The aortic valve allows blood to flow unidirectionally from the left ventricle to the aorta. When the heart contracts, the leaflets of the aortic valve open, freely allowing blood to pass through, and after contraction, the leaflets close hermetically, preventing the reverse flow of blood from the aorta into the left ventricle.
In the vast majority of people, the aortic valve consists of three leaflets. About 2% of the world's population have a bicuspid aortic valve.
The valve that has three valves turned out to be the most effective and durable.
The bicuspid aortic valve experiences a large mechanical load, as a result of which valve dysfunction is much more common with this structure.
Over a long period of time, the bicuspid valve can successfully perform its assigned function, and the person does not experience health problems.
But, as a rule, sooner or later the function of the bicuspid aortic valve is impaired, as its narrowing or, more rarely, insufficiency develops.
At CELT you can consult a cardiologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Clinic for bicuspid aortic valve and treatment methods
Bicuspid aortic valve is the most common heart defect formed in utero. Pathology is diagnosed in 20 out of 100 people who consult a cardiologist. In healthy people, the valve has three leaflets. They open and close at a certain moment. The valves allow blood to move in one direction. The bicuspid valve develops before birth in the womb. Considered a deviation from the norm. Over a long period of time it may not manifest itself in any way.
Bicuspid aortic valve is a pathology that develops in utero
Root causes
Aortic defect “bicuspid aortic valve” occurs against the background of:
- a pregnant woman suffering from one or another infectious pathology;
- exposure to radiation;
- frequent stressful situations in a pregnant woman;
- smoking and drinking alcohol-containing drinks by a girl while carrying a child;
- genetic predisposition;
- the presence of any serious hereditary disease in one of the parents.
A 2-leaf aortic valve is a pathology that develops in utero. As a rule, this occurs at 5-9 weeks of pregnancy. This period is considered the most critical. When negative factors interact with the body of a woman carrying a child, the risk of abnormalities in the functioning of the heart and vascular system of the fetus increases.
Heart disease can be a consequence of a pregnant woman suffering from influenza and rubella.
Most often, the formation of two valves is associated with a hereditary predisposition. There is a high risk of a child developing a disorder if one of his parents has encountered a disorder.
Women who have had viral diseases during pregnancy are at risk of giving birth to a baby with a bicuspid valve.
Symptoms of pathology
Congenital heart disease “Bivalve aortic valve” can occur for a long time without obvious signs. Patients often find out about the presence of a disorder at an older age.
Usually, up to 10-20 years, the valve functions as expected and does not provoke the occurrence of any negative signs. Symptoms appear gradually. The patient begins to worry:
- Aortic heart defects: causes, diagnosis and treatment
- a feeling of pulsation in the head (its intensity may vary);
- feeling of strong heartbeat;
- sinus tachycardia;
- fainting and periodic loss of consciousness;
- regular and obvious dizziness;
- disturbance in the functioning of the visual organs;
- difficulty breathing even with the most minor physical exertion;
- pain syndrome in the chest.
Fatigue and fainting may be signs of heart disease
With pathology, the patient's blood flow is significantly impaired. Symptoms can vary in intensity. The bicuspid aortic valve in children does not cause discomfort for a long time. Gradually, intolerance to any type of physical stress may appear. From time to time, a small patient may complain of aching headaches.
A bicuspid aortic valve in a child provokes memory impairment.
In infancy, pathology can manifest itself as a weak sucking reflex, excessive tearfulness and lethargy. The baby is not gaining weight well and is constantly spitting up.
If left untreated, the pathology becomes chronic. The deviation is characterized by the following symptoms:
- heart rhythm disturbances;
- constant presence of difficulty breathing;
- night cough;
- swelling.
Coughing is one of the signs of chronic disease
Patients are at high risk of developing additional pathologies. When they appear, all symptoms become more pronounced.
Diagnostic measures
CHD - bicuspid aortic valve can be diagnosed using:
- Ultrasound;
- standard ECG and daily monitoring;
- radiographs of the lungs.
First of all, the cardiologist questions the patient and identifies complaints. The doctor determines the possible root causes of the development of the disorder.
Particular attention to the initial examination. Children with heart defects are significantly behind their peers in physical development. When diagnosing a disorder in an infant, a doctor may notice bluish skin, muscle hypotonicity, and slow weight gain.
- Heart defects: classification, diagnosis, treatment and prevention
If a bicuspid valve is suspected, an ECG of the heart is mandatory.
Laboratory tests are necessary to determine the general condition and identify associated abnormalities.
The main diagnostic method is ultrasound. This is the only way to confirm the presence of a bicuspid aortic valve. Other studies are required to clarify the extent of damage and select therapeutic measures.
Features of therapy and life activity
Bicuspid aortic valve does not always require treatment. Therapy is selected on an individual basis, so the patient needs to be diagnosed annually for prevention.
Surgery is considered difficult, so it is performed only if there are negative symptoms
Treatment is not necessary if the patient does not have negative symptoms. The condition is normal. At an advanced stage of deviation, surgical intervention is prescribed - installation of a prosthesis. After the procedure, you will need to take medications. The types of implants are described in the table.
>Type of prosthesis Description Biological Made from tissues of animal origin. Mechanical Made from metal compounds.
The operation is considered difficult. Can lead to:
- severe disruption of blood flow;
- destruction of biological processes;
- arterial thromboembolism.
The patient must take medications in courses. The cardiologist prescribes:
A bicuspid aortic valve cannot be treated on its own. Medicines should only be prescribed by a doctor.
Proper nutrition, frequent walks and giving up bad habits are the main recommendations when pathology is detected.
- Why is aortic valve stenosis dangerous?
If the heart valve has 2 leaflets, the patient must completely change his lifestyle. You should give preference to a balanced diet. Special formulas are recommended for infants. Regular walks outside are required.
The patient is recommended to sign up for swimming. Therapeutic exercises are indicated daily. Physical activity should be moderate. The patient may be referred for dissection of the bicuspid aortic valve.
The patient should not deny himself sports. However, its type is selected on an individual basis. Maximum loads are contraindicated. People with a bicuspid aortic valve are most often not accepted into the army.
The doctor can make a decision about surgery only after a thorough examination.
Prognosis and life expectancy
The prognosis for the future with bicuspid aortic valve in children is individual. In the absence of a clinical picture of deviation and deterioration of the condition, the pathology may not cause any discomfort. The patient will live a normal life.
After surgery, people live 12-17 years. This directly depends on the way of life and the individual characteristics of the body. If all doctor's instructions are followed, life expectancy will be long.
In other words, the prognosis for life with a bicuspid aortic valve is often favorable. The main thing is moderate physical activity and regular diagnostic testing.
Most patients with bicuspid valve lead normal lives.
Prevention of deviation
Preventative measures are necessary to maintain good health and reduce the risk of complications. These include:
- maintaining a correct lifestyle;
- eating healthy foods with plenty of essential vitamins;
- outdoor sports;
- regular walks outside;
- alternating physical activity with mental activity.
The patient should avoid stress. You should absolutely not overwork yourself. It is important that the load alternates with rest. You need to give up bad habits. The diet should include as many fruits and vegetables as possible. The 2-leaf aortic valve is not dangerous and if the doctor’s recommendations are followed, the patient will not experience any discomfort.
The video talks about the role of the aortic valve and what happens if its operation malfunctions:
Medical Internet conferences
Introduction
Bicuspid aortic valve is the most common congenital heart defect. Remaining asymptomatic for a long time, it may eventually become complicated by the development of aortic stenosis or aortic insufficiency. Bicuspid aortic valve is also associated with aortic aneurysm and dissection. Given the high prevalence of this defect and the severity of complications, it is believed to cause more deaths than all other congenital heart defects combined [1].
Introduction
Bicuspid aortic valve is the most common congenital heart defect. Remaining asymptomatic for a long time, it may eventually become complicated by the development of aortic stenosis or aortic insufficiency. Bicuspid aortic valve is also associated with aortic aneurysm and dissection. Given the high prevalence of this defect and the severity of complications, it is believed to cause more deaths than all other congenital heart defects combined [1].
Introduction
Bicuspid aortic valve is the most common congenital heart defect. Remaining asymptomatic for a long time, it may eventually become complicated by the development of aortic stenosis or aortic insufficiency. Bicuspid aortic valve is also associated with aortic aneurysm and dissection. Given the high prevalence of this defect and the severity of complications, it is believed to cause more deaths than all other congenital heart defects combined [1].
Clinical case
Patient A., 51 years old, was admitted on March 4, 2021 with complaints of shortness of breath with difficulty inhaling and exhaling when going up to the 4th floor; dizziness when moving to a vertical body position; attacks of rapid heartbeat that occur in a lying position, lasting a few seconds, stopping on their own.
Considers himself sick for a year and a half (from the age of 49), when dizziness first began to bother him. Since March 2021, shortness of breath occurs during physical activity. Over the course of six months, an increase in blood pressure to 140 and 90 mm was repeatedly recorded. rt. Art. Since September 2021, attacks of rapid heartbeat occur occasionally at rest. An examination at a local clinic revealed a congenital heart defect: bicuspid aortic valve. Sent to the cardiology hospital.
From the life history it is known that the patient served in the army, coped well with physical activity, currently works as a mechanic at a factory, and previously smoked. As a child I had frequent sore throats. Among the operations undergone, he noted a tonsillectomy at the age of 12 years.
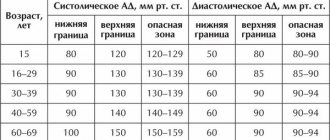
Upon examination, an asthenic physique attracted attention. On palpation, a high, intense, resistant, dome-shaped apical impulse was detected in the 5th intercostal space 1 cm outward from the left midclavicular line. During percussion, the left border of relative cardiac dullness was shifted to the left and coincided with the apical impulse. On auscultation, heart sounds were rhythmic, heart rate 72 per minute. At the top, the first tone was slightly weakened, but louder than the second tone. Above the aorta, the second sound was weakened, a rough systolic murmur was heard, carried through to the vessels of the neck and the entire precordial region. Blood pressure was 140 and 80 mm Hg. The radial artery pulse was the same in both arms, rhythmic with a frequency of 72 per minute.
There were no changes in general and biochemical blood tests as of 03/05/2019.
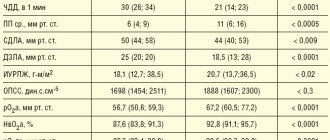
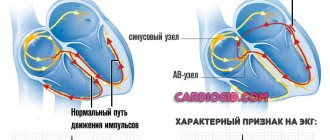
During electrocardiography on March 4, 2021 (Fig. 1), sinus rhythm was recorded with a frequency of 72 per minute. The electrical axis of the heart was located horizontally. Signs of left atrium enlargement were determined.
Holter ECG monitoring dated March 11, 2021, which lasted for 23 hours, showed the dominant rhythm was sinus. The average heart rate was 54 per minute. A paroxysm of ventricular tachycardia consisting of 5 contractions with a frequency of 129 per minute, 24 single ventricular extrasystoles was recorded. Supraventricular ectopic activity consisted of 288 contractions, of which 12 atrial groups lasting from 3 to 8 contractions with a frequency of 105 to 129 per minute, 12 episodes of paired atrial extrasystoles, including with aberration of intraventricular conduction, 201 single atrial extrasystoles. There were no diagnostically significant dynamics of the ST segment.
X-rays of the chest organs with a contrast-enhanced esophagus dated March 5, 2021 (Fig. 2) revealed signs of dilation of the ascending aorta, a slight enlargement of the left ventricle, and right-sided scoliosis of the thoracic spine.
Echocardiography on March 5, 2021 (Fig. 3) visualized a bicuspid aortic valve and multiple calcifications at the base and distal parts of the leaflets. Slight aortic regurgitation was detected; aortic stenosis, the degree of obstruction is severe, the maximum gradient is 79 mm Hg, the average gradient is 46-50 mm Hg, slight expansion of the aortic root (diameter 4.2 cm). There was a pronounced expansion of the ascending aorta (diameter 4.6-4.8 cm), slight pulmonary hypertension: systolic pulmonary artery pressure 36 mm Hg. Slight left ventricular hypertrophy was determined: myocardial mass index 107 g/m², slight enlargement of the left atrium (end-systolic volume 74 ml). The left ventricular ejection fraction was 66%. A pseudonormal type of transmitral blood flow was recorded.
Coronary angiography on March 6, 2021 revealed stenosis of the right coronary artery in the second segment up to 80%.
The patient was diagnosed:
Congenital heart defect: bicuspid aortic valve. Combined aortic disease: aortic stenosis of III-IV degree. Aortic insufficiency degree I. Arterial hypertension stage III risk 4.
Complications: Chronic heart failure stage IIa, functional class 2.
Treatment was prescribed: acecardol 100 mg once a day in the evening, cozaar 50 mg once a day in the morning, bisoprol 2.5 mg once a day in the evening.
A council of cardiac surgeons recommended aortic valve replacement for the patient.
Discussion
The incidence of bicuspid aortic valve ranges from 0.6% to 2% [1]. The disease occurs 3 times more often in men than in women.
The frequency of detection of pathology in first-degree relatives of a patient is 9% [2]. In recent years, views on this pathology have changed significantly, and today, when talking about this defect, they mean valvulo- and aortopathy of hereditary origin, caused by molecular and histological changes in the connective tissue [3]. The genetic mechanisms leading to the formation of a bicuspid aortic valve are not well understood. Currently, NOTCH1 remains the only confirmed candidate gene whose mutation is associated with both familial and sporadic cases of bicuspid aortic valve with concomitant thoracic aortic aneurysm [4].
The clinical picture in patients with a bicuspid aortic valve can vary from severe manifestations of valve dysfunction in infancy to their complete absence in older people [1]. In the presence of aortic stenosis or aortic insufficiency, patients are bothered by headaches, fainting, and dizziness, as in our patient. Clinical manifestations may also be caused by dilation of the ascending aorta (aortopathy), coarctation of the aorta, and the development of infective endocarditis [2].
Signs of a bicuspid aortic valve can be detected by auscultation. In patients with a normally functioning bicuspid aortic valve, a systolic ejection murmur is heard at the apex of the heart and in the projection of the aorta. In children predominantly 7-11 years old, aortic systolic clicks can be detected in the 2nd intercostal space to the right of the sternum [5]. With aortic regurgitation, a diastolic murmur is heard above the aorta and at Botkin's point, and in the presence of aortic stenosis (as in our patient), a rough systolic murmur is heard above the aorta, conducted to the vessels of the neck.
The electrocardiogram is usually normal, but there may be signs of left ventricular hypertrophy. The mainstay of diagnosis is echocardiography [6].
Currently, the following types of surgical interventions can be performed in children with a bicuspid aortic valve due to its stenosis: balloon valvuloplasty, valve replacement with mechanical and biological prostheses, Ross operation and reconstructive plastic surgery on the aortic valve [7].
According to Petrushenko D. Yu. and co-authors, satisfactory results of treatment of critical aortic stenosis in newborns and children in the first months of life were reported both when performing balloon valvuloplasty and open reconstructive plastic surgery on the valve. Both procedures are palliative: sooner or later the patient will again need surgical treatment, since after balloon valvuloplasty valve insufficiency develops, and after open repair there is a risk of developing restenosis [7]. Aortic valve replacement is performed in children and adolescents in whom previous balloon valvuloplasty has resulted in aortic insufficiency. The operation is performed during the period when the growth of the aorta is completed [5]. Surgical treatment of bicuspid aortic heart disease in adults in tactical terms does not cause much discussion: unlike children, the issue of tactics and surgical techniques is much simpler to solve - the vast majority of patients require aortic valve replacement [3]. Patients with large aortas have a significant risk of mortality within 5 years due to aortic dissection or rupture, especially when the aortic diameter reaches 6 cm [8]. In case of bicuspid aortic valve, surgery on the ascending aorta is indicated in the case of: enlargement of the root or ascending aorta >55 mm; enlargement of the root or ascending aorta >50 mm and the presence of other risk factors; enlargement of the root or ascending aorta >45 mm during planned aortic valve replacement surgery. With planned replacement of the ascending aorta (including the aortic root), surgical mortality ranges from 1.6-4.8% [9].
It is known that in patients with Marfan syndrome, β-blockers and/or losartan can slow down the dilatation of the aortic root and reduce the risk of aortic complications. By analogy, it is common clinical practice to recommend these drugs to patients with a bicuspid aortic valve and enlargement of the root or ascending aorta [10]. Therefore, our patient was prescribed bisoprolol and cozaar.
In the presence of a bicuspid aortic valve, as with other heart defects, when performing invasive medical interventions accompanied by bacteremia, it is necessary to prescribe antibiotics to prevent infective endocarditis.
The prognosis for bicuspid aortic valve is generally favorable. However, more than half of all patients in the world who require aortic valve replacement are patients with this heart defect [5]. According to Pelekh D.M., who analyzed the outcomes of surgical treatment of patients with aortic stenosis, including patients with bicuspid valvulopathy, aortic valve replacement leads to good immediate and long-term results: a decrease in the size of the left chambers of the heart, a decrease in the severity of myocardial hypertrophy, and an improvement in myocardial contractility left ventricle and, consequently, the well-being of patients. Most patients progress to NYHA functional class 1–2. After surgery, acute cerebrovascular accidents, prosthesis thrombosis, and infective endocarditis may develop. Mortality in the early postoperative period ranges from 9.3 to 12.3% [11].
Conclusion
Bicuspid aortic valve is a common heart defect, the presence of which predisposes to severe complications. The disease may not appear clinically for a long time. To prevent the development of complications, it is necessary to timely identify this heart defect and carefully monitor the patient to timely determine indications for surgical treatment.
Causes
The pathology develops during the period of intrauterine development, therefore it is a congenital heart defect. This happens between 6 and 8 weeks. During this period of time, the active process of formation of internal organs in children begins. The two doors are fused together, forming only two moving parts. They take on the functions of the missing component of the heart muscle. In a child, this pathology develops under the influence of a number of provoking factors. The main reasons for the formation of a bicuspid aortic valve include:
- suffered by the mother during the period of gestation of various infectious diseases;
- the influence of radiation, exposure caused by X-ray examination;
- harmful effects of the environment due to poor ecology;
- severe stress, anxiety, psycho-emotional disorders and shocks;
- abuse of alcohol and tobacco products while carrying a baby;
- a predisposition that is inherited if the baby’s parents have cardiovascular system defects;
- genetic predisposition to pathologies associated with connective tissues.
If parents have a bicuspid aortic valve as a congenital pathology, when planning conception and during gestation, it is necessary to carefully monitor all processes, carry out comprehensive diagnostics and take timely measures to ensure the normal functioning of the baby’s cardiovascular system.
Symptoms
In a child, a congenital pathology may not manifest itself in any way for a long time. Symptoms can intensify as he grows up and gradually increases the load on his body, which is in the stage of active development and formation. There are cases when a congenital valve defect was discovered when the child reached adolescence and adulthood. With such congenital heart disease as a bicuspid aortic valve, symptoms manifest themselves in the form of the following characteristic signs:
- Strong pulsation, which is felt in the neck, head or projection of the heart muscle. The pulsation intensifies when the patient assumes a supine position. Such symptoms manifest themselves due to high myocardial emissions and elevated pulse rates.
- Sinus type tachycardia. Its manifestations are characterized by rapid heartbeat. It can occur for no apparent reason, that is, in a state of rest.
- Fainting, dizziness. They are observed quite often in patients. They can develop with moderate physical activity, or when a person suddenly changes the position of his body. This happens if the patient stands up suddenly. These symptoms are caused by a lack of blood circulation in the brain. Such signs are relevant when serious changes occur in the structure of the valves.
- Dyspnea. It first appears if the patient has undergone significant physical exertion. But over time, symptoms are observed even in a state of complete rest. If the systolic function assigned to the left ventricle decreases, the person exhibits signs of orthopnea. As the disease progresses, myocardial asthma and pulmonary edema gradually develop. Because of them, the patient faces dangerous attacks of suffocation.
- Increased and excessive fatigue with minimal activity, a feeling of general weakness throughout the body.
- A person’s vision noticeably decreases, even if it was initially 100%.
- In the region of the myocardium, pain is felt behind the chest, which has no emotional or physical provoking factors. Can be observed at rest. If the aortic valve is severely damaged, the pain becomes pressing and squeezing, lasts for a long time and does not go away after taking potent drugs. The most difficult pain for the patient is the attacks of pain that occur at night. At the same time, sweat is actively released. This condition is caused by hypertrophy of the affected ventricles.
Only hardware diagnostics can detect a bicuspid aortic valve in a person as a congenital pathology of the cardiovascular system. Therefore, at the first signs, seek advice from a cardiologist. If symptoms are detected in time, the diagnosis is confirmed and treatment is started, the functional cardiovascular system will suffer minimally. It is often possible to return patients to normal life and restore blood flow. Prediction is made based on the results of the examination and the therapeutic methods prescribed for treatment.
The prevalence of bicuspid aortic valve (AAV) ranges from 0.5 to 2% among all congenital heart defects. Among patients with bicuspid AK, more than 80% are male [41, 68, 69]. It is generally accepted that bicuspid AV is not a variant of the development of AV, but a congenital heart defect [5, 6, 12, 13, 20, 30, 36, 40, 45, 56, 59, 62, 68, 70]. In patients with bicuspid aortic valves, 66% of cases have aortic insufficiency of varying degrees [45]. Indications or contraindications for surgical treatment of patients with bicuspid aortic valves are not clearly defined.
According to C. Ward, in terms of incidence rate, bicuspid aortic valve ranks first among all congenital heart defects [70]. According to Yu.V. Belousov [1], in 80% of cases, pathological changes in the aortic root are caused by congenital pathology of the aortic valve (bicuspid and extremely rarely monocuspid aortic valve).
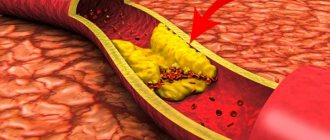
In 1926, M. Abbott and W. Hamilton [3] described the relationship between bicuspid aortic aneurysm and rupture of aortic aneurysm in an adult patient. Most often, bicuspid aortic valve is combined with acquired diseases such as aneurysm of the ascending aorta, stenosis and insufficiency of the aortic valve, aortic dissection and rupture, and bacterial endocarditis [4, 12, 37, 51, 56-58]. The association between bicuspid aortic valves and aortic stenosis, regurgitation, and infective endocarditis has been known for more than 150 years, and the relationship between bicuspid aortic valves and aortic dissection and rupture has been known for more than 75 years [3, 54]. V. McKusick et al. [42] in their work supported the theory of the histopathology of the aortic wall in patients with bicuspid aortic valve and dissection of the ascending aorta, in particular linking it with medianecrosis. The term “medionecrosis” was introduced by O. Gsell [27, 31] in 1928, taking a strong position in the pathogenesis of aneurysms and dissections of the ascending aorta. Clinical studies [39] performed in recent years clearly demonstrate the relationship between bicuspid aortic valves and degenerative changes in the wall of the ascending aorta, which consist of elastin fragmentation and disruption of the orientation of smooth muscle cells. These results are consistent with reports by other authors indicating similar changes in the aortic wall during its dissection in patients with bicuspid aortic valves [26], with aneurysms of the ascending aorta [35] and with anuloaortic ectasia [21, 61]. Such histological changes are detected in bicuspid aortic valves (in 45% of patients gross changes in the aortic wall were found) much more clearly than in tricuspid aortic valves (only in 9% of patients) [39]. In the work of M. Bauer et al. [8] conducted morphometric studies of the aortic wall obtained during surgery in 107 patients with bicuspid aortic valves. It was shown that in patients with bicuspid aortic valves, the elastic lamina of the aortic media is thinner than in patients with tricuspid aortic valves, while the total thickness of the aortic media did not differ significantly in both groups. Similar data were obtained by Mauro de Sa [39], M. Nataatmadja [44].
Although the bicuspid aortic valve can function normally, it is a substrate for the occurrence of aneurysm and dissection of the ascending aorta [25, 48, 70]. According to a study conducted by R. Beroukhim et al. [9], during an echocardiographic examination of children (n=101) with bicuspid AV and 98 children with tricuspid AV, the sizes of the ascending aorta in the first group of children were larger than in the second (2.3±0.6 and 1.8±0. 5 cm, respectively; p<0.0001).
In bicuspid aortic aneurysms, aneurysms of the ascending aorta are localized along its anterior surface. In addition, diffuse dilatation of the ascending aorta is common. Dissection or rupture of the aortic wall in the presence of a bicuspid aortic valve occurs 8–10 times more often than in a tricuspid aortic valve [7, 13, 18, 22, 36, 67, 70]. According to the International Registry of Acute Aortic Dissections, the incidence of dissections with a diameter of the ascending aorta of more than 5.5 cm is statistically significantly higher in patients with bicuspid aortic valves [65]. When comparing different age groups of patients with bicuspid and tricuspid aortic valves, the group with bicuspid aortic valves showed a statistically significantly higher incidence of ascending aortic aneurysms [6, 15, 29, 67, 71]. The age group was dominated by patients under 40 years of age [15, 38]. Even with a normally functioning bicuspid aortic valve, aneurysms and aortic dissection occur in 50–69% of cases [45, 52]. According to foreign authors, the rate of increase in aortic diameter in patients with bicuspid aortic valves ranges from 0.2 to 1.9 mm per year [15, 16, 23, 38, 47]. Some studies [63] demonstrated that the expansion of the ascending aorta in patients with bicuspid aortic valves was 2.1 mm per year with an initial aortic diameter of 35-40 mm and even 5.6 mm per year with a diameter of 60 mm.
Aortic diameter is an important prognostic criterion for aortic dissection and rupture [14, 15, 19]. A study of 1,600 cases of aortic aneurysm with dissection found that for aortic diameters greater than 60 mm, the annual rupture rate was 3.6% and the annual dissection rate was 3.7%. The overall incidence of all these complications, including deaths, was 14.1%, i.e. 2 times higher than the incidence of similar complications in patients with aneurysms with a diameter of 50 mm [19]. The average diameter of the ascending aorta at dissection or rupture in patients with bicuspid aortic valves in this study was 59–60 mm (range, 3.0 to 10 cm) [14, 65]. In separate studies examining dissections of aortic aneurysms in patients under 40 years of age, in 24% of cases dissections were recorded in patients with bicuspid aortic aneurysms [26].
Despite the above, the authors [55] argue that the presence of a bicuspid aortic valve does not affect the occurrence of an aneurysm of the ascending aorta. O. Yoshihiro [72], based on a similar opinion, performs plasty of bicuspid aortic valve, demonstrating good immediate results. However, it is unknown how a bicuspid aortic valve will behave in the long-term postoperative period.
Back in 1886, W. Osler [49] put forward a hypothesis about the relationship between infective endocarditis and bicuspid aortic valve, in which he was not mistaken. The results of further studies conducted by a number of authors [10, 24, 48, 50, 64] show that in patients with bicuspid aortic valves, the incidence of infective endocarditis varies from 10 to 30%. According to S. Higgins [33] and A. Stewart [66], of the total number of observations, the substrate of infective endocarditis was in 25% of cases the leaflets of the bicuspid aortic valve, with the highest frequency of lesions in children and adolescents. In observations conducted by R. Grant et al. [28], in patients with bicuspid aortic valves younger than 40 years of age, the cause of death in 30% of cases was infective endocarditis. According to the authors [4, 58], in patients with bicuspid aortic valves, infective endocarditis is the cause of severe valvular insufficiency and leaflet perforation with a frequency of 43 to 60%.
It has been proven that bicuspid aortic valve serves as a trigger in triggering the development of aneurysms of the ascending aorta, stenosis and insufficiency of the aortic valve, dissection and rupture of the aorta, and endocarditis. However, in none of the studies studied, the authors [9, 15, 32, 46, 52, 71, 72] do not answer the question of why aneurysms of the ascending aorta are more common in patients with bicuspid aortic valves than in patients with tricuspid aortic valves.
The lack of understanding of the mechanism leading to the development of ascending aortic aneurysms in bicuspid aortic valves is that the aortic root is not considered in terms of physical processes during the cardiac cycle. In structural and functional terms, the valves of the aortic valve and the aortic root should be considered as a single whole. The components of the aortic root are the aortoventricular crest, commissural rods and arched ring, connected into a complete frame that maintains the stereometry of the aortic bulb and controls the operation of the leaflets. The fibrous frame of the AC serves as a stress concentrator; this structural physiological structure reduces the load on the valve leaflets due to the redistribution of forces in systole and diastole [2].
The work cycle of the heart consists of rhythmic processes of systole and diastole, indirectly replacing each other. In the diastole phase, the left ventricle is filled with a volume of blood, which in the systole phase is ejected through the aortic valve into the ascending aorta. The valve leaflets open under the pressure of the blood volume created in the left ventricle of the heart according to the Frank-Starling law. The closure of the AV valves occurs under the influence of the pressure force of the blood volume, which interacts with the AV valves according to the principles described by B. Bellhouse [11]. If the valves of the aortic valve are not changed, the volume of blood is retained in the ascending aorta until the next volume arrives. Anatomically, the unit area of the aorta is designed for a uniform pressure force of a certain volume of blood arising during the diastole of the left ventricle and the reverse flow of blood under the influence of gravity. This volume and this force of fluid pressure on the aortic wall are created due to the distribution of the fluid volume between the three valves of the aortic valve. Thus, the pressure force of the shock wave created by the reverse flow of blood volume in the ascending aorta is dampened. To better understand these processes, it is necessary to know the difference between “fluid pressure” and “fluid pressure force,” since these concepts are not equivalent. The pressure of a liquid is a constant value equal to the product of the density of the liquid, the height of the liquid column and the acceleration of gravity. Pressure force is the product of fluid pressure and the surface area on which this pressure is applied. Now, considering the aorta as a vessel containing fluid, we can understand that the pressure force exerted on its bottom, and in particular on the AC, falls evenly on all 3 leaflets. The shock wave of the reverse flow of fluid is “quenched” evenly and the pressure force is evenly distributed on the walls of the aorta; overload of the fibrous ring of the aortic valve, commissural rods and sinotubular crest does not occur. Thus, conformational changes in the aortic root, which are a predisposing factor in the development of aneurysm of the ascending aorta and aortic insufficiency, are prevented.
In bicuspid aortic valves, the spatial arrangement of the aortic root structures is disrupted. The AC valves are formed as right and left or as anterior and posterior [2]. The latter have different areas [70], in contrast to the tricuspid AC, in which the area of the valves is approximately equal or differs slightly. These anatomical changes, due to the uneven distribution of pressure on the valves of the aortic valve, lead to overload of the previously identified structures and lead to the formation of aneurysms of the ascending aorta and aortic insufficiency. The pressure force created by the reverse flow of fluid in the ascending aorta during diastole “falls” perpendicularly onto both leaflets of the bicuspid aortic valve. The greater the surface area on which this force is exerted, the greater the pressure force. Considering the size of the unchanged ascending aorta, its shape resembles a cylinder tapering upward, with this shape of the vessel, the force of not only the poured liquid acts on the bottom, but also the pressure force of the walls of the vessel itself (in our case, the aorta). The pressure force of the reverse blood flow in a bicuspid aortic valve on the leaflet with a larger area is greater than on the leaflet with a smaller area. This force is increased by the force of pressure on the walls of the vessel, which inevitably entails overstraining the structures of the AC that are under maximum load - the commissures and the attachment points of the pathologically altered valves of the AC - the walls of the sinuses of Valsalva. In these zones, the greatest stretching and bending of the valves occurs, which leads to trophic tissue disorders, expansion of the ascending aorta, calcium deposition on the valves of the aortic valve, as well as aortic dissection [2]. With bicuspid aortic valves, not only conformational changes occur, but also changes in the flow of the blood stream passing through the aortic ring. In patients with bicuspid aortic valves, regardless of the presence of an ascending aortic aneurysm, so-called nested “helical flows” were found at peak systole in the ascending aorta. These flows play a trigger role in the occurrence of an aneurysm of the ascending aorta. No similar flows were found in patients with tricuspid aortic valve [43].
Taking into account the presented data, it can be stated that bicuspid aortic valve is one of the reasons for the formation of an aneurysm of the ascending aorta. The question of the surgeon's tactics when detecting a bicuspid aortic valve during surgery, during intervention for an aneurysm of the ascending aorta, remains unresolved. If the bicuspid aortic valve is wealthy and the patient’s age at the time of surgery is over 60 years, it is logical to preserve the aortic valve, since its service life will be longer than the patient’s life expectancy. Another question is if we are dealing with a young patient, younger than 50-55 years old. The question of the advisability of re-implantation of a bicuspid aortic valve into an aortic root prosthesis is currently open.
Question of military service
Some young guys plan to enter naval schools or go to military service after reaching adulthood. Others want a reprieve. Therefore, a natural question would be whether an army with such a diagnosis as bicuspid aortic valve is possible. If, due to a valve defect, reverse blood flow is observed, that is, it flows in the opposite direction from the norm, then conscripts must be released from service. They are given a deferment and recognized as having limited fitness. This corresponds to category B.
But in the absence of signs of reverse flow and other complications, the congenital defect itself is not considered an argument for preventing conscription.
Diagnostic methods
The bicuspid aortic valve can only be examined using instrumental diagnostic methods. But first, a cardiologist conducts a visual examination if such a pathology is suspected. With BAV, patients experience paleness of the skin or some areas with bluish tints. External signs also include increased pulsation. There are several basic instrumental diagnostic methods that can confirm the fact of a congenital defect and assess the patient’s current condition.
- Using ultrasound or echocardiography, it is possible to determine the degree of damage to the affected valves, as well as confirm or refute the development of an aortic aneurysm.
- The method of vascular Dopplerography or ultrasound dopplerography is used to determine the current state of the valve structure, the speed of blood flow through them and cavities.
- To identify symptoms of blood stagnation, the fact of an enlarged ventricle and aorta, an x-ray method is used. The x-ray scans the chest and provides the doctor with relevant information.
- If it is necessary to check the heart muscle for pathological noise, resort to phonocardiography.
The most effective and useful examination method for such pathology is considered to be ultrasound. Based on the results of the instrumental study, the doctor forms an individual tactic for treating the disorder.