First symptoms
A pulmonary infarction does not manifest itself immediately. For the first two to three days after a vessel is blocked, a person may not be aware of the problems. Many people confuse the first symptoms with the discomfort that occurs with angina pectoris. Sometimes pain is possible, as with an acute abdomen. You should be alert to the following symptoms:
- acute chest pain;
- increased pain when coughing, rapid breathing, bending the body;
- shortness of breath that occurs out of the blue, without physical activity;
- when coughing, blood is coughed up (not in everyone, in about half of the cases), complete pulmonary hemorrhage rarely occurs;
- the nasolabial triangle and fingers of the limbs become bluish;
- cold sticky sweat during painful attacks;
- hiccups;
- general malaise, possible fever;
- Some patients vomit.
People suffering from thrombophlebitis and thrombosis, pulmonary hypertension, and frequent relapses of pulmonary embolism are predisposed to pulmonary infarction. Risk factors include age over 60 years, excess weight, pregnancy and childbirth (or caesarean section).
Why is a pulmonary infarction dangerous?
When a large artery is blocked, the patient's condition quickly deteriorates. Pain and fever intensify, panic attacks appear, and attacks of suffocation occur. If a person is not taken to the hospital, he will face serious consequences, including death.
If there is a problem with a small or medium vessel, the pathological condition develops more slowly, and at first the symptoms are not pronounced. But if treatment is left untreated, complications arise:
- post-infarction pneumonia is associated with congestion in those parts of the lung where the blood supply has been disrupted;
- lung abscess - an advanced stage of the infectious process, purulent melting of tissue, subsequently - the formation of a cavity in the lung;
- necrosis of affected tissues due to developing ischemia and cessation of nutrition of a part of the organ.
About the danger of heart attack and the effectiveness of coronary stenting
What do we know about heart attack? Almost everyone has heard that this is a serious, deadly condition. In the relatively recent past, saving the life of a person with a massive heart attack was considered a truly remarkable result of treatment, and with the most favorable course of the disease it meant long months of strict regime, slow recovery, and loss of ability to work. Today, medicine poses different tasks: not just to save, but to return a person to normal life, and the provision of specialized medical care plays an important role here. At the same time, maintaining heart health depends on ourselves.
KONSTANTIN ALEKSENDROVICH KIREEV, head of the Center for X-ray endovascular diagnostics and treatment about the danger of heart attack and the effectiveness of coronary stenting:
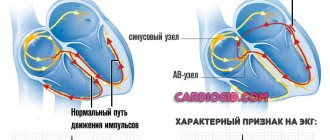
— First of all, it is necessary to understand what acute myocardial infarction is. This is necrosis, that is, the death of a section of the heart muscle, developing as a result of a sudden, acute disturbance of blood flow in the coronary (related to the heart) artery system. Blockage of a branch of the coronary artery can be caused by its thrombosis, less often by embolism or long-term (more than half an hour) persistent spasm.
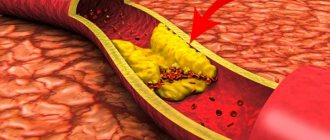
The most common cause of a heart attack is atherosclerosis, when atherosclerotic plaques form on the walls of blood vessels: they narrow the lumen of the coronary arteries and can also contribute to the destruction of their walls, which provokes the formation of blood clots and blockage.
An acute heart attack causes irreversible changes in the heart muscle: the death of part of the functional muscle cells of the heart (necrosis) and their subsequent replacement with connective tissue, that is, the formation of a post-infarction scar. The scar on the myocardium remains for life. It cannot resolve, and the heart always remembers the heart attack. Subsequently, a violation of the blood supply to the myocardium can lead to a disorder of cardiac activity: heart failure develops, that is, the heart does not perform its functions in full, accordingly, for the full existence of the whole organism there is simply not enough “power”.
In simple terms, due to an acute circulatory disorder, the heart gradually begins to “die”, and in order to save a person’s life, it is necessary to restore blood circulation as soon as possible. If medical care is not provided in a timely manner, a person with a heart attack may die within the first 24 hours. In general, the prognosis of the outcome of a heart attack depends on the size of the myocardial lesion, the severity of the course, the age of the patient, and the development of complications. But in any case, the prognosis of the disease is influenced by the timeliness of the start of treatment and its adequacy.
More than 5,000 myocardial infarctions are registered annually in the Chelyabinsk region, and this disease still remains one of the main causes of premature death. For a long time, the treatment of acute infarction in our area was far from the most advanced strategy. According to indications, thrombolytic therapy was carried out, that is, the administration of drugs that resolve the blood clot and restore the patency of the vessel. Such assistance was provided both by emergency medical teams before hospitalization and in intensive care units of hospitals. The success of treatment often depended on the correct choice of drug and the timely start of its use. Of course, there was no talk of the high effectiveness of drug therapy: a very high percentage of deaths (about 16−20%), and if a person remained alive, he became disabled, his heart could not work properly.
The situation changed fundamentally in 2011, when, as part of the healthcare modernization program in Chelyabinsk, they began to perform emergency operations for acute myocardial infarction - percutaneous coronary interventions, including stenting of the coronary arteries. This was an undeniable breakthrough for Chelyabinsk healthcare.
Coronary stenting is the most effective way to treat acute myocardial infarction due to the complete elimination of circulatory disorders through direct and immediate impact on the infarction. The essence of the method is to install a special stent into the affected vessel through the radial artery (on the wrist) in order to restore blood flow. A stent is a metal mesh structure that resembles a hollow tube of small diameter. Using a special balloon, a folded stent is inserted into the artery, under the control of an X-ray machine, it is delivered to the site of narrowing of the vessel, then, when the balloon is inflated under pressure, it is expanded and implanted, expanding and supporting the affected vessel in the area of blockage or critical narrowing and restoring blood flow. Also, in order to make the intervention most effective and safe, a wide range of special drugs are used.
The advantages of stenting also lie in the fact that this operation is low-traumatic, practically painless, has a small number of complications, reduces the length of hospital stay from 15-17 to 7-11 days, makes it possible for the patient to become active early and refer him for rehabilitation to a sanatorium. resort conditions. Thanks to stenting in acute myocardial infarction, mortality has decreased by almost half, and today it is about 6%. But the most important thing is that after a heart attack the patient can return to a normal, fulfilling life, to his work.
COMMENT BY EVGENY MIKHAILOV, chief freelance cardiologist of the South Ural Health Directorate, candidate of medical sciences:
— During a heart attack, approximately half the thickness of the heart muscle dies in the first three hours, and in the next three hours the entire thickness of the muscle dies. Therefore, stenting in the acute period of myocardial infarction is effective if it is performed as early as possible, no later than the first 6 hours from the onset of the infarction, optimally - up to 2-3 hours. Restoring blood flow in a clogged artery in this time period, before the development of irreversible changes in the myocardium, sharply reduces the area of the infarction, and sometimes makes it possible to “interrupt” its development. When we intervene after these 6 hours, we can only reduce the area of necrosis, but not save from myocardial infarction. Because patients arrive too late, half of them do not survive.
Here, a lot depends on how quickly the patient or his relatives call an ambulance. People should know the clinical manifestations of myocardial infarction. If you suddenly experience severe, usually frightening, pain in the chest that cannot be relieved by taking nitroglycerin, you should not hesitate, call an ambulance immediately. Thus, first aid will be provided on the spot: the team carries out intensive therapy to relieve pain and dissolve the blood clot, and will deliver you to the hospital as quickly as possible. But I repeat once again, the most important thing is to call an ambulance on time!
About the work of the X-ray surgical service
Four days a week we receive patients from 4 districts of Chelyabinsk and 7 municipalities of the Chelyabinsk region, a population of 700 thousand people. Today, percutaneous coronary interventions are one of the priority areas of work for the Road Clinical Hospital. It should be noted that we provide emergency assistance to everyone without exception, and not just assigned citizens. Among the hospitals of the Russian Railways-Medicine health care network from Kaliningrad to Khabarovsk, we have the largest volume of emergency coronary stenting operations.
We are interested in ensuring that a patient who came to us sick leaves us relatively healthy, relatively quickly, so that he can return to work with minimal loss of quality of life. Every effort is being made to achieve this. All actions of medical personnel are very clearly organized to quickly determine treatment tactics - from the emergency department to the patient’s admission to the cath lab or intensive care unit. We not only strive to provide this assistance as quickly as possible, but we also have every opportunity to do so.
Effective results are also facilitated by the fact that practical work is always carried out in close connection with science. On the basis of the road hospital there are two main departments of the South Ural State Medical University, which means the introduction of modern technologies into the treatment process, continuous training of specialists, provision of advisory assistance, joint analysis of the treatment and clinical cases.
We should always evaluate our work in accordance with global standards so that we can understand whether we are doing good or bad work. Thus, it is considered that a medical organization is working well when 70% of patients with heart attacks undergo coronary stenting. In 2021, this figure was 76%. In my opinion, today everything that is necessary is being done to save lives and preserve people’s health.
How not to “live to have a heart attack”
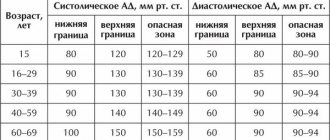
There are major risk factors that can lead to the development of myocardial infarction. We can influence some of them, but not others. You cannot influence, for example, gender (men are more susceptible to coronary heart disease), age, family history, or hereditary predisposition. However, we can significantly reduce the adverse effects of factors such as arterial hypertension, smoking, diabetes, high cholesterol, excess weight, and a sedentary lifestyle. All these factors, both in combination and each independently, provoke the development of atherosclerosis, which, as I have already said, is the main cause of myocardial infarction.
We conducted a study of medical and social status, quality of life, and the presence of risk factors for atherosclerosis in a group of patients diagnosed with myocardial infarction. 200 people took part in the survey, all residents of Chelyabinsk, under the age of 65 (this age group is at risk of premature death, a generation that in 10 years will give the expected average life expectancy in the country).
The results of the study revealed that the lifestyle of our patients leaves much to be desired. Every second patient smokes, 90% have a smoking history of more than 20 years, 2/3 of patients smoke a pack of cigarettes or more per day. Arterial hypertension was detected in 70% of patients, while only 20% of them take antihypertensive drugs; diabetes mellitus - in 40%, high cholesterol - in 42%, obesity - in 55%, that is, in every second person studied.
Moreover, every third out of 200 patients suffers from a second heart attack, because people neglect secondary prevention, in particular, drug therapy and giving up bad habits. Many patients, feeling almost healthy after stenting, want to forget about the disease as soon as possible. However, we must not forget about it. In order for the heart to work efficiently, for a year you need to take special medications to thin the blood, improve cardiac output, contribute to minimal changes in the myocardium after a heart attack, and statins to lower cholesterol levels. It is also necessary to give up smoking, alcohol, monitor your weight, adhere to a certain diet, etc. The result of non-compliance with these recommendations is always disastrous.
I note that the number of patients in whom a heart attack is not associated with atherosclerosis, but is most likely caused by a sharp spasm of the coronary artery against the background of severe stress or a large loss of fluid and, as a consequence, thickening of the blood and the formation of a blood clot, in the study group is very, very small .
Indeed, people think little about their health, they ignore alarming symptoms due to an irresponsible attitude towards themselves or out of ignorance, although there is enough necessary information in the media and on the Internet, there are very good social advertising videos. But citizens simply do not pay attention to this.
Today, medical capabilities make it possible to save the lives of patients even with severe heart attacks. But not only doctors, but also ordinary people should be wary in this regard. Without this, no technology will help. Atherosclerosis is a very vicious disease; it affects many vessels, not only those related to the heart, but also in the brain and limbs. Therefore, proper attention to your health is so important.
Give up bad habits and “fast food”, add more physical activity to your life, devote at least 30 minutes a day to physical exercise and walking in the fresh air. Also, do not skip medical examinations and consult a doctor on time.
Even if you undergo a medical examination once every three years, this will allow you to identify existing health problems and correct them before the bell rings.
Now there are very good and affordable medications that can not only improve the situation, but actually affect the prognosis for a person’s life. A heart attack can be prevented, and not at the cost of any incredible efforts or means. You just need to be a little more attentive to yourself. Share
How to diagnose
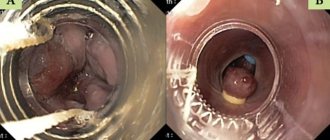
If a pulmonary infarction is suspected, the patient is examined by a pulmonologist and a cardiologist. At the first stage, the doctor interviews the patient and listens to him using a phonendoscope. Small wheezing, pleural flapping noise, systolic murmurs and other specific signs should alert you. The patient experiences rapid breathing, and palpation of the abdominal area reveals an enlarged and painful liver.
An important test is an x-ray of the lungs. Photographs are taken in frontal and lateral projections, effusion in the pleural cavity, deformation and expansion of the lung root are detected. The state of pulmonary circulation is assessed using angiopulmonography - x-ray with contrast injected into the arteries.
To complete the clinical picture, it is necessary to take a general blood test and undergo an ECG. The patient may also be sent for Doppler ultrasound of the lower extremities to assess the condition of the veins and the presence of thrombosis.
Noninvasive ventilation for acute myocardial infarction
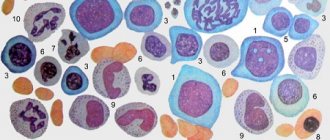
Acute heart failure (AHF) during myocardial infarction (MI) is the inability of the heart, as a pump, to pump the required volume of blood (cardiac minute volume (MCV) l/min), adequate to the metabolic needs of the body (providing basal metabolism), which is manifested by severe hemodynamic disorders and impaired gas exchange function of the lung. Failure of the pumping ability of the heart, due to ischemic damage to the left ventricular myocardium, leads to the development of hypoxemia - an early and permanent sign of circulatory failure, which underlies the clinical signs of AHF. The basis of the hypoxemic syndrome, by the mechanism of reducing blood oxygen saturation, involves two components of hypoxemia - central (cardiogenic - stagnation of blood in the lung) and peripheral (circulatory - slowdown of peripheral tissue blood flow).
Depending on the severity of clinical manifestations, according to the proposed classification by T. Killip, J. Kimball, there are 4 degrees of AHF in MI:
I degree - absence of clinical manifestations of heart failure;
II degree - wheezing in the lungs during auscultation, heard in an area of less than 50% of the pulmonary fields, or the presence of tachycardia in combination with III sound during auscultation of the heart - systolic ri;
III degree - wheezing in the lungs on auscultation of more than 50% of the lung fields in combination with rhinitis;
IV degree - pulmonary edema, clinical picture of cardiogenic shock [1].
Standard drug therapy (SMT) for acute myocardial infarction (AMI) complicated by AHF is quite well developed and regulated. The in-hospital mortality rate of MI complicated by AHF is 24%; in severe cases, with the need for artificial pulmonary ventilation (ALV) using tracheal intubation, according to domestic and foreign authors, it reaches 52% [2, 3, 4, 6, 7, 8, 9, 12].
Recent fundamental works, including a meta-analysis of a large number of studies of AHF, have shown the high effectiveness of the main methods of non-invasive (mask) artificial pulmonary ventilation (NIV) in the treatment of cardiogenic pulmonary edema (CPE), refractory to CMT: continuous positive airway pressure (CPAP - Continuous). Positive Airway Pressure), support with increased pressure during inspiration (PSV - Pressure Support Ventilation), support with increased pressure at the end of expiration (PEEP - Positive End-Expiratory Pressure) [13, 15, 19].
The British Thoracic Society guidelines recommend the use of CPAP in patients with persistent hypoxemia during complex medical treatment of AHF and reserving the use of two-level ventilation - PSV + PEEP for patients in whom CPAP does not improve [5].
Currently, the medical literature contains isolated reports on the use of NIV in the treatment of COL in patients with AMI [16, 17, 18]. These publications documented that the combination of inspiratory support with positive end-expiratory airway pressure (PSV + PEEP) was more effective in reducing work of breathing and respiratory distress than CPAP alone [10, 11, 14].
All of the above was the purpose of this work - to study the effectiveness of various methods of NIV in patients with AMI complicated by grade III-IV AHF, refractory to standard drug therapy.
Materials and methods. The study group included 94 patients with AMI, whose average age was 67.4 ± 5.5 years. Inclusion criteria were: large-focal AMI complicated by grade III–IV AHF according to the Killip–Kimball classification, respiratory failure and peripheral hypoxemia (resting respiratory rate (RR) > 25/min, H2O2 — transcutaneous < 90%), persisting for 1 hours against the background of ongoing SMT.
SMT included: oxygen through nasal cannulas or face mask, antiplatelet agents and anticoagulants, loop diuretics, nitroglycerin, ACE inhibitors, beta blockers; Patients with grade IV AHF were additionally prescribed catecholamines.
In order to objectify the effectiveness of the treatment, all patients underwent sounding of the right parts of the heart with measurement of mean pressure in the right atrium (RA), systolic and diastolic pressure in the right ventricle (SDP, DPPV), systolic and diastolic pressure in the pulmonary artery (SDPA, DPPA) , pulmonary artery wedge pressure (PAWP), with calculation of cardiac (CI) and shock indices (SI), left and right ventricular shock index (LVSI, IURP), total peripheral vascular resistance (TPVR), total pulmonary resistance (TPR). Before and after 60 minutes of NIV, blood samples were taken from the pulmonary and peripheral arteries to determine the acid-base state of the blood (ABC), hemoglobin concentration (Hb), oxygen and carbon dioxide tension (pO2, pCO2), oxygen saturation of Hb (HbO2) and calculation of the oxygen delivery index (IDO2), oxygen consumption index (IPO2), percentage of blood shunting in the lungs (Qs/Qt). NIV was performed on an RV-7200 device (USA) with atmospheric air (FiO2 - 21%) in three modes: CPAP, PSV and PSV + PEEP. In 85% of cases a face mask was used, and in 15% a nasal mask was used.
Depending on the NIV regimen, patients with AMI complicated by AHF were divided into three groups: group A-1 mask CPAP - 19 patients (11 men, 8 women), average age in the group - 59.7 ± 10.8 years; group A-2 with PSV ventilation mode - 27 patients (24 men and 3 women), average age was 68.3 ± 10.9 years; group A-3 combined ventilation mode PSV + PEEP - 48 patients (34 men and 14 women), average age in the group - 60.7 ± 12.5 years. By age, patients in groups A-1, A-2 and A-3 were comparable and did not differ statistically from each other (p > 0.05).
In group A-1, the course of AMI was complicated by grade III AHF in 15 patients, grade IV AHF in 4. In group A-2, grade III AHF was recorded in 22 patients, grade IV HF in 5. In group A-3, grade III AHF was observed in 38 patients, stage IV HF in 10. With PSV artificial ventilation mode, the inspiratory pressure averaged 17.0 ± 5.9 cmH2O; with PEEP, expiratory pressure averaged 5.4 ± 1.4 cmH2O; average inspiratory pressure PSV + PEEP - 17.6 cmH2O.
The doses and rate of administration of SMT drugs in all patients before and during NIV were almost the same (p > 0.05). When comparing the initial parameters of hemodynamics and gas exchange between groups A-1, A-2 and A-3, no significant differences were noted (p > 0.05).
Statistical processing was carried out using the statistical analysis application package Statistica v.6.0; parametric and nonparametric reliability criteria were used.
Treatment results and their discussion. The dynamics of central hemodynamics and blood gas composition in AMI patients with AHF under the influence of various modes of auxiliary ventilation during spontaneous breathing (groups A-1, A-II, A-III) are presented in
,
,
.
Respiratory support in the CPAP mode from 5.0 to 13 cm H2O led to clinical improvement in 93% of patients, which was expressed in a decrease in patient agitation, a decrease in tachycardia and shortness of breath, and an improvement in peripheral circulation (a positive change in the color, temperature and humidity of the skin) , at the same time, moist congestive rales in the lungs significantly decreased or completely disappeared. Positive clinical dynamics were accompanied by a statistically significant decrease in preload (PPWP mmHg) by 25% and afterload (TPPL) by 13.5% for the left ventricle against the background of a decrease in heart rate (HR) by 10.3% and an increase in pumping function left ventricle (LVRI) by 8.3%, a decrease in the right ventricular performance index by 13.3%.
A decrease in PAWP indirectly indicated unloading of the pulmonary circulation, which led to significant positive changes in gas exchange indicators: an increase in arterial blood oxygenation (HbO2a, %) by 5.6% and mixed venous blood (HbO2a, %) by 11.2% with a statistically significant decrease shunting blood in the lungs by 43%. A decrease in the percentage of blood shunting in the lungs, with an improvement in arterial blood oxygenation, was accompanied by a significant increase in oxygen delivery to the executive organs and tissues: IDO2 increased by 6% (p < 0.0005) with a significant decrease in IPO2 by 12.2% (p < 0. 01), which is associated with a decrease in the work of the respiratory muscles against the background of a decrease in respiratory rate by 23.1%.
Thus, total respiratory support in the form of CPAP with an average pressure of 9.0 ± 0.3 cm water column led to a significant decrease in respiratory rate, heart rate, hydrostatic pulmonary capillary pressure, blood shunting in the lungs, afterload for the left ventricle and was accompanied by an increase in oxygenation of the arterial and venous blood, shock index and oxygen delivery to executive organs and tissues.
Respiratory support with PSV also resulted in rapid clinical improvement and patient stabilization in 91% of cases. Hemodynamic and gas exchange data are presented in.
Inspiratory pressure support led to a significant decrease in hydrostatic pressure in the pulmonary capillary (PCP), systolic pressure in the pulmonary artery and right ventricle by 19.2%, 20% and 25%, respectively, which was accompanied by a decrease in the work of the right ventricle by 16.2% and restoration of the efficiency of the left ventricle of the heart by 17.5%. In total, these changes contributed to a significant decrease in heart rate by 7.4%.
Respiratory pressure support during inspiration in patients of group A-2 led to an effective improvement in gas exchange rates: a decrease in blood shunting in the lungs by 35.1%, restoration of the oxygenating function of the lung - an increase in the oxygen content in arterial blood by 4.5%, an increase in oxygen delivery by 12.9% and a decrease in the O2 consumption index by 7.2%. A statistically significant decrease in heart rate by 13.3% indirectly indicates an improvement in the gas exchange function of the lung, confirmed by a decrease in PCO2 in arterial blood by 5.6%. In turn, a decrease in respiratory rate helps to reduce energy consumption for the work of the respiratory muscles, leading to a decrease in IPO2.
Respiratory support in the PSV + PEEP mode in patients of group A-3 also led to rapid clinical improvement and stabilization of the condition in 92% of observation cases. Positive clinical dynamics were confirmed by objective data presented in.
The table shows that NIV in the PSV + PEEP mode was accompanied by a significant decrease in heart rate by 14.2%, a decrease in hydrostatic pulmonary capillary pressure by 26%, with an increase in left ventricular performance by 14.4%, and an increase in pressure in the right atrium by 83 .3%. The increase in pressure in the right atrium (an indicator of central venous pressure) is due to an increase in intrathoracic pressure due to increased pressure during inhalation and exhalation of the NIV respiratory cycle (on average by 17.6 cm H2O), which is accompanied by an increase in resistance to blood flow to the right ventricle. Indicators of blood pressure, resistance of the systemic and pulmonary circulation, pressure and work of the right ventricle did not change significantly.
It follows from the table that NIV in the PSV + PEEP mode led to a rapid decrease in shortness of breath (RR decreased by 30%), an improvement in the oxygenation of arterial and mixed venous blood by 6% and 9.8%, respectively, and a decrease in the degree of shunting of venous blood in the lungs by 31.8% and an increase in oxygen delivery to executive organs and tissues by 4%. Improvement in gas exchange function of the lung is documented by a decrease in pCO2 in arterial blood by 7.8%.
In a retrospective analysis (for one year) of medical records of patients with AMI complicated by AHF, who underwent standard artificial ventilation using tracheal intubation, hospital mortality was 39.6%. In our studies, in the overall group of patients with AMI complicated by AHF who received NIV in various modes, hospital mortality was 25.5% (24 patients).
Conclusion
With myocardial infarction, there is a violation of the contractile state of the heart muscle, leading to a decrease in the pumping activity of the heart and, as a consequence, to an increase in end-diastolic pressure, in particular in the cavity of the left ventricle. A physiologically significant increase in left ventricular end-diastolic pressure or left atrial pressure invariably leads to a retrograde increase in pressure in the pulmonary vessels and forms post-capillary, passive pulmonary hypertension. In accordance with the Starling equation, with an increase in hydrostatic pressure in the pulmonary circulation, the rate of fluid filtration through the microvascular endothelium in the pulmonary interstitium increases. When fluid is filtered faster than it is removed by the lymphatic system, perivascular, interstitial, and then alveolar pulmonary edema develops.
At the first stage of compensation, with an increase in interstitial pressure, J-receptors are stimulated with an increase in the volume of ventilation, which helps to increase lymph outflow and, as a result, minimizes the risk of progressive interstitial edema and subsequent alveolar flooding.
From a mechanical point of view, fluid retention in the pulmonary circulation can be represented as restrictive disorders, manifested by changes in lung volumes, a decrease in the elastic properties of lung tissue due to edema of the interstitium, flooding of the alveoli - functional units, which overall leads to a decrease in the gas exchange function of the lung.
The hemodynamic factor - an increase in pressure in the venous bed of the pulmonary circulation during AMI - is accompanied by heterogeneous disorders of lung ventilation, which are restrictive (decreased elasticity of the lung tissue) and obstructive (increased airway resistance due to swelling and bronchospasm) in nature.
A progressive decrease in lung capacity and its distensibility lead to an increase in negative pressure in the pleural cavity necessary for inhalation; consequently, to an increase in the “work of breathing”, increasing the proportion of the cardiac output required to provide energy for the mechanics of breathing.
All of the above changes lead to disturbances in the ventilation-perfusion ratios underlying cardiogenic-respiratory hypoxemia, which are aggravated by the appearance of additional intrapulmonary blood flow shunts, reaching more than 10% of the MVR in volume.
In patients with AMI complicated by acute left ventricular failure, the “work of breathing” is increased due to decreased compliance of the lung tissue and increased airway resistance (interstitial and bronchial edema); energy costs for the work of breathing in conditions of reduced CI reach 30% of cardiac output. Consequently, by reducing the energy costs of breathing using NIV, it is possible to reduce the proportion of SI directed to the respiratory muscles, redistributing it to other parts of the cardiovascular system.
NIV during spontaneous breathing of a patient with high blood pressure in various modes (CPAP, PSV PEEP), in addition to reducing the work of breathing, helps to “squeeze” the liquid part of the blood from the alveoli and interstitium of the lung tissue into the bloodstream, which ensures more efficient gas exchange and neutralizes the negative effect of the shunt in the lung.
Thus, respiratory support in various modes - CPAP, PSV and PSV + PEEP - turned out to be an effective method of treating COL, refractory to standard drug therapy, in patients with AMI. Against the background of NIV, clinical improvement and positive changes in parameters not only of hemodynamics, but also of gas exchange were observed. The effectiveness of various NIV techniques and the nature of their impact on indicators such as respiratory rate, heart rate, PP, MPAP, PAWP, IDO2, pO2a, pO2la and Qs/Qt turned out to be similar. A difference was noted when using PSV and PSV + PEEP in the degree of influence on the growth of LVRI and a decrease in CO2 tension in arterial blood.
It can be assumed that respiratory support regimens using PSV and PSV + PEEP will be more effective in patients with AMI complicated by AHF with concomitant hypoventilation and hypercapnia.
Although both PSV and CPAP demonstrate similar efficacy, from a practical point of view, CPAP is cheaper and more accessible in clinical practice, so CPAP may be considered the preferred method in patients suffering from AMI with cardiogenic pulmonary edema.
For questions regarding literature, please contact the editor.
A. M. Shilov , Doctor of Medical Sciences, Professor S. P. Grachev , Candidate of Medical Sciences, Associate Professor of MMA named after. I. M. Sechenova , Moscow
Treatment and prevention
To eliminate pain, the patient is prescribed non-narcotic (less often narcotic) analgesics. Coagulants are used to prevent further thrombosis. And to stimulate the dissolution of already formed blood clots - streptokinase and urokinase, tissue plasminogen activator.
If there is a suspicion of post-infarction pneumonia, antibiotics are prescribed. The drugs are prescribed orally and in the form of droppers. In cases where conservative treatment does not give the expected effect, surgical intervention is indicated - pulmonary embolectomy.
To avoid problems in the future, it is recommended not to start and treat thrombophlebitis in a timely manner. Since pulmonary infarction in the vast majority of cases develops precisely against their background. Therefore, for prevention it is necessary:
- wear compression stockings;
- do therapeutic exercises;
- Visit a phlebologist regularly if you are prone to varicose veins and thrombosis.
If you experience symptoms of a pulmonary infarction, consult your doctor immediately. At the medical center you will receive a consultation with a pulmonologist. If necessary, you will be examined by a surgeon and a cardiologist. At the clinic you will also be tested and undergo the necessary examinations. If therapy is started in a timely manner, the prognosis is favorable.