of blood flow.
- Increased utilization of oxygen by tissues in the periphery.
Capillary blood contains a lot of reduced hemoglobin.
This may occur for reasons:
- Pathological formation of conglomerates (glued together) of red blood cells under the influence of cold or due to disease.
- Raynaud's disease.
- Complicated course of radiculitis of the cervical spine.
- Phlebeurysm.
- Autoimmune inflammation of small arteries and veins (Buerger's disease).
- Scleroderma.
- Sudek's syndrome (trophic and vasomotor disorders after limb injuries).
- Cervical rib syndrome.
- Exposure to medications or other toxic substances resulting in the formation of forms of hemoglobin that are not capable of carrying oxygen (sulf- and methemoglobin).
- Insufficient blood oxidation in the lungs.
- Mixing of a large amount of venous blood to arterial blood.
- Slowing down the blood and increasing the utilization of oxygen from it.
The severity of acrocyanosis and its occurrence are influenced by:
- The amount of skin color pigment. The more it is, the less pronounced the cyanosis.
- Amounts of oxyhemoglobin in the blood.
- Skin thickness.
- The number of small capillaries in an area of skin, their location and size. The more of them, the stronger the cyanosis.
- Increased venous pressure.
- Ambient temperature.
Forms
Based on the cause of acrocyanosis, there are several types:
- Anesthetic, which occurs as a reaction when cold is applied to the surface of the skin. Slightly expressed cyanosis is a physiological phenomenon that develops when the skin temperature drops to 15 - 20 ° C.
- Essential or idiopathic. This form of acrocyanosis, caused by spasm of small arteries, is manifested by a persistent bluish tint of the lips, hands and other acral parts of the face in physically healthy females during puberty. It is observed even in warm conditions and at rest, intensifying during physical activity or under the influence of cold.
- Central or diffuse, which is caused by a sharp decrease in oxygen levels in the pulmonary circulation. Occurs with a marked increase in the content of reduced hemoglobin in venous blood (5.2 g%) as a result of impaired blood oxygenation in the lungs.
- Spasmodic, which develops as a result of spasm of small vessels in response to any irritants. It is detected in adolescence in persons with astheno-neurotic syndrome.
What diseases does it develop in?
Secondary acrocyanosis develops in diseases:
- Cardiovascular diseases (myocardial infarction, vascular atherosclerosis, stroke).
- Hypoxia.
- Diseases of the respiratory system (acrocyanosis in bronchial asthma, alveolar malformations, pulmonary embolism, pulmonary hypertension).
- Some cancers.
- Prolonged fasting, sudden weight loss with constant nervous tension.
- Diseases of the joints and connective tissue (arthritis, lupus erythematosus, granulomatosis).
- Blood diseases.
- Spinal cord injuries.
- Chronic hypertrophic rhinitis.
- Down, Riley-Day, Sneddon syndromes, which are hereditary.
- Infectious diseases (mononucleosis, HIV, hepatitis C).
Why does the skin turn blue?
Doctors distinguish several types of blue discoloration of the skin, each of which has its own causes and mechanisms of development. Acrocyanosis occurs due to impaired blood circulation in the smallest capillaries and manifests itself in areas of the body farthest from the heart. This is its main difference from “ordinary” cyanosis, in which the blueness of the skin is general.
The bluish coloration of the skin during acrocyanosis is caused by an increased content of carboxyhemoglobin in the blood, which accumulates due to a slowdown in blood flow in the peripheral vessels.
At normal blood circulation rates, hemoglobin and carbon monoxide compounds are “evacuated” from the capillaries in time, while the skin remains healthy pink.
Acrocyanosis develops when the outflow of blood is impaired for some reason, and reduced hemoglobin accumulates in the smallest vessels, causing the skin to darken and acquire a bluish tint.
Diagnostics
Diagnosing the condition is not difficult. A visual examination is sufficient, which shows bluish extremities (feet and hands) and areas of the face. The doctor pays attention to which areas are widespread, whether there is pain in the area of bluish skin and sweating in places. This is necessary in order to determine whether acrocyanosis is primary or secondary, as well as to diagnose the disease in a timely manner.
First of all, acrocyanosis is differentiated from a disorder associated with Raynaud's syndrome. With the latter, the skin changes shade: when cold it turns blue, when warmed it restores color. This does not happen with secondary acrocyanosis.
Diffuse acrocyanosis requires further examination and study; it occurs with severe disturbances in the functioning of the cardiovascular system and lungs. With other diseases, the limbs turn blue asymmetrically, accompanied by soreness and partial tissue necrosis.
The patient may be prescribed:
- Dopplerography is a study of blood flow in the peripheral circulatory system.
- Plethysmography is the study of blood flow in tissues.
- Electrothermometry.
- Capillaroscopy is the study of the structure of capillaries on the surface of the skin and mucous membranes.
- Ultrasound of the heart.
- X-ray examination of the lungs.
- Spirometry.
- ECG.
- Blood tests.
The examination begins with an examination of the patient and a questioning. It is important for the doctor to find out when the first signs of the problem appeared and what factors contributed. General blood and urine tests are performed. Research will help identify an infectious disease or pathology.
Acrocyanosis should be differentiated from a number of other pathologies. Diagnostic studies are aimed not only at identifying the extent of the lesion, but also to exclude the following diseases and abnormal conditions:
- Ultrasound of the heart, respiratory organs, limbs.
- X-ray of the chest and limbs.
- Electrothermometry on different parts of the body (temperature measurement).
- Doppler sonography, which will help identify circulatory problems.
Capillaroscopy allows you to find out the condition and structural features of the capillaries of the lips, tongue, and nail bed. The study is necessary to identify anomalies in areas where a blue tint is noticed.
Features of acrocyanosis in newborns
It is a very common disease in children. When cyanosis is diagnosed in a newborn, you first need to find out its nature. Cyanosis in newborns can be of several types:
- Peripheral. It happens to absolutely all children, even healthy ones. It usually appears in the first days. The child still has an embryonic type of blood circulation and is still adapting, which is why for several days some areas of the child’s body take on a bluish color. Acrocyanosis appears mainly on the feet, hands, and around the mouth. The affected area increases with stress, crying, screaming, hypothermia, and even with ordinary anxiety. Most often, peripheral cyanosis occurs in premature infants. When the child adapts to the world around him, the disease recedes and then disappears altogether.
Peripheral acrocyanosis manifests itself as blue discoloration on the arms or legs
- Central cyanosis is observed in exactly the same cases as in adults, with insufficient oxygen concentration in the blood. It may occur in the case of pathologies in the child’s cardiovascular system.
To read: Signs of unstable angina and classification of the disease
Character
In order to clarify the nature of the pathology, find out:
- Time of appearance. The occurrence of deviations from the first days of life is observed in children with developmental defects that make it possible to change the direction of blood flow.
- The circumstances under which it was diagnosed.
- Persistent cyanosis.
- Changes in shades depending on time.
- Place of origin.
The manifestation of this symptom can also be observed in newborns.
In newborns, cyanosis can be: permanent, transient, total, regional and isolated. Constant cyanosis is observed at any time of the day. Transient, in turn, indicates hypoglycemia, diabetic fetopathy, sepsis, meningitis. Total cyanosis covers almost the entire surface of the child’s body. Regional cyanosis, in which only certain areas on the surface of the newborn’s body are affected. Such areas can be: the nose, the area around the mouth, hands and feet, ears.
To cure a disease, you need to know about its characteristics and how it occurs.
Treatment
We found out about acrocyanosis that it is a condition, but not a disease, we cannot talk about a specific treatment. If it is physiological in nature and does not cause inconvenience, then it is not worth treating. To reduce the appearance of cyanosis, it is enough to warm the skin and calm down.
Secondary cyanosis as such does not require treatment. It is necessary to deal with the disease of which it is a symptom. If acrocyanosis leads to a cosmetic defect, then the following may be recommended:
- Creams and ointments with glucocorticosteroids.
- Electrophoresis with nicotinic acid.
- Taking adenoblockers.
- Injections or droppers with prostaglandin.
- Preparations with minoxidil.
- UV irradiation of the skin.
- Immunosuppressive therapy for autoimmune diseases (rheumatoid arthritis, etc.).
- Neuromuscular stimulation after injury.
In exceptional cases, surgical intervention is indicated - removal of the nerve nodes that innervate the vessels of the area affected by acrocyanosis.
If acrocyanosis leads to partial tissue necrosis with the appearance of ulcers, it is necessary to ensure that they do not become infected (treatment with ointments and solutions, sterile dressing).
Medicines aimed at improving blood circulation will help relieve symptoms. Vinpocetine, Vazonit are prescribed orally, intramuscularly or intravenously. Sometimes warming ointments (Viprosal) are used.
If the reason lies in vascular spasm, it is advisable to take antispasmodics: No-shpa, Papaverine. Preparations based on potassium and calcium will help strengthen the walls of blood vessels. Increase the level of immunity - vitamins, especially A, E, C.
Physiotherapy procedures: applications, magnetic therapy, UHF, electrophoresis have shown effectiveness in getting rid of the causes of cyanosis of the extremities.