What is the ST segment?
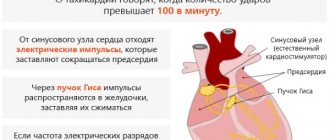
The ST segment is one of the sections of the electrocardiogram - a recording on which the electrical impulses of the heart are recorded. The work of this organ is regulated with the help of a pacemaker in the sinus node, which produces 60-90 impulses every minute.
The latter cover various areas of the heart muscle (myocardium) with excitation and are recorded on paper tape in the form of an ECG curve.
The segment of the graph, marked with the Latin letters ST, displays the part of the heart cycle when slow repolarization of the ventricles occurs, that is, their relaxation before subsequent contraction. Cardiac muscle cells cannot remain excited for a long time.
The leading role in the processes of extinction of myocardial activity is played by the coordinated work of the potassium-sodium pump, the return of sodium ions to their original state. Since electrical activity is low during this period, the ST segment should normally be in a straight line between two adjacent teeth.
Its duration (length on the graph) depends on the heart rate; the higher it is, the shorter the segment. The exact duration is difficult to measure and has little clinical significance.
Brief description of ECG elements
In the graphic image, time is recorded horizontally, and frequency and depth of changes are recorded vertically. Sharp angles displayed above (positive) and below (negative) from the horizontal line are called serrations. Each of them is an indicator of the condition of one or another part of the heart.
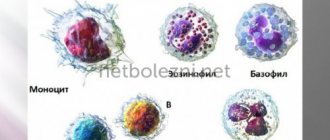
On the cardiogram, the waves are designated as P, Q, R, S, T, U.
- the T wave on the ECG reflects the recovery phase of the muscle tissue of the heart ventricles between myocardial contractions;
- wave P – indicator of depolarization (excitation) of the atria;
- teeth Q, R, S reflect the excited state of the ventricles of the heart;
- The U-wave determines the recovery cycle of distant areas of the cardiac ventricles.
The range between adjacent teeth is called a segment; there are three of them: ST, QRST, TP. The tooth and the segment together represent the interval - the time it takes for the impulse to pass. For accurate diagnosis, the difference in indicators of the electrodes (electric potential of the lead) attached to the patient’s body is analyzed. Leads are divided into the following groups:
- standard. I – difference in indicators on the left and right hand, II – ratio of potentials on the right hand and left leg, III – left hand and leg;
- reinforced. AVR – from the right hand, AVL – from the left hand, AVF – from the left leg;
- chest Six leads (V1, V2, V3, V4, V5, V6) located on the chest of the subject, between the ribs.
A qualified cardiologist deciphers the results of the study.
Having received a schematic picture of the work of the heart, the cardiologist analyzes the changes in all indicators, as well as the time for which the cardiogram records them. The main data for decoding are the regularity of muscle contractions of the heart, the number (number) of heart contractions, the width and shape of the waves reflecting the excited state of the heart (Q, R, S), the characteristics of the P wave, the parameters of the T wave and segments.
What are nonspecific ST-T changes on an ECG?
Nonspecific ST-T changes on the ECG can occur with various disorders - from infectious diseases to myocardial infarction. This ECG parameter is sensitive to the influence of many factors, that is, it cannot serve as the only diagnostic criterion for a certain pathology. Therefore, its changes are called nonspecific.
They do not have much diagnostic value, but their occurrence requires additional research, since in combination with other characteristics they can indicate serious diseases that lead to serious complications.
As mentioned above, this section should be on an isoline.
However, its deviation is allowed in the following cases:
- a decrease of 0.5 mm, especially if the T wave, reflecting the ability of the myocardium to hold the electrical potential, is characterized by a small amplitude or it is negative, that is, the phenomenon of inversion is observed (inversion relative to the isoline);
- an increase of 1.5-2 mm with a high positive T wave, while the segment has a concave shape;
- ST elevation up to 3-3.5 mm with a deep S wave and a high positive T wave. Its elevation occurs in this case gradually, that is, the segment actually turns into a T wave.
Sometimes doctors mistake these variants of the norm for deviations and make an incorrect diagnosis.
T wave indicators
Repolarization or restoration of muscle tissue after contractions, which is reflected by the T wave, has the following standards in the graphic image:
- lack of serration;
- smoothness on the rise;
- upward direction (positive value) in leads I, II, V4–V6;
- strengthening the range values from the first to the third lead to 6–8 cells along the graphic axis;
- downward (negative value) in AVR;
- duration from 0.16 to 0.24 seconds;
- predominance in height in the first lead in relation to the third, as well as in lead V6 compared to lead V1.
Deviation of the pattern from the norm indicates dysfunction of the ventricles of the heart after muscle contraction.
Heart ST depression
Depression of the ST segment, or its decrease relative to the isoline by more than 1 mm, is a clinically significant sign. Such a change can be caused by both nonspecific and specific reasons, which are discussed below.
Non-cardiac and physiological causes include:
- errors on the part of medical staff when taking an ECG - incorrect application of electrodes or their poor contact with the patient’s skin;
- water and electrolyte disturbances that occur when drinking sea water in large quantities, dehydration, alcohol abuse, salt-free diet, anorexia, heavy physical activity, use of diuretics, as well as certain pathologies (diseases of the kidneys, gastrointestinal tract, thyroid gland, burns, significant blood loss);
- drinking very cold water;
- hyperventilation (increased air exchange in the human body).
What does ECG mean in decoding?
Nonspecific ST-T changes on the ECG in the form of its decrease relative to the isoelectric line are primarily associated with cardiac ischemia, as the most dangerous condition that can lead to death.
However, this change is nonspecific and can also occur with other disorders of the heart. To correctly interpret this deviation, differential diagnosis is necessary.
Why is the ST segment reduced in adults and children?
A decrease in the ST area on the ECG in adults and children can occur in the following cases:
- Myocardial infarction with absence of ST elevation. In this case, depression of the segment is observed in two or more leads (by lead is meant the difference in biopotentials between two points of the body, for example, right hand - left hand). This type of coronary insufficiency is less common than elevation of the segment infarction (about 28% of all cases), but in recent years there has been an increase in incidence. The cause of this disorder is most often blockage of the coronary artery by a thrombus, which leads to a significant deterioration in the blood supply to the heart muscle and the development of necrosis in the tissues. The development of this condition can be triggered by stress, anemia, and infectious and inflammatory pathologies.
- Unstable angina (58% of all cases) is an intermediate condition in coronary heart disease, when the risk of developing myocardial infarction is high. The most common cause is atherosclerotic plaques in the coronary vessels of the heart, closing their lumen by ¾ or more. Risk factors are arterial hypertension, tachycardia, physical and emotional stress, consumption of heavy food and alcohol, which increases the load on the heart and causes a lack of oxygen.
- Inflammatory lesions of the heart muscleappearing against the background of infectious diseases (including influenza and respiratory pathologies).
- Toxic effects of ethanol in alcohol abuse. In this case, there is an accumulation of fatty tissue in the heart muscle and an expansion of all the cavities of the heart. At the initial stage, this disorder can be reversible, that is, giving up alcoholic beverages contributes to a significant improvement in function.
- Changes in hormonal levels during menopause in women. The main factor in menopausal cardiomyopathy is a decrease in estrogen production, which contributes to the formation of protein deficiency in the myocardium.
- Dilated cardiomyopathy , in which stretching of the cavities of the heart develops. At the same time, heart failure progresses, the rhythm and conductivity of this organ are disrupted.
- Enlargement of the right chambers of the heart due to embolism (blockage) of the pulmonary artery, severe attack of bronchial asthma, pneumonia, accumulation of air in the pleural cavity.
- Intoxication with cardiac glycosides. Heart failure does not occur immediately, but as the drug accumulates in the blood.
- Paroxysmal tachycardia , detected in elderly people.
In pregnant women, disorders associated with the ST segment are most often caused by physiological reasons - changes in the anatomical position of the heart. Therefore, if such a condition is not accompanied by complaints or a history of cardiac pathologies, then treatment is not required. In doubtful cases, the doctor may prescribe an echocardiogram.
Types of segment reduction
There are 3 types of ST depression:
- obliquely ascending, occurring against the background of tachycardia and being a variant of the norm;
- horizontal, often serving as a sign of ischemic processes in the myocardium;
- oblique, also a symptom of cardiac muscle dysfunction.
To accept the above-described phenomena as normal, the doctor must first exclude possible pathological causes.
Symptoms of deviation
Patients may experience the following symptoms as subjective symptoms:
- Myocardial ischemia:
- severe pain, feeling of pressure, heaviness behind the sternum;
- in women, pain can often radiate to the neck and arm;
- dyspnea;
- arrhythmia;
- general weakness;
- cough;
- in more rare cases - nausea, vomiting, bloating, dizziness, darkening of the eyes, cold sweat, swelling.
- Unstable angina:
- painful attacks lasting 1-10 minutes, similar in nature to the previous case;
- increased symptoms when walking, physical and emotional stress;
- signs subside when taking nitroglycerin.
- Alcoholic cardiomyopathy:
- heartache;
- dyspnea.
- Menopausal cardiomyopathy:
- pressing pain in the upper region of the heart;
- At the same time, other symptoms occur - facial redness, sweating, feeling hot;
- increased symptoms are not associated with physical activity and are not relieved by nitroglycerin.
- Intoxication with glycosides:
- nausea, vomiting, diarrhea;
- severe arrhythmia;
- tachycardia.
Differential diagnosis
Nonspecific ST-T changes require differential diagnosis taking into account medical history, additional studies and analysis of other indicators on the ECG.
To detect acute myocardial infarction, rapid determination of cardiac markers in the blood (globular protein troponin, oxygen-binding protein myoglobin, creatine kinase-MB) is used. For angina pectoris, this test shows negative results.
With alcoholic cardiomyopathy, making a diagnosis usually does not cause difficulties even after interviewing the patient. Painful attacks usually occur the day after alcohol abuse.
Pulmonary embolism is accompanied by a sharp increase in pressure in the right parts of the heart and their expansion, coronary insufficiency occurs, and on the ECG graph the electrical axis of the heart deviates to the right.
In case of an overdose of cardiac glycosides, the ECG shows a rarer heart rhythm, short electrical systole, and a trough-shaped appearance of the ST segment.
Emergency (first) aid for depression
As medical statistics show, about 70% of patients with acute myocardial infarction die in the first 6 hours.
First aid consists of the following activities:
- Call an emergency medical team.
- If the patient is conscious, give him 1 tablet of nitroglycerin under the tongue.
- Provide the patient with peace and fresh air, unfasten his clothes.
- If the patient is alone in the house, open the door to provide free access to the ambulance team, sit down and cough forcefully to induce blood flow to the heart.
Treatment of conditions accompanied by ST depression
Treatment of the most severe and dangerous condition - myocardial infarction - is carried out using the basic means indicated in the table below.
| Drug name | Dosage per day | Average price, rub. |
| Painkillers, narcotic analgesics, intravenously (dispensed strictly according to prescription) | ||
| Morphine | 3-10 mg | 120 |
| Fentanyl | 0.05-0.1 mg | 300 |
| Moradol | 1-2 mg | 250 |
| Thrombolytic agents (dissolution of blood clots) | ||
| Streptokinase | 150 million IU | 1500 |
| Urokinase | 2 million IU | 1400 |
| Anticoagulant therapy (preventing blood clots) | ||
| Heparin | 5 ml (25 thousand units) | 260 |
| Agents for limiting foci of necrosis in the heart muscle (cardioselective beta blockers) | ||
| Metoprolol | 15-50 mg | 25 |
| Atenolol | 10-50 mg | 20 |
All patients also undergo oxygen therapy - oxygen supply through a mask or catheter, which is inserted into the nasal passages. This procedure allows you to saturate the blood with oxygen and reduce the degree of ischemic damage to the myocardium.
Causes of a negative T-wave
If, with a negative T wave value, additional factors are involved in the process, this is an independent heart disease. When there are no concomitant manifestations on the ECG, a negative T display may be due to the following factors:
- pulmonary pathologies (difficulty breathing);
- disruptions in the hormonal system (hormone levels are higher or lower than normal);
- cerebrovascular accident;
- overdose of antidepressants, heart medications and drugs;
- a symptomatic complex of disorders of part of the nervous system (VSD);
- dysfunction of the heart muscle not associated with coronary disease (cardiomyopathy);
- inflammation of the heart sac (pericarditis);
- inflammatory process in the inner lining of the heart (endocarditis);
- mitral valve lesions;
- enlargement of the right side of the heart as a result of hypertension (cor pulmonale).
Objective ECG data regarding changes in the T wave can be obtained by comparing a cardiogram taken at rest and an ECG in dynamics, as well as the results of laboratory tests.
Since abnormal T-wave display may indicate CAD (ischemia), regular electrocardiography should not be neglected. Regular visits to a cardiologist and an ECG procedure will help identify pathology at the initial stage, which will significantly simplify the treatment process.
ST segment elevation
Nonspecific ST-T changes on the ECG in the form of elevation, or a higher position of the segment, in some cases are also a variant of the norm. This deviation can reach 3.5 mm in persons under 40 years of age. However, this nonspecific sign also serves as a criterion for damage to the basal sections or septum of the heart.
What does the ECG mean?
Pathological upward displacement of the ST segment above the isoelectric line is accompanied by a change in its shape:
- combination of a pronounced rise with an unrounded surface;
- horizontal flow with convexity upward;
- the excess of the amplitude of the T wave over the rise of the segment is no more than 1 mm.
Nonspecific ST-T changes on ECG
Normally, the ST is a straight horizontal or gently rising line that merges with the T, or has a convexity that faces downwards (crescent shape). In healthy people, segmental displacement with a deep S wave and a high T wave in the right precordial leads may also be observed. In doubtful cases, the patient undergoes a dynamic electrocardiographic study.
Causes in adults, children
The reasons for the higher position of this segment may be the following violations:
- Acute myocardial infarction. This is the most common pathology in which ST elevation is observed. During an attack, the segment on the ECG graph has a convex shape (“cat’s back”) and smoothly passes into the left knee of the positive T wave. Subsequently, the segment acquires a curved shape, and the T wave becomes negative, and a deep pathological Q wave appears. The rise of this section of the graph indicates about ischemic myocardial damage with complete blockage of one of the coronary arteries.
- Prinzmetal's angina. This disorder is rare in patients with chest pain - in 2-3% of cases. This deviation is based on spasm of the coronary arteries, which occurs due to an imbalance between constrictor and dilating factors (constricting and relaxing blood vessels) and the increased sensitivity of the coronary vessels to them.
- Dressler syndrome , developing in 1-3% of patients after a major myocardial infarction. The cause of this disease is autoimmune aggression and damage to the connective tissue lining of the heart.
- Early ventricular repolarization syndrome , detected in 1-9% of patients. At risk are athletes and men leading a sedentary lifestyle, people with diseases of the connective tissue and cardiovascular system. This condition can be provoked by taking alpha-adrenergic agonists, hypothermia, and lipid metabolism disorders. The severity of the disease also depends on genetic predisposition.
- Post-infarction ventricular aneurysm , when a section of the wall can gradually protrude outward during the ejection of blood into the aorta. Ultimately, part of the left ventricle expands and heart failure develops.
- Brugada syndrome , which is a genetic disorder of the heart rhythm.
Clinical manifestations
Nonspecific ST-T changes on the ECG during elevation may be accompanied by the following symptoms:
- Myocardial infarction:
- a few weeks before an acute condition - angina pectoris and rest, increased frequency of attacks;
- Otherwise, the symptoms are similar to those of a heart attack with segment depression.
- Dressler's syndrome:
- pain or discomfort in the heart;
- general malaise;
- temperature increase;
- chills;
- increased sweating;
- shallow breathing;
- red or pink skin rash;
- cough with moist wheezing.
- Early ventricular repolarization syndrome is often asymptomatic, and arrhythmia occurs in some patients.
- Prinzmetal's angina is angina that occurs regardless of external factors.
- Brugada syndrome - frequent short-term fainting.
Diagnostics
Diagnosis of acute myocardial infarction in this case is made in the same way as in the previous case. A dynamic ECG study, determination of cardiac markers, and echocardiography are performed. For Prinzmetal's angina, coronary angiography is done to study blood flow in the coronary arteries.
Dressler's syndrome is detected using laboratory blood tests (increased ESR, leukocytosis, eosinophilia, C-reactive protein), echocardiography (marked dilatation of the left ventricle, fluid in the pericardial cavity), radiography (pleural effusion). Left ventricular aneurysm is also determined using echocardiography.
Features of treatment
Features of the treatment of the above diseases are the following:
- Prinzmetal's angina – use of calcium channel blockers (Nifedipine, Diltiazem, Verapamil), long-acting nitrovasodilators (Cardiket, Monomak and others);
- Dressler's syndrome - diuretic, antiarrhythmic, antibacterial drugs, anticoagulants, cardiac glycosides, low dosage NSAIDs (Aspirin cardio, Diclofenac), glucocorticosteroids (Prednisolone);
- early ventricular repolarization syndrome - antiarrhythmic drugs (specific therapy has not been developed);
- Ventricular aneurysms – surgical treatment.
Prognosis for nonspecific ST-T changes
According to medical statistics, mortality among patients who have suffered a myocardial infarction remains high and reaches 20%. This indicator depends on the timeliness of treatment, since it is necessary to open the artery in the first 1-1.5 hours. In 44% of patients, electrocardiographic signs may be absent, which complicates diagnosis.
The following disorders may occur as complications of myocardial infarction:
- pulmonary edema;
- cardiogenic shock (sharp drop in blood pressure);
- aneurysm or heart rupture;
- inflammation of the serous membrane of the heart;
- bleeding in the gastrointestinal tract;
- mental disorders;
- development of chronic heart failure, Dressler's syndrome and post-infarction angina.
With Prinzmetal's angina, the prognosis is more favorable - mortality in the first year from the onset of the disease does not exceed 5%. In the presence of arrhythmia, hypertension, and bad habits (smoking, drinking alcohol), the risk of developing myocardial infarction and complications increases.
With a left ventricular aneurysm, the 5-year survival rate of patients is only 12%. This is associated with the progression of heart failure and arterial thrombosis.
Sudden death in patients with Brugada syndrome is one of the leading causes of nonviolent death in young adults. Sudden infant death syndrome, spontaneous ventricular fibrillation of unknown causes, and other disorders are associated with this disease.
Nonspecific ST-T changes may indicate the development of life-threatening conditions. Only one parameter taken on an ECG is not enough to make a diagnosis and prescribe treatment.
Additional diagnostics using laboratory and instrumental methods is required. In some patients, functional disorders of the heart are practically asymptomatic, so it is important to undergo preventive medical examinations on time.