Patient complaints that he does not have enough air are not uncommon. Almost everyone has encountered this phenomenon in their life, but not everyone knows that its systematic appearance can be a symptom of a number of pathological conditions that require immediate treatment.
The problem can occur when inhaling (inspiratory dyspnea) or when exhaling, when due to a lack of air it is difficult to exhale (expiratory dyspnea). If both signs alternate, this is mixed shortness of breath. In the process, the person feels a lack of oxygen and breathes heavily with a whistling sound.
Such conditions are typical for pregnant women, patients suffering from pathologies of the heart, pleura or lungs, as well as with traumatic injuries and neuroses. CELT specialists will help determine the reason why there is not enough air when breathing and alleviate the condition. You can find out the cost of our services by going to the “Services and Prices” tab. To avoid misunderstandings, we recommend that you contact our operators to clarify the numbers.
Why is there not enough air when breathing?
Lack of air in healthy people occurs due to the fact that their body receives less oxygen than it needs. It manifests itself during physical exertion, heavy work, climbing, or stress. There are times when the feeling of lack of air is provoked by too tight clothing, squeezing the body.
In older people, it occurs due to age-related changes in the heart and blood vessels and manifests itself even with light loads. In addition, difficulty breathing, as already mentioned, is part of the symptomatic complex of a number of pathological conditions. If you experience it regularly, you need to seek professional medical help in order to accurately determine the cause. The most common of them are:
- Staying in a poorly ventilated room with stale air;
- Unhealthy lifestyle, accompanied by frequent alcohol consumption and smoking;
- A number of lung diseases;
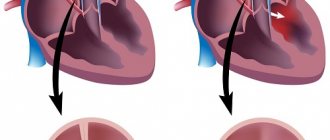
- Pathologies of the cardiovascular system;
- Traumatic chest injuries.
Another initiating factor is the second half of pregnancy. During this period, the uterus seriously increases in volume and provokes the diaphragm to press upward, which does not allow the woman to breathe as deeply as she is used to. The longer the period, the stronger and more often the deficiency is felt, and it occurs not only with minor loads, but also when walking, accompanied by slight dizziness or darkening of the eyes.
The above is especially pronounced in patients carrying twins, triplets, or just a large baby, or suffering from an obstetric anomaly such as polyhydramnios, in which there is an increased volume of amniotic fluid. The problem is particularly alarming against the background of inferior vena cava compression syndrome. When it is present, a woman not only finds it difficult to breathe and lacks air, but also experiences severe dizziness, sudden weakness, fainting and a serious drop in blood pressure.
Conventionally, there are 3 types of shortness of breath
- inspiratory dyspnea (difficulty breathing) – more typical for heart disease
- expiratory shortness of breath (difficulty exhaling) – most often occurs in bronchial asthma due to spasms
- mixed shortness of breath (when both inhalation and exhalation are difficult) – characteristic of a variety of diseases
The most important method of combating shortness of breath is treating the disease that caused it. Once the specialist determines the cause, an effective treatment plan will be determined. For example, for coronary heart disease and myocardial infarction, treatment with tablets is often used. For bronchial asthma - regular treatment with inhalers. Since the main cause of shortness of breath in many cases is low oxygen levels in the body, oxygen therapy is one way to reduce shortness of breath.
Diseases that cause lack of air
| Diseases | Causes, symptoms |
| Cardiological | Patients suffering from pathological conditions characterized by heart rhythm disturbances complain of shortness of breath and lack of air:
People suffer from it in diseases characterized by a lack of blood supply to the myocardium: angina pectoris, ischemia. The severity of the feeling of lack of air depends on the form and degree of insufficiency: in mild cases it is recorded under minor loads or in stressful situations. The problem is manifested by a lack of oxygen and rapid breathing when doing work or while walking. Other symptoms include cyanosis, chest pain, and swelling of the legs. |
| Pleurisy | A feeling of lack of air develops during inflammatory processes of the pleural layers, accompanied by the appearance of fibrin on their surface or the accumulation of exudate in the cavity. Breathing disorders occur due to severe pain of an acute stabbing or dull pulling nature: the patient tries not to inhale deeply so as not to experience them. The above is accompanied by fever, chills, and cough. |
| Laryngeal stenosis | The most common triggering factor for lack of air is pathologies that provoke obstructions and, as a result, limited oxygen supply. This is typical for acute and chronic stenosis:
|
| Lungs | Inflammatory and diffuse lesions of the lung tissue - initiate deficiency due to the fact that part of the lungs is “switched off” from the breathing process. This happens when:
|
| Foreign bodies in the respiratory tract | Blocking the airways with foreign objects can not only make breathing difficult, but also make it impossible. The person feels suffocated, restless, and takes a position in which he can at least somehow breathe. The symptom develops suddenly after accidentally inhaling an object and is accompanied by coughing, lacrimation, and intense salivation. |
| Pulmonary and pleural neoplasms of malignant etiology | Respiratory disorders are accompanied by a complex of specific symptoms, depending on the location of the neoplasia. Common to all are rapid fatigue, appetite disturbances, and rapid loss of body weight. A similar thing happens with pleural cancer or lung adenocarcinoma, in which malignant cells spread along the walls of the alveoli and bronchioles. |
| Traumatic injuries to the lungs and chest | This type of injury is called thoracic. These include:
|
Which doctor should I contact if I have shortness of breath?
If this clinical manifestation is regular, you should first visit your doctor. He will conduct an examination, collect anamnesis - and, based on the information received, send the patient to an appointment with a specialist in pulmonology, cariology, hematology, neurology or endocrinology.
If a patient has a traumatic injury to the chest, he should consult a traumatologist. In cases where shortness of breath is part of an emergency condition - it appears suddenly and sharply - you should immediately call an ambulance.
Diagnosis of air shortage
The initial stages of diagnosis are usually carried out by a therapist. He carries out an examination and collects anamnesis, after which, after analyzing the data obtained, he sends the patient to specialized specialists. To clarify the diagnosis, the latter prescribe the following studies:
- Chest X-ray to detect diseases and injuries;
- Electrocardiography - aimed at identifying heart disease;
- Spirometry - examines the functions of external respiration;
- Laryngoscopy - detects foreign bodies and diseases of the larynx.
Treatment with folk remedies
Folk remedies will help eliminate shortness of breath. They eliminate the inflammatory process, improve heart function, and cleanse blood vessels. But it is better to use them in combination with medications.
A drink to improve blood circulation and cleanse blood vessels. Mix the juice of 10 lemons with 10 medium chopped heads of garlic. Add 1 liter of honey. Place the mixture in a dark place for 7 days. Take 20 ml every day before breakfast. The duration of treatment is 8 weeks.
Advertising:
A drink with a bronchodilator effect. Pour 200 ml of boiling water over 1 tbsp. l chopped astragalus herb. Leave in a sealed container for 1.5 hours. Drink the strained infusion 50 ml 3-4 times a day before meals. The duration of the course is 1 month.
To stabilize the respiratory rhythm, pour 400 ml of vodka and 100 g of dried sunflower flowers. Leave in a cool place for 14 days. Drink 35 drops three times a day before meals.
For shortness of breath caused by diseases of the heart and bronchi, horse chestnut inflorescences will help. Pour 50 ml of alcohol 1 tsp. crushed raw materials. Leave in a dark, cool place for 7 days. Drink 30 drops before breakfast and dinner. Pre-dissolve in 150 ml of water.
Prevention and recommendations for shortness of breath
Physiological shortness of breath goes away on its own after the person has rested. However, if the problem arose acutely and suddenly, the following measures should be taken to alleviate his condition:
- Calm down and sit on a sofa or chair, comfortably resting your back;
- Remove or unfasten tight clothing, a belt that is too tight;
- Provide fresh air by opening a window or door;
- Humidify the air by hanging a pre-wetted sheet near the patient;
- Offer a herbal sedative.
If a person knows about his illness and he has drugs that alleviate his condition, he should be offered to drink them. If he does not feel better within fifteen minutes, he will have to call an ambulance.
There is no specific prevention in this case. However, you can minimize the risk of developing this condition by following these rules:
- Maintaining an active, healthy lifestyle;
- Avoiding excessive physical activity and stress;
- Body weight control;
- Timely treatment of diseases;
- Systematic completion of preventive studies.
Remember: lack of air can be a sign of serious pathological conditions. That is why CELT specialists recommend promptly finding out its causes and taking appropriate measures!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
First aid
If there is a lack of air, it is important to quickly provide first aid to the person. Against the backdrop of suffocation, panic begins. Which only makes the situation worse. First aid rules:
- calm down, don’t panic;
- lie down, sit down to avoid falling in case of fainting. try to move less;
- unbutton all tight parts of clothing;
- ensure free access of air;
- drink cool water;
- if shortness of breath increases, accompanied by chest pain, call an ambulance;
- in case of rapid swelling of the neck, lips, cheeks, take an antihistamine. if possible, give a dexamethasone injection;
- take a sedative. for heart pain - nitroglycerin.
Before the ambulance arrives, you need to record the time of the onset of the attack. Be sure to record what additional symptoms appeared and when. Tell your doctor about all actions taken.