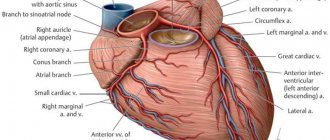
Hydropericardium refers to the accumulation of transudate (non-inflammatory fluid) in the pericardial cavity. Normally, between the layers of the pericardium there is a small amount of lubricant (about 30 ml), which is necessary for the normal functioning of the heart. An increase in the volume of transudate is usually due to increased permeability of the vessels of the pericardial sac in the decompensated course of chronic diseases, or difficulty in its reabsorption, which is caused by venous stagnation.
- Causes
- Symptoms and possible complications
- Diagnostics
- Treatment, prognosis and prevention
Why does pericarditis occur?
The following are the main causes of pericarditis:
- Infectious agents: viruses, bacteria, fungi and even parasites. The inflammatory process in the pericardium is triggered by the influence of exo- and endotoxins released by microorganisms.
- Autoimmune connective tissue diseases such as lupus erythematosus or scleroderma. At the same time, the body synthesizes antibodies to its own cells, which damage connective tissue and cause systemic inflammation.
- Heart diseases. The result of serious damage to the heart muscle is the spread of the pathological process to the surrounding pericardium. This can occur with transmural myocardial infarction, infectious or reactive myocarditis.
- Damage to other organs, such as the kidneys, can lead to pericarditis. In cases of serious impairment of excretory function and the formation of renal failure, deposition of metabolic products in the serous cavities, including the pleura and pericardium, is observed.
- Penetrating pericardial injuries that disrupt the integrity of the pericardial layers.
- Metastatic tumors that cause pericardial carcinomatosis.
- The causes of pericarditis are varied, and, therefore, treatment approaches depend on what caused the inflammation. But in the absence of timely diagnosis and correction of this condition, the outcome is always the same. The result of chronic pericarditis is cardiac tamponade, which leads to the death of the patient.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Classification
The classification is based on the main aspect - the amount and type of accumulated fluid.
Taking into account the amount of fluid in the heart sac and the distance between its leaves, they speak of three stages of the disease:
- Early stage. The amount of accumulated liquid does not exceed 100 ml, the distance between the sheets is from 6 to 10 mm;
- Moderate stage. The accumulated liquid is in the range of 100 - 500 ml, the sheets have separated by 10-20 mm;
- Expressed stage. Water mass > 500 ml, sheets separated by more than 20 mm.
As you can see, an increase in the amount of accumulated fluid increases not only the manifestation of symptoms, but the risk to health and life.
The quality of the accumulated liquid is also important. There can be several types, it is important to know this to make a diagnosis:
- Accumulated natural fluid is a diagnosis of “hydropericardium”;
- Accumulation of fluid with blood - “hemopericardium”;
- Accumulation of lymphatic fluid - “chelopericardium”;
- Accumulated pus and inflammation are called “pericarditis.”
What are the types of pericarditis?
According to the pathophysiological mechanism, pericarditis is divided into:
- exudative pericarditis (when inflammatory fluid accumulates in the cavity - exudate);
- adhesive pericarditis (when “dry” inflammation predominates and adhesions form);
- constrictive pericarditis (when compression of the heart occurs and calcification of the pericardial walls).
This division is very arbitrary, because at different stages of the pathological process the type of inflammation can transform. And the formation of areas of calcification is the outcome of any pericarditis in the absence of adequate therapy.
Treatment methods in Medscan
Patient management tactics at the Medscan clinic are based on international protocols. An individual treatment regimen is drawn up for each patient. Treatment of hydropericardium depends on the amount of accumulated fluid, as well as echocardioscopy (ultrasound of the heart).
Based on the results of laboratory and instrumental studies, the doctor makes appropriate prescriptions.
First of all, specialists pay attention to the underlying pathology (oncological process), which provoked the complication. In parallel with cancer treatment, hydropericardium is combated. It begins with the use of diuretics (diuretics), which “unload” the blood circulation and remove excess fluid.
A significant amount of effusion is observed when a combination of transudate and exudate (produced during inflammation) requires a therapeutic puncture of the pericardium.
Symptoms of pericarditis
The onset of pericarditis, symptoms and first signs are quite characteristic. The main reason to see a doctor is chest pain. The pain syndrome in this disease can be quite pronounced and persistent. But there are times when fever comes first in severity. Its combination with shortness of breath and chest pain is often mistaken for pneumonia.
The pain syndrome in this cardiac pathology can radiate, as with angina pectoris, to the left arm and shoulder blade. But the hallmark of pain with pericarditis is the lack of connection with physical activity. The pain is almost constant and intensifies when changing body position or taking a deep breath.
In addition to pain, pericarditis is always accompanied by additional symptoms: general weakness, increased body temperature, shortness of breath with little physical exertion, interruptions in heart function, and decreased blood pressure. Unlike angina, nitrate-based medications do not provide relief.
If you notice similar symptoms in yourself or your loved ones, you need to urgently consult a doctor, because the price of delay can be human life. Only a professional cardiologist, having examined the patient and prescribed an immediate instrumental examination, will be able to accurately diagnose and recommend adequate treatment.
Otherwise, if medications are not prescribed in a timely manner, a terrible complication inevitably arises - cardiac tamponade. With tamponade, a large amount of exudate accumulates in the pericardial cavity. The consequence is that the heart muscle is literally compressed and cannot fully contract.
The result of such compression is acute cardiovascular failure, cardiac arrest and death of the patient. In this case, the usual methods of resuscitation rarely have a positive effect, and only the release of the pericardium from the excess amount of exudative fluid can make the heart beat again.
Diagnostics
The examination of the patient begins with a history and examination. During percussion, an increase in the size of the heart is determined.
As part of instrumental research, the following is used:
- Chest X-ray - reveals only a significant increase in fluid volume.
- X-ray kymography is a method of recording the pulsation of parts of the heart, as well as the great vessels. With hydropericardium, X-ray film reveals a uniform decrease in ventricular and atrial waves, and with large effusions, their complete disappearance.
- Echocardiography, which is the main method for identifying this pathology. Normally, the distance between the heart wall and the inner surface of the pericardium is 3-5 mm. An increase in the lumen according to ultrasound results to 10 mm or more proves the presence of significant effusion in the cavity.
- Diagnostic puncture of the pericardium is the only method that allows one to establish the exact nature of the pathological contents of the cavity of the heart sac. With hydropericardium, the fluid is transparent, yellowish, poor in protein, and may contain traces of fibrin, a small number of lymphocytes, and sometimes single erythrocytes.
As part of an extended diagnosis aimed at determining the underlying disease that led to the occurrence of hydropericardium, a general and biochemical blood test and a general urinalysis are prescribed. Ultrasound of the abdominal cavity and pelvis, CT scan of the chest and other studies may also be prescribed.
Treatment of pericarditis
The following groups of drugs are used in the treatment of pericarditis:
- Non-steroidal anti-inflammatory drugs that relieve the symptoms of inflammation.
- Antibiotics, antiviral, antifungal and antiparasitic drugs, if the etiological factor is an infectious agent.
- Glucocorticosteroids and cytostatics, if the cause of pericarditis is an autoimmune pathology.
- Treatment of the underlying disease that caused pericarditis - in case of renal failure, hemodialysis can be used, and in case of myocardial infarction - thrombolysis and restoration of blood flow through the coronary arteries.
- If there is a threat of developing cardiac tamponade, they resort to puncture of the pericardial cavity. The purpose of this manipulation is to remove fluid and prevent tamponade. But this puncture is no less important in diagnostic terms. The resulting exudate is subjected to microscopy, bacteriological and cytological examination. It can contain atypical tumor cells or an infectious pathogen.
The prognosis for pericarditis is generally favorable. If pericarditis is correctly diagnosed and treatment is started on time, then a complication in the form of tamponade is extremely unlikely. But it is worth remembering that pericarditis, the treatment of which requires a professional approach, is a rather formidable disease with dangerous complications.
By contacting CELT cardiologists, you can be absolutely sure of timely diagnosis and correct treatment tactics for any cardiac pathology. After all, we employ specialists of the highest category with extensive practical experience. Another argument in favor of CELT is that our clinic has the technical capabilities for a full and comprehensive examination.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Possible complications
The development of complications of hydropericardium is associated with the severity of heart failure.
An increase in the volume of pathological effusion to 1-1.5 liters provokes an increase in symptoms: pressure numbers decrease, shortness of breath worsens, and swelling becomes more noticeable. Advanced hydrocele of the heart leads to the development of tamponade, in which accumulated fluid compresses the heart muscle so much that physiological contractions become impossible. The clinical picture of the condition is accompanied by a pronounced loss of strength, weakness, attacks of suffocation with frequent shallow breathing, a feeling of rapid heartbeat, and episodes of loss of consciousness. In such a case, emergency medical attention is required.
Forecast
Ascites in cancer significantly worsens the general well-being of the patient. As a rule, such a complication occurs in the later stages of oncology, in which the survival prognosis depends on the nature of the tumor itself and its distribution throughout the body.
Life expectancy with ascites depends on the following factors:
- Functioning of the kidneys and liver;
- Activities of the cardiovascular system;
- The effectiveness of therapy for the underlying disease.
The development of ascites can be prevented by an experienced doctor observing the patient. Doctors at the Yusupov Hospital have extensive experience in dealing with various types of cancer. Qualified medical personnel and the latest equipment allow for accurate diagnosis and high-quality, effective treatment in accordance with European standards.
Pulmonary embolism (PE) - symptoms and treatment
Pulmonary embolism (PE) is a blockage of the pulmonary arteries with blood clots of various natures, most often formed in the large veins of the lower extremities or pelvis.
Risk factors for pulmonary embolism include pathological conditions in which there is impaired venous blood return, endothelial damage or endothelial dysfunction, and hypercoagulability disorders.
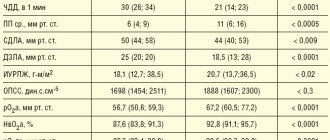
As a result of thromboembolism of the pulmonary arteries, the blood supply to the lung tissue stops, necrosis (tissue death) develops, infarction-pneumonia, and respiratory failure occur. The load on the right parts of the heart increases, right ventricular circulatory failure develops: cyanosis (blue discoloration of the skin), edema in the lower extremities, ascites (fluid accumulation in the abdominal cavity). The disease may develop acutely or gradually over several hours or days. In severe cases, the development of pulmonary embolism occurs rapidly and can lead to a sharp deterioration of the patient’s condition and death.
Every year, 0.1% of the world's population dies from pulmonary embolism. In terms of the frequency of deaths, the disease is second only to IHD (coronary heart disease) and stroke. More patients with pulmonary embolism die than patients with AIDS, breast and prostate cancer, and victims of road accidents combined. The majority of patients (90%) who died from pulmonary embolism were not correctly diagnosed in time and did not receive the necessary treatment. PE often occurs where it is not expected - in patients with non-cardiological diseases (trauma, childbirth), complicating their course. The mortality rate for pulmonary embolism reaches 30%. With timely, optimal treatment, mortality can be reduced to 2-8%.[2]
Symptoms of pulmonary embolism depend on the size of the blood clots, the suddenness or gradual onset of symptoms, and the duration of the disease. The course can be very different - from asymptomatic to rapidly progressing, up to sudden death.
PE is a ghost disease that wears the mask of other heart or lung diseases. The clinic may be infarct-like, reminiscent of bronchial asthma, acute pneumonia. Sometimes the first manifestation of the disease is right ventricular circulatory failure. The main difference is the sudden onset in the absence of other visible reasons for the increase in shortness of breath.
Etiology
PE usually develops as a result of deep vein thrombosis, which usually develops 3-5 days before the onset of the disease, especially in the absence of anticoagulant therapy.
Risk factors for pulmonary embolism
When diagnosing, the presence of risk factors for thromboembolism is taken into account. The most significant of them are: fracture of the femoral neck or limb, replacement of the hip or knee joint, major surgery, trauma or brain damage.
Dangerous (but not so strong) factors include: knee arthroscopy, central venous catheter, chemotherapy, chronic heart failure, hormone replacement therapy, malignant tumors, oral contraceptives, stroke, pregnancy, childbirth, the postpartum period, thrombophilia. In malignant neoplasms, the incidence of venous thromboembolism is 15% and is the second leading cause of death in this group of patients. Chemotherapy treatment increases the risk of venous thromboembolism by 47%. Unprovoked venous thromboembolism may be an early manifestation of malignancy, which is diagnosed within a year in 10% of patients with an episode of PE.[2]
The safest, but still risky, factors include all conditions associated with prolonged immobilization (immobility) - prolonged (more than three days) bed rest, air travel, old age, varicose veins, laparoscopic interventions.[3]
Some risk factors are common to arterial thrombosis. These are the same risk factors for complications of atherosclerosis and hypertension: smoking, obesity, sedentary lifestyle, as well as diabetes, hypercholesterolemia, psychological stress, low consumption of vegetables, fruits, fish, low level of physical activity.
The older the patient, the more likely it is to develop the disease.
Finally, today the existence of a genetic predisposition to pulmonary embolism has been proven. The heterozygous form of factor V polymorphism increases the risk of initial venous thromboembolism by three times, and the homozygous form by 15-20 times.
The most significant risk factors contributing to the development of aggressive thrombophilia include antiphospholipid syndrome with an increase in anticardiolipin antibodies and a deficiency of natural anticoagulants: protein C, protein S and antithrombin III.
The occurrence of hydropericardium in the fetus
Ultrasound examination reveals fetal hydrocephalus. Accumulation of free fluid in the fetal pericardium indicates malformation or edema due to hemolytic disease.
The condition is dangerous for the baby and often occurs with congenital heart defects. The echo-negative bandwidth should be within normal limits.
If examination during pregnancy shows abnormalities in the development of the fetus, the woman should undergo a course of treatment and monitor the condition of the fetus until delivery.
Hydropericardium - how it occurs
The pericardium is the connective tissue membrane of the heart (sac, corium), consisting of two sheets (layers), between which a small volume of transudate is distributed. The volume of this liquid should usually not exceed 15-50 ml.
In some painful conditions associated with increased vascular permeability and impaired absorption in the pericardium, the amount of transudate increases. The fluid is non-inflammatory and contains proteins, trace amounts of fibrin, blood cells and endothelial cells.
Another name for the pericardium is the pericardial sac. My heart aches in this bag. If the amount of fluid between the pericardial valves exceeds 200 ml, the work of the organ becomes difficult, and with a large volume of pericardial effusion, clinical symptoms worsen the patient’s well-being and aggravate heart failure.
A small accumulation of exudate in itself does not cause clinical symptoms or discomfort to the patient. Often hydrocephalus is not detected during life and is discovered only after death.
Causes
Most often, hydrocephalus is one of the symptoms of hydrocephalus; it occurs with congestive cardiac events caused by circulatory disorders. Other causes of hydrocephalus include:
- congenital heart defects
- Hypoproteinemia;
- hypoalbuminemia;
- Hypothyroidism;
- allergic reactions;
- injury;
- anemia;
- anorexia;
- radiation therapy;
- acute and chronic nephritis.
Less commonly, hydrocephalus is caused by taking nonsteroidal anti-inflammatory drugs that dilate blood vessels.
Hydrocephalus occurs with an ischemic heart, with a hemorrhagic symptom, with the growth of malignant tumors. Pericardial effusion may be caused by a mechanical obstruction that prevents blood from flowing out of the pericardium. Such an obstacle is the growing tumors of the mediastinum and lungs.
Common reasons
Hydrocephalus, as one of the symptoms, accompanies heart disease. Non-inflammatory fluid accumulates in the pericardial sac in cardiomyopathies, myocarditis and acute heart failure.
The accumulation of fluid in the pericardial sac is caused by impaired protein synthesis due to deficiency of thyroid hormones in thyroid diseases. Hyaluronic acid, chondroitic acid and mucin accumulate in the tissues, which can retain water in the body.
Water retention occurs throughout the body, including the connective tissues of the pericardium. When this serous fluid enters the pericardium, it causes hydrocephalus. In hypothyroidism, echocardiography shows the accumulation of water in the amount of 15-100 ml, less often the accumulation of transudate in large volumes.