Changes in the veins of the testicular pampiniform plexus usually occur during adolescence. The incidence of the disease reaches 20% and it is considered one of the main causes of male infertility. The pathology manifests itself as dilation of the veins in the upper part, mainly of the left half of the scrotum.
The generally accepted method of treatment is surgery. Its goal is to interrupt reflux from the left renal vein into the pampiniform plexus along the testicular vein. All modern techniques have a single principle of intervention with some technical differences.
In 95-98% of cases, it is possible to interrupt the pathological blood flow. It is not possible to do this without surgical intervention, therefore conservative treatment methods are not considered recommended for correcting the pathological condition of the testicular vein.
Causes of varicocele
Varicocele is a disease that occurs in men and results in dilation of varicose veins in the testicles. This pathology affects the full functioning of blood vessels and increases pressure in the veins. Varicocele is more common on the left testicle, rarely on both.
IMPORTANT! Information from the article cannot be used for self-diagnosis and self-medication! Only a doctor can prescribe the necessary examinations, establish a diagnosis and draw up a treatment plan during a consultation!
The main reasons causing dilation of the veins of the testicles include:
- genetic predisposition to varicose veins;
- physical activity with constant lifting of weights;
- features of the anatomical structure that contribute to pinched veins in the genital organs;
- neoplasms (both benign and malignant);
- constipation and diarrhea in the chronic stage;
- irregular sex life;
- increased body weight;
- various inflammatory processes.
Classification
There are primary and idiopathic varicoceles, caused by damage to the venous system; in the supine position, the veins collapse and return to normal. Symptomatic varicocele, or secondary, is provoked by kidney disease and compression of the inferior vena cava due to neoplasms. It may not cause pain; the shape and size of the veins do not decrease when lying down. Depending on the location, there are left-sided, right-sided or bilateral varicoceles. Due to anatomical features, the left testicle is most often affected; right-sided and bilateral ones are less common.
Depending on the degree of damage to the veins, three stages of varicocele are distinguished:
- The first is determined only by palpation at the moment of tension of the abdominal muscles in a standing position.
- The second is that the expansion of the veins is well determined visually, while the testicles retain normal size and consistency.
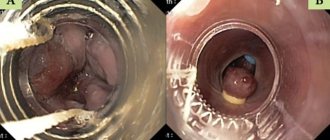
- The third - cluster-shaped swollen veins in the pampiniform plexus are visible visually, are clearly visible in the photo, and are characterized by a decrease in the size of the testicles and their density.
Varicocele, unfortunately, is not a cosmetic defect, but a threat to become infertile. The dilated veins create an enlarged layer around the testicle, the temperature increases, and the number and mobility of produced sperm decreases. This can happen at any stage of the disease.
Treatment of varicocele and effect on male infertility
Treatment of varicocele is carried out exclusively by surgery, since only surgery can give the best effect. Read more.
There are different types of operations. It is believed that at present the microsurgical method of surgical treatment is the most effective: it allows surgical intervention to be performed with the least tissue damage as a result, rehabilitation time takes less time.
The operation helps restore blood flow in the testicles and restore normal spermatogenesis (production of a sufficient number of living and anatomically correct sperm). Improving the quality of sperm and eliminating pain will allow you to have a full sex life, without the threat of infertility. From childhood, varicocele prevention should be done, since hereditary acquisition of the disease is possible. It is important to see a urologist regularly.
Dr. Tkachenko Grigory Gennadievich – urologist-andrologist, surgeon, doctor of the highest category. Conducts both conservative and surgical treatment of urological patients, as well as diagnosis of diseases of the MVS organs. Find out more about the doctor.
Symptoms
The initial form is asymptomatic and is discovered mainly by chance during examination by a urologist.
The second stage begins to manifest itself with minor pain that goes away in a lying position, discomfort and an increase in the size of the scrotum. Increased sweating and a burning sensation in the scrotum area are increasingly observed, and problems arise during sexual intercourse.
With varicocele of the third stage, the pain is constant and does not depend on the position of the body and the physical activity performed. Significant asymmetry upon visual inspection, swollen dilated veins form a blue cluster. Poor circulation and increased temperature inside the testicle lead to changes in the structure of sperm and their motility. This leads to infertility.
Only surgical intervention is indicated, especially if the man is of childbearing age. If the disease is advanced, the processes may become irreversible, the veins can be removed, but reproductive function cannot always be restored. Only a timely visit to a urologist in St. Petersburg gives effective results.
Prevention
Any disease is easier to prevent than to treat. Simple physical exercises aimed at improving blood circulation and relieving congestion in the pelvic organs, avoiding heavy physical activity, and regular sexual relations can stop the development of the disease. Normalization of stool, avoidance of alcoholic beverages, and consumption of fortified foods or vitamin preparations prevent the appearance of varicocele.
A healthy lifestyle and good nutrition help get rid of many problems, including preventing varicocele.
Diagnostics
Modern equipment makes it possible to detect the disease even at the zero stage, when nothing is felt externally or upon palpation. Ultrasound of the scrotum and Dopplerography of blood vessels are necessary when the veins are not visually dilated and it is difficult to make a diagnosis using palpation. At the second and third stages of the disease, the doctor can make a diagnosis based on an external examination; additional examination is prescribed as necessary.
In any case, it is necessary to conduct a study of sperm quality. The spermogram is done twice, with a break of several days; before taking it, you must abstain from sexual intercourse for two to seven days.
Which methods do we prefer?
We have experience using almost all modern treatment methods. We give preference to combined treatment methods in our own modification, including ligation and sclerosis of veins. Studies and analysis of results before and after treatment have shown the advantages of these methods. With minimal trauma and operation time, high efficiency in eliminating varicose veins and improving spermogram parameters is achieved in a short time.
According to indications, we perform microsurgical dissection with ligation of veins from the inguinal approach, as well as endovascular sclerosis under angiography control.
If performed technically and in a timely manner, the operation restores the development and function of the testicle.
What methods of surgical treatment are currently used?
- Ivanisevich's operation is one of the most common treatment methods. Ligation of the branches of the spermatic vein from the inguinal approach. Efficiency 85-95%. Disadvantages - relatively low efficiency, high percentage of testicular edema after surgery from 3 to 30% and the risk of damage to the testicular artery.
- Microsurgical excision and ligation of veins - Marmar's, Goldstein's operations (modern modifications of Ivanisevich's operation) - are among the effective methods of surgical treatment of varicocele. Allows you to obtain more than 95% of positive treatment results and significantly reduce the risk of developing testicular hydrocele and lymphostasis compared to the Ivanisevich operation. Disadvantages are the long duration of the operation and the risk of damage to the testicular artery.
- Antegrade sclerotherapy from a microsurgical approach. Combined treatment method. 90-97% positive results, minimal treatment trauma among all surgical methods and higher efficiency compared to endovascular treatment.
- Palomo-Erokhin operation - ligation of the internal spermatic vein with contrasting of the lymphatic vessels of the testicle. The simplest and most effective technique, widely used in Russia until 2000. It involves staining the lymphatic vessels of the testicle to prevent their damage. In case of relapses, varicocele can reduce the risk of testicular hydrocele. Often, when performing this operation, to prevent recurrence of varicocele, the internal spermatic artery is ligated, which reduces the arterial flow to the testicle, and is one of the disadvantages of the method. Another disadvantage is the injection of a dye with a needle directly into the testicular tissue. The effectiveness is 90-95% with ligation of the testicular artery and 80-85% without ligation of the artery.
- Laparoscopic treatment of varicocele - application of clips to the internal spermatic vein during laparoscopy. A modern modification of the Palomo operation. Treatment results are similar. Efficiency 85-95%. Hydrocele 4-16%. This is the riskiest procedure due to the risk of damage to the abdominal organs. In addition, more complex and lengthy anesthesia, longer surgical intervention (along with anesthesia 30-60 minutes per procedure) with experienced specialists. All this reduces the value of the method.
- Endovascular sclerosis - angiographic introduction of sclerosing substances into the internal spermatic vein without open surgery - intravascular manipulation causing adhesion of the vein walls (endovascular occlusion, scleroplasty, endosclerosation, etc.).
The method is performed in adolescents and adults under local anesthesia and provides about 80% of positive treatment results. Sclerosing agents are delivered to the internal testicular vein through a catheter, which is placed into the venous system percutaneously (percutaneously) by puncturing the skin and the right femoral vein. Next, the catheter under fluoroscopy control is passed into the inferior vena cava and left renal vein. Failures of endovascular interventions occur in 15-20% of cases and are associated primarily with anatomical obstacles when advancing the catheter into the internal spermatic vein caused by the individual characteristics of the venous vessels. The use of occlusive emboli leads to the risk of their migration into the pulmonary arteries, although due to their small size, they do not create serious problems. - Bypass operations involve the creation of a shunt, a bypass route for the outflow of blood from the testicle, bypassing the left renal vein. The spermatic vein is sutured into the femoral, iliac or hypogastric vein. These operations are complex and not always effective due to the risk of shunt thrombosis, which occurs due to the low pressure gradient between the veins being sutured and poor blood flow.
Complementary therapy
Treating varicocele with compresses and decoctions alone is not enough. It is best to combine it with exercise, massage and wearing compression garments.
Physiotherapy
Exercises that improve pelvic circulation and make blood vessels more elastic will help. These include:
- alternate walking on toes and heels;
- bending forward;
- swing your legs;
- rotation of the pelvis.
Before performing the exercises, you should warm up. Each of them needs to be repeated 10-15 times. It is advisable to perform gymnastics 2-3 times a day.
Massage
After therapeutic exercises, it is recommended to massage the testicles. You can perform either self-massage or contact a massage therapist.
The specifics of self-massage are as follows: lying in a comfortable position, you need to rub the testicles with light circular movements, gradually increasing the pressure. Movements should be clockwise. Duration of massage for varicocele – up to 10 minutes
The procedure should not be painful. You should immediately stop manipulation if there is pain or discomfort.
Aromatherapy
A relaxing procedure with an aroma lamp has a good effect on the healing process. Suitable natural essential oils:
- mint;
- lemon balm;
- lemongrass;
- sandalwood;
- tea tree.
You can choose from this list what you like best or create your own aromatic composition. This will not reduce the therapeutic effect.
Rules for the procedure:
- light the aroma lamp and drop 5-7 drops of the selected oil into it;
- dim the lights;
- turn on relaxing music;
- relax, lying on your back.
20 minutes for such a procedure will be enough. Can be done every other day.