1.General information
According to the definitions existing in modern medicine, a heart attack is a rapid, one-stage focal necrosis (death, death) of a large number of parenchymal, i.e. the main, functionally specialized cells of any tissue or organ. The cause is ischemia, a pathological state of oxygen and trophic starvation due to a lack of blood supply. Outside of medicine, the most famous example of such a scenario is myocardial infarction, while in clinical practice, infarctions of the spleen, brain (stroke), kidneys and other organs are also encountered.
Due to the peculiarities of the anatomical structure and vasculature (blood supply) of the organs of the human respiratory system, pulmonary infarction in most cases develops on the right side and in the lower lobes.
A must read! Help with treatment and hospitalization!
2. Reasons
The direct cause of pulmonary ischemia leading to a heart attack in 15-25% of cases is pulmonary embolism (PE). In this case, the mortality rate, taking into account the insufficient specificity of the observed clinical manifestations and the complexity of intravital diagnosis of pulmonary embolism, can reach 30%.
The pathological basis is a wide range of cardiovascular diseases, including myocardial infarction, infectious carditis, vasculitis, as well as thrombophlebitis of the deep veins of the lower extremities and pelvis.
In addition, pulmonary embolism can develop as a result of complicated childbirth, fractures, and various surgical interventions.
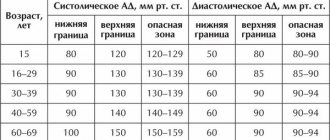
Risk factors are considered to be old age, a hereditary predisposition to thrombosis, taking certain medications (in particular, hormone-containing contraceptives), excess body weight, hypertension and symptomatic hypertension, malignant tumor processes, and some diseases of the hematopoietic system.
Visit our Thoracic Surgery page
First symptoms
A pulmonary infarction does not manifest itself immediately. For the first two to three days after a vessel is blocked, a person may not be aware of the problems. Many people confuse the first symptoms with the discomfort that occurs with angina pectoris. Sometimes pain is possible, as with an acute abdomen. You should be alert to the following symptoms:
- acute chest pain;
- increased pain when coughing, rapid breathing, bending the body;
- shortness of breath that occurs out of the blue, without physical activity;
- when coughing, blood is coughed up (not in everyone, in about half of the cases), complete pulmonary hemorrhage rarely occurs;
- the nasolabial triangle and fingers of the limbs become bluish;
- cold sticky sweat during painful attacks;
- hiccups;
- general malaise, possible fever;
- Some patients vomit.
People suffering from thrombophlebitis and thrombosis, pulmonary hypertension, and frequent relapses of pulmonary embolism are predisposed to pulmonary infarction. Risk factors include age over 60 years, excess weight, pregnancy and childbirth (or caesarean section).
3. Symptoms and diagnosis
Pulmonary infarction does not have a distinct specificity that allows “diagnosis at a glance.” It is known, however, that the patient’s condition most often deteriorates suddenly or quite quickly. Most patients note sharp chest pain, which can easily be mistaken for angina pectoris, an increase in body temperature to subfebrile values (in the case of reactive post-infarction pneumonia, the temperature can reach 39°C or more), unexplained shortness of breath, increased breathing and pulse, cyanotic pallor of the skin, arrhythmic symptoms, a sharp decrease in blood pressure, nausea, vomiting, diarrhea.
In severe cases, these symptoms can take the form of vascular collapse, acute abdomen, atrial fibrillation, disorders of higher nervous activity, including hemorrhagic stroke, cerebral edema and coma. From a third to half of patients note hemoptysis, which, with malignant dynamics, can transform into pulmonary hemorrhage, which, however, is rare. Infection of a necrotic focus can result in gangrene, lung abscess, and sepsis.
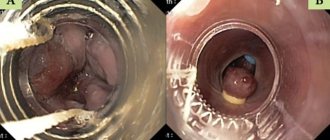
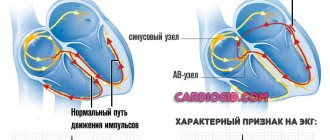
As shown above, the clinical picture of pulmonary infarction is very polymorphic and, at the same time, not very specific, therefore, only a detailed analysis of clinical manifestations in comparison with the results of objective studies allows us to suspect the true cause and exclude symptomatically similar conditions. Of the instrumental methods, the most important are ECG, various, especially angiographic modifications of contrast-enhanced radiography, as well as MSCT, ultrasound examinations of the heart and great vessels in Doppler mode, and lung scintigraphy. A battery of laboratory tests is prescribed.
About our clinic Chistye Prudy metro station Medintercom page!
Pulmonary infarction
Signs
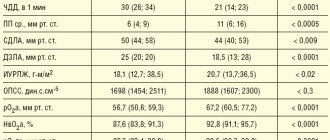
Symptoms and course are determined by the caliber, location and number of obstructed vessels, the state of compensatory mechanisms, and the initial pathology of the lungs and heart. The most common symptoms: sudden onset of shortness of breath (or suddenly intensified); chest pain; pallor with ashy skin tone, less often cyanosis; tachycardia, possible heart rhythm disturbances in the form of extrasystole, less commonly atrial fibrillation; arterial hypotension up to collapse; symptoms of myocardial hypoxia; cerebral disorders (psychomotor agitation, cerebral edema, focal brain lesions associated with hemorrhages, polyneuritis); increased body temperature; cough with mucous or bloody sputum; hemoptysis; dullness of percussion sound; weakened breathing, pleural friction noise and fine moist rales in a limited area; unilateral exudative pleurisy in the presence of peripheral phlebothrombosis, pulmonary pleural pain in the chest. Occasionally, abdominal syndrome is observed, manifested by acute pain in the right hypochondrium, intestinal paresis, pseudo-positive symptoms of Shchetkin, Ortner, Pasternatsky, leukocytosis, persistent hiccups, vomiting, dysgraphia, loose stools (the syndrome is caused by damage to the diaphragmatic pleura). Signs of acute pulmonary hypertension and overload of the right heart (increased cardiac impulse, outward displacement of the right border of the heart, pulsation in the second intercostal space on the left, accent and splitting of the second tone, systolic murmur in the pulmonary artery, signs of right ventricular failure) are observed only with obstruction of large trunks of the pulmonary artery .
Description
The disease is most often based on thrombosis of the veins of the systemic circulation (lower limbs, pelvis, iliac, inferior vena cava, etc.), much less often - thrombosis of the right cavities of the heart. The development of peripheral phlebothrombosis is predisposed by surgical interventions, the postpartum period, chronic heart failure, fractures of long bones, malignant tumors, and prolonged immobilization (in particular, bed rest). Pulmonary vascular thrombosis is caused by stagnation and slowing of blood flow in the lungs, stable pulmonary hypertension, and pulmonary vasculitis. Vessel obstruction is accompanied by a reflex spasm in the pulmonary artery system, which leads to acute pulmonary hypertension and overload of the right heart. Impaired diffusion and arterial hypoxemia occur, which is aggravated by shunting of under-oxidized blood through arteriovenous anastomoses in the lungs and intersystem anastomoses.
Pulmonary infarction most often occurs against the background of existing venous stagnation and is usually hemorrhagic in nature due to the outpouring of blood from the bronchial arteries into the pulmonary tissue, flowing through intersystem anastomoses, as well as the reverse flow of blood from the pulmonary veins. Pulmonary infarction occurs one day after pulmonary vessel obstruction; its full development ends by the 7th day. In some cases, vessel embolism can lead to the development of incomplete infarction in the form of focal pulmonary apoplexy and is not accompanied by irreversible destruction of lung tissue. Infection of a pulmonary infarction leads to the development of perifocal pneumonia (bacterial, candidal) often with abscess formation; with a subpleural location of the infarction, fibrinous or, more often, hemorrhagic pleurisy occurs.
Diagnostics
Various combinations of these signs and varying degrees of their severity are possible, which makes the diagnosis of pulmonary embolism and pulmonary infarction sometimes difficult. The diagnosis is helped by: identifying signs of acute overload of the right side of the heart on the ECG; X-ray examination, which reveals unilateral paresis of the diaphragm, expansion of the root of the lung, focal compaction of any shape, shaded part of the pulmonary field (usually in the area of the bone-phrenic sinus), asymmetry of the shadow and its subpleural location, the presence of effusion without a contour. A decisive role in the diagnosis of pulmonary embolism is played by radioisotope scanning of the lungs and selective angiopulmonography. The prognosis depends on the underlying disease and the size of the infarction.
Treatment
If PE is suspected, heparin and aminophylline are immediately administered; emergency hospitalization is indicated. If the diagnosis is certain, fibrinolytic agents are used in combination with heparin. Treatment with heparin is continued for 7-10 days, followed by replacement with indirect anticoagulants. Along with this, aminophylline, rheopolyglucin, and antibiotics are used.
© Great Medical Encyclopedia
4.Treatment
First aid for suspected pulmonary infarction consists of relieving intense pain and immediate hospitalization of the patient. Further, according to indications (and in the absence of contraindications), anticoagulants, antiplatelet agents, thrombolytics, hormonal vasopressors, and supportive oxygen therapy are used; if there is a reasonable or confirmed suspicion of post-infarction infection, broad-spectrum antibiotics are used in effective doses. In some severe cases, the method of choice, which does not have a reasonable life-saving alternative, becomes thoracic surgical intervention.
It should be emphasized that in case of pulmonary infarction, the time factor is critical. The prognosis is favorable if you seek help in a timely manner and apply an adequate protocol for its provision, when it is possible to quickly and accurately diagnose the cause and prevent possible complications.
Treatment of heart attack-pneumonia
If the cause of pneumonia after a pulmonary infarction is thromboembolic complications, then therapy begins with fibrinolytic agents and anticoagulants.
Symptomatic treatment involves reducing pain by taking analgesics. Etiotropic treatment involves a course of antibiotics depending on the nature of the pathogen. The principle of therapy after myocardial infarction is based on the use of steroid hormones, which contribute to the rapid improvement of general well-being.
Only an experienced doctor can prescribe treatment, based on the results of the studies obtained, and taking into account the individual characteristics of each patient’s body. Pulmonologists, cardiologists, therapists, neurologists and other doctors at the Yusupov Hospital always prescribe a course of treatment for their patients on an individual basis. In this case, the general condition of the patient, age factor, the presence of concomitant diseases and much more are taken into account. Doctors at the Yusupov Hospital are putting back on their feet even those patients who were abandoned in other medical centers.
You can make an appointment with a doctor at the Yusupov Hospital by phone and by filling out the feedback form on the website.