Immediately after birth, the newborn stays for some time with his mother under the supervision of doctors, so that they can identify possible pathologies of the child in the early stages. This approach influences the successful prevention of complications and timely treatment of cerebral palsy and other neurological diseases. One of them may be cyanosis - blueness of the skin or mucous membranes, which indicates pathological processes occurring inside the newborn. Lack of timely help if a blue complexion or lips occurs can be fatal.
Causes of cyanosis in newborns?
Typically, blueness on the face of a newborn appears in the nasolabial triangle, which indicates heart problems. This phenomenon can be congenital, with blood supply being obstructed.
The causes of cyanosis depend on the location of its appearance:
- On the face - indicates a lack of oxygen in the tissues or impaired blood supply to the brain. All this can lead to suffocation and result in serious heart disease.
- Under the eyes - speaks of physical exhaustion and the need for normal nutrition.
- On the mucous membranes - it usually appears immediately after birth, which indicates problems with the respiratory system, or more precisely, a lack of oxygen in the lungs. Blueness in a baby increases when crying or during feeding, but it does not become pathological.
The doctor considers any case of blue skin individually, because it can be caused by several factors. In most of them, it is necessary to provide qualified assistance. The cyanotic color of the mucous membranes or skin indicates a high level of carbon dioxide in the blood.
If cyanosis develops quickly: from a few minutes to a day, then this is most likely associated with bronchial asthma, lung damage or heart disease.
Cyanosis and “blue” defects
What is "cyanosis"? Why does it occur? What to do with him?
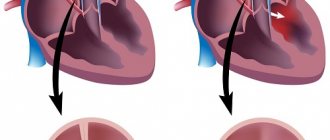
In previous chapters, we described “pale” defects, in which arterial blood, through a defect located inside or outside the heart, enters the venous system and mixes there with venous blood. A “left-to-right” reset is formed, i.e. from the left chambers of the heart to the right.
With the defects of the group that we now want to examine, the opposite picture occurs: venous blood enters
the arterial system
and mixes with
oxidized arterial blood
. That is, there is a “right-to-left” discharge, from the right parts of the heart to the left.
Children suffering from these types of defects differ from healthy ones in the bluishness of the skin and, especially, mucous membranes, which look crimson-red or purple, as if the child had eaten blueberries. Noticeable blue discoloration may appear immediately after birth, or may appear several weeks or even months later, and can be of varying degrees. Why is this happening?
The fact is that arterial blood receives, through a defect in the heart, an admixture of purely venous, oxygen-poor blood. As a result, this blood is constantly undersaturated, and there is not enough oxygen for the tissues.
The body fights this in a simple way: the bone marrow and spleen produce more blood cells - red blood cells, which carry this oxygen. Their amount in the blood is significantly higher than normal. of hemoglobin increases
, which they contain, is actually the substance to which oxygen molecules are attached in the pulmonary alveoli.
The greater the admixture of venous blood to arterial blood, the more red blood cells and hemoglobin there are in the blood. This is a protective reaction that allows cells of organs and tissues to live, despite the low oxygen content in the incoming blood.
But such a disturbed composition also affects the appearance of the skin and mucous membranes, since their vessels are filled with thick and dark blood: after all, an increase in the number of red blood cells makes the blood thicker, and the blood flow in the capillaries slows down.
The consequences of this condition are dangerous. In children, small blood vessels can become clogged, especially in the brain. As a result, areas of insufficient supply to certain areas of the brain may develop and neurological symptoms may appear. Due to insufficient oxygen supply to the areas of the body furthest from the heart—the tips of the fingers and toes—they not only begin to change their color, becoming bluish, but also thicken at the ends (the so-called “drumsticks”), and the nails become enlarged and become convex (the so-called “watch glasses”).
In patients with defects in which the “right-to-left” discharge is accompanied and enhanced by an obstruction to blood flow in the right ventricle, dyspnea-cyanostic attacks appear when the child loses consciousness for several seconds, and sometimes minutes, and cannot inhale a sufficient amount of air. This is already very scary, because it can turn into a long-term and sometimes irreversible loss of consciousness. So the very existence of cyanosis is dangerous at any age and it is absolutely necessary to get rid of it surgically.
Depending on the degree of mixing of venous and arterial blood, the degree of cyanosis can be very different. Sometimes the child’s entire body is “blue”, sometimes only the lips and tips of the fingers and toes. With some defects, cyanosis does not become noticeable immediately, but several weeks or months after birth. In other words, a defect that was “pale” in infancy becomes “blue.” This does not mean that something happened to the child. It’s just that with growth, the “right-to-left” discharge has become larger. And please keep in mind: while a “pale” vice can become “blue” over time, then a “blue” can only
using surgery.
How to get treatment at the Scientific Center named after.
A.N. Bakuleva? Online consultations
Diagnosis of the disease in a newborn
At the neurorehabilitation center, diagnostic measures are used that are aimed at identifying the cause of the disease - its main cause of occurrence.
First of all, a small patient is listened to to identify heart sounds and breathing stability.
More detailed information is obtained using special instruments and laboratory tests:
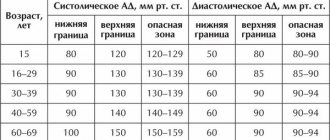
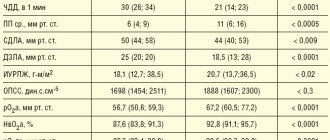
- checking vital parameters such as temperature, breathing, pulse and blood pressure;
- objective examination with medical history;
- X-ray of the chest or respiratory organs;
- blood analysis;
- response to oxygen therapy.
The specialist also takes into account the presence of provoking factors in the patient’s body and the time of manifestation of cyanosis (in infants the disease is noticeable immediately).
Tactics for cyanosis
Cyanosis often indicates the presence of conditions requiring emergency medical attention: heart failure, suffocation, or terminal illness. But if the causes of cyanosis are, for example, varicose veins or neurocirculatory dystonia, then the patient will be prescribed therapeutic treatment.
Only a specialist can determine the exact cause of the appearance of cyanosis in the skin of the face and other parts of the body, so such a sign should be a reason to visit a therapist, who will conduct the necessary examinations and refer you for consultation to other specialists. In the treatment of diseases in which cyanosis occurs, medications such as:
- bronchodilators;
- analeptics that affect the brain centers that control the respiratory system;
- cardiac glycosides;
- antihypoxants.
More information about cyanosis of the skin and mucous membranes can be found on the pages of our website Dobrobut.com. It is also possible to make an appointment with experienced doctors, whose consultation will help determine the causes of this phenomenon and provide competent, effective treatment.
Related services: Ambulance call 5288
Therapy
During neurorehabilitation
Doctors are trying to normalize hemoglobin and increase oxygen levels; after using oxygen therapy, cyanosis should completely disappear in infants. If cyanosis becomes chronic, then it will not be possible to quickly eliminate the blue color of the skin; it may reappear even after complete disappearance.
During the treatment of facial cyanosis in a newborn, medications belonging to the following groups are often used:
- cardiac glycosides;
- bronchodilators;
- antihypoxants;
- analeptics.
Only a specialist can determine the reasons for the appearance of a bluish color on the skin of newborns, and he will also prescribe the most effective treatment in a particular case. Most often, the disease is stopped in the early stages, but if a child was born with a heart defect, cyanosis can only be removed surgically.
Transient cyanosis
Some people report that from time to time they experience cyanosis in the tips of the fingers of the upper and/or lower extremities. Moreover, no other signs of deterioration in health are noted. This condition cannot be ignored, since in any case it indicates problems in the functioning of the heart or blood vessels. For example, such cyanosis may indicate the progression of neurocirculatory dystonia, and in the absence of medical assistance, sudden changes in blood pressure, constant dizziness, and weakness throughout the body may develop.
Blueness of the skin that occurs during physical activity may indicate the development of inflammatory heart diseases. As a rule, it is accompanied by shortness of breath, fatigue, and tremors of the upper extremities.
If even short-term cyanosis occurs, you should seek help from a medical facility - this will help avoid the most severe consequences.
Acquired heart defects
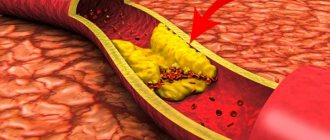
A number of diseases cause secondary structural changes in the heart valves. These are vices. What kind of diseases are these:
- systemic pathologies affecting connective tissue - systemic lupus erythematosus, rheumatoid arthritis;
- infective endocarditis;
- atherosclerosis;
- myocardial infarction;
- traumatic heart injuries (including those received during surgery);
- carcinoid syndrome, etc.
Valves are “doors” for the passage of blood from vessels to the heart, from the heart to vessels and between the parts of the heart (atrium and ventricle). Their defects are of two types:
- “under-opening” of doors - stenosis, as a result of which blood cannot freely pass into the corresponding space;
- constantly “open doors” - valve insufficiency, as a result of which blood can pass not only in the forward direction, but also in the opposite direction.
METHODOLOGY FOR STUDYING PATHOLOGICAL SKIN COLORING
Recognition of cyanosis comes down to differential analysis and verification of the provocateur (the disease against which cyanosis occurred, requiring treatment). At the first level, cyanotic pigmentation is distinguished from related pathologies - methemoglobinemia and carboxyhemoglobinemia.
To do this, blood is taken (it may contain toxins that cause one of three pathologies). For verification and “targeted” treatment, the following can be carried out:
- capillaroscopy;
- UAC;
- spectrophotometry;
- study of blood gases (arterial);
- pulse oximetry;
- measurements of PaO2 and SaO2;
- refined assay for the identification of hemoglobin derivatives.
To exclude (confirm for the purpose of treatment) OD pathologies, X-rays, chest CT and spirometry are performed. To exclude (or clarify and begin treatment) heart disease, you need an ECG / EchoCG, sometimes an MRI or scintigraphy.
Congenital heart defects
An organic defect of various localization either forces the blood to move in a direction not prescribed by law (against its natural flow), or an obstacle appears in its path, which the heart has to overcome with effort. In both cases, an additional load is created both on the heart itself and on the lungs and nearby vessels, which disrupts their functioning and sooner or later ends in irreversible organic changes.
In terms of frequency of occurrence in the top three:
- pathology (defect) of the interventricular septum;
- pathology (defect) of the interatrial septum;
- narrowing (stenosis) of the pulmonary artery.
Less common: patent ductus arteriosus, stenosis of the aortic mouth, tetralogy and pentade of Fallot, others. It is possible to have a combination of different types of defects in one person.
There are some childhood defects that can go away on their own with age. Of course, this only applies to small defects. So, for example, a ventricular septal defect can close in childhood and not cause any concern in the future.
Some congenital heart defects (for example, atrial septal defect) clinically manifest themselves only in adulthood (after 20 years), and before that they are indirectly reflected in people’s susceptibility to infectious diseases of the respiratory system.
HOW TO GET RID OF CYANOSIS?
The treatment tactics for cyanosis always come down to three levels of exposure.
- Urgent identification of the provocateur and treatment of critical illness.
- Oxygen treatment (cocktails, tents, procedures).
- Maintenance treatment. This includes exercises, aqua physiotherapy, massage.
Actually, the treatment of cyanosis is based on the elimination of hypoxia - oxygen deficiency in the blood transport system. Treatment should be carried out with mandatory procedural oxygen support and LOP. The patient himself must comply with a number of conditions for treatment of both the related and the underlying disease.
The first is giving up dangerous habits (alcohol, smoking) - treatment of cardiac and respiratory mechanisms without this is ineffective. The second is building a rest schedule (here – treatment through auto-training and self-massage). Third, a strict treatment regimen for the underlying disease (antibacterial, anti-inflammatory therapy).