Intermittent claudication is one of the most insidious conditions of the body. A person diagnosed with such a disease never knows where and how his own legs will fail. Sharp pain in the hip and the feeling that further steps are impossible are the most common symptoms among those who have encountered this problem. At the same time, it is as capable of unexpectedly letting go as it is of beginning. A number of daily habits influence the development of the problem and its transformation into a chronic form. A timely decision, namely, seeking medical help, following all the recommendations and a course of therapy, will help you forget about the disease.
What is intermittent claudication?
Intermittent claudication, also known as vascular claudication, is a symptom that describes muscle pain with mild strain (cramping, numbness, or feeling tired). The classic version is lameness that occurs during exercise such as walking and improves with a short period of rest. It is associated with early stage peripheral artery disease and can progress to critical limb ischemia unless treatment or risk factors are changed.
Content:
- What is intermittent claudication?
- Symptoms and causes of intermittent claudication
- Diagnosis of intermittent claudication
- Pharmacological treatment options
Intermittent claudication is a painful, severe, debilitating and sometimes burning pain in the legs that comes and goes - usually occurring when walking due to poor circulation in the arteries of the legs. With very advanced lameness, pain is felt even at rest. Intermittent lameness can occur in one or both legs and often progresses over time. However, some people only complain of weakness in their legs when walking and a feeling of "tiredness" in their buttocks. Impotence is a very rare complaint in men caused by lameness.
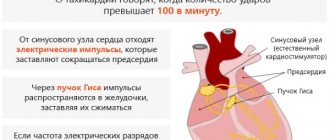
Typically, the variable nature of the lameness is associated with a narrowing of the arteries that fill the leg with blood, a limited supply of oxygen to the leg muscles, which is felt as the need for oxygen in these muscles increases (during exercise). Intermittent claudication can be caused by short-term narrowing of an artery due to spasm, narrowing due to atherosclerosis, or occlusion (closing). This condition is quite common.
Signs
For a long time, a dangerous disease does not manifest itself, the processes proceed slowly, which leads to an advanced stage. Therefore, read the peculiar symptoms very carefully and do not treat them with disdain.
- Painful sensations at first only when climbing (uphill or stairs), and then during normal walking.
- Dry and flaky skin, discoloration.
- Hair loss.
- Non-healing wounds form.
The pain can be burning or throbbing, sharp or aching, concentrated in the fingers, calves, and thighs. The feeling of discomfort causes a person to limp and make frequent stops while walking.
If you experience such conditions, be sure to contact our doctors. Only timely intervention by a specialist can prevent serious consequences.
Symptoms and causes of intermittent claudication
One of the hallmarks of arterial claudication is that it occurs intermittently: it disappears after a very short rest, and the patient can begin to walk again until the pain recurs. The following signs are common for atherosclerosis of the arteries of the lower extremities:
- cyanosis;
- atrophic changes such as hair loss, shiny skin;
- low temperature;
- decreased impulse;
- redness as the limb returns to a "dependent" lameness position;
- paresthesia;
- paralysis.
Causes and factors influencing intermittent claudication may include: vascular disease, smoking, hypertension and diabetes. Most often, intermittent claudication (vascular or arterial) is caused by peripheral arterial disease, which implies significant atherosclerotic blockages leading to arterial insufficiency. It is distinct from neurogenic claudication associated with lumbar spinal stenosis. The disease is also directly provoked by smoking, hypertension and diabetes.
There are several other factors that cause lameness. The most important thing is the habit of smoking and irregular exercise (or their complete absence). If you are a smoker, you must make a determined effort to completely quit your negative lifestyle. Tobacco is especially harmful to those suffering from lameness because smoking accelerates the clogging of the arteries. The best way to quit is to choose a day when you're going to stop completely, rather than trying to taper your dose gradually. If you are having problems, contact your doctor who can provide advice and further help. Excess weight is the main cause of vascular problems and, as a result, lameness. The more weight your legs have to carry, the more blood the muscles themselves need. If necessary, your doctor or nutritionist will create a personalized weight loss diet.
Discussion
Thus, the results of the study demonstrated the existence of various clinical forms of NPH in patients with PDS. Noteworthy is the relatively high incidence of painless forms of NPH among the observed patients (7.2%), despite the fact that pain is a key manifestation of the disease, and there are practically no descriptions of the painless form of NPH in the literature. Silent NPH can cause difficulties in diagnosing PDS and NPH and require differential diagnostic measures. We did not find a connection between clinical manifestations and the nature of changes in MRI studies and the type of NPH, while the form of clinical manifestations of NPH did not affect the outcome of surgical treatment. We noted a symptom of pacing, manifested by a relatively short period of increase in the clinical manifestations of NPH during walking, followed by their complete regression, despite non-stop walking. A typical manifestation of NPH is an increase in radicular symptoms and pain when walking, while the phenomenon of pacing is noted much less frequently and is not discussed in the literature. The possibility of the existence of such an atypical symptom, which may be the reason for the incorrect identification of the nature of NPH, seems important. It should also be noted that the presence of this phenomenon in the observed patients did not affect the outcome of the disease.
The data presented indicate a variety of (often atypical) clinical manifestations of PDS, which requires both a thorough analysis of the clinical picture of the disease and an imaging examination to clarify the cause of NPH and select the optimal treatment tactics.
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Diagnosis of intermittent claudication
Intermittent claudication is a symptom and by definition is diagnosed by the patient reporting a history of leg pain associated with walking. However, because other conditions (sciatica) can mimic intermittent claudication, testing is often performed to confirm the diagnosis of peripheral artery disease.
Magnetic resonance angiography and duplex ultrasonography appear to be slightly more cost-effective in diagnosing peripheral arterial disease among people with intermittent claudication than projection angiography. Exercise may improve symptoms, and revascularization may also help. Both methods together are much more effective than one intervention. Diagnostic tests include:
- measuring blood pressure to compare it in the arms and legs;
- Doppler ultrasound examination of the legs;
- duplex Doppler or ultrasound examination of the extremities to visualize arterial blood flow;
- ECG and arteriography (an injectable dye that can be visualized in the arteries).
The prognosis is usually good because the condition can improve over time. Doctors also recommend conservative therapy. A program of walking daily for short periods and stopping pain or cramping will often help improve functional leg function by encouraging the development of collateral circulation, that is, the growth of new small blood vessels that bypass the area of obstruction in the artery.
You should stop smoking, avoid applying heat or cold to your feet, and avoid wearing shoes that are too tight. If conservative therapy is unable to correct the situation, after diagnosis, doctors suggest correction of the affected artery. This option depends on the location and degree of narrowing of the artery, as well as the patient's underlying condition.
Testing for lameness may include:
- Ultrasound is most often used to determine the location and degree of narrowing in blood vessels;
- ankle index measures blood pressure compared to blood pressure in the arm (an abnormal result is a sign of peripheral artery disease);
- segmental blood pressure measures it in different parts of the leg to detect blockages that are causing decreased blood flow;
- Computed tomography (CT) and magnetic resonance angiography (MRA) are other non-invasive tests that can help the doctor map blood flow to affected areas (these are considered if the doctor thinks a procedure (revascularization) to treat peripheral artery disease might be helpful) .
Treatment
First aid
In case of traumatic injuries, they provide rest, temporarily fix the limb with a splint or soft bandage, give painkillers, and apply cold. In other conditions, limit the load on the leg, select comfortable shoes, and use a cane or crutches if necessary.
Conservative therapy
For lameness, the following treatment measures can be taken:
- Protective mode
. The patient may be placed in a plaster cast, advised to remain quiet, refrain from walking long distances, and use additional devices to unload the limb (crutches, cane, walker). - Orthopedic structures
. The goal is to support the affected segment, reduce or redistribute the load, and equalize the length of the legs. Splints, insoles, and orthopedic shoes are used. - Drug therapy
. Analgesics, antibiotics, NSAIDs, vitamin complexes, drugs to improve blood circulation, and drugs to restore nerve conduction are prescribed. - Physiotherapy
. To reduce inflammation and pain, stimulate recovery processes, the patient may be recommended UHF, ultrasound, laser therapy, magnetic therapy, medicinal electrophoresis, shock wave therapy, and other techniques. - Exercise therapy
. It is an important part of the treatment of many diseases accompanied by lameness. May include exercises to increase muscle strength and joint mobility, improve coordination of movements, and correct motor stereotypes. - Other methods
. Massage and manual therapy are widely used. In recent years, taping has become increasingly common.
Surgery
Taking into account the characteristics of the pathology for lameness, the following operations are performed:
- Traumatic injuries
: suturing wounds, opening hematomas, open removal of menisci, arthroscopic meniscectomy, osteosynthesis of an impacted femoral neck fracture. - Infectious processes
: opening, drainage of abscesses, arthrotomy for purulent arthritis. - Congenital and acquired deformities
: elimination of curvature, lengthening of the tibia or femur using the Ilizarov apparatus, various types of bone grafting. - Oncological diseases
: tumor removal, bone resection, amputation and disarticulation. - Vein diseases
: phlebectomy, miniphlebectomy, RFO and laser coagulation of varicose veins, thrombectomy, crossectomy, installation of a vena cava filter, venous bypass surgery, etc. - Arterial pathologies
: sympathectomy, thromboembolectomy, endarterectomy, stenting, bypass and other reconstructive interventions. - Neurological diseases
: removal of spinal cord tumors, elimination of spinal stenosis, stabilizing interventions on the spine.
To improve joint function and increase the supportability of the limb in case of articular lesions of various origins, arthroplasty, arthrodesis, and endoprosthetics are used.