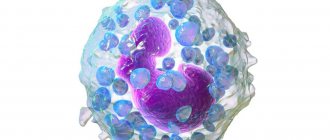
Eosinophils are cells contained in the blood that perform a protective function and are an integral part of the leukocyte formula. To determine their quantity, a general blood test (from a finger or vein) is used.
The main task of eosinophils is to penetrate into the site of inflammation and activate cellular receptors in it that are responsible for antiparasitic immunity. In other words, blood eosinophils provoke the cells around the parasite to self-destruct, thereby enclosing the parasite in a capsule of their membranes. Such a capsule becomes a beacon for other, more aggressive cells and substances of the immune system, and shows them where the parasite is located.
Eosinophils also accumulate and release substances (called inflammatory mediators) such as histamine, phospholipase, and others involved in general immune reactions (eg, anaphylactic shock). In addition, eosinophils are able to absorb and destroy small microbial bodies.
In pregnant women
Normally, eosinophils in the blood are reduced in pregnant women - this is a physiological state of quantity.
With the onset of labor and during labor, the number of eosinophils during pregnancy decreases. After 14 days it returns to normal. When taking a blood test for eosinophils, one should take into account the physiological conditions in which eosinopenia may occur, mentioned above. The body compensates for the physiological decrease in eosinophils in pregnant women and the number of blood cells quickly returns to normal.
Treatment or some kind of intervention from specialists is required only in case of a pathological decrease in the number of these blood cells.
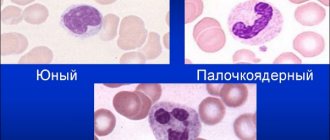
Place among blood cells
Leukocytes are the body's natural protectors. Their structure and ability to absorb different dyes during microscopy allowed researchers to divide cells into groups, and the functions of each of these groups may be special. Granular leukocytes include neutrophils, eosinophils, and basophils; They are united by segmentation of the nucleus and granules in the cytoplasm. Lymphocytes and monocytes are considered nongranular. All white blood cells try to be the first to meet any invader, so the body intensively replenishes their number during infections, allergies or parasite invasions. Eosinophils are no exception.
In childhood
In children, the absolute number of eosinophils in the blood is 0.05-0.7X109/l; by the age of 11, the number of cells becomes 0-0.6X109/l. The leukocyte formula takes into account only the percentage of eosinophils. It is these numbers that have diagnostic value.
Eosinophils may be low in the blood of a child for the same reasons as in an adult. But let us remind you once again that you need to look not at absolute values, but at relative ones. Because normally, indicators may differ for children of different ages.
FAQ
h25,0,0,0,0—>
Question: Is it possible to get rid of eosinopenia with herbs? If yes, which ones?
p, blockquote21,0,0,0,0—>
Answer: It is not the deviation in the UAC itself that needs to be treated, but its causes. It is not a fact that the problem is caused by a depressed state of immunity. It is better not to self-medicate. There is a risk of missing a dangerous disease and even worsening its course. If a person knows for sure that disorders are caused by stressful situations or a lack of nutrients in the diet, high loads, it makes sense to resort to general strengthening measures. A balanced diet, moderate physical activity, hardening, and frequent walking help normalize the functioning of the defenses. When you really want to resort to herbal medicine, you can use herbs with adaptogenic properties. These include Echinacea purpurea, Rhodiola rosea, Eleutherococcus and ginseng. Their extracts can be purchased at the pharmacy in ready-made form.
p, blockquote22,0,0,0,0—>
- Why are eosinophils in the blood low, what does this mean?
Question: How to prepare for the analysis in order to exclude a false positive result? I’m taking the UAC test for the 3rd time, the previous 2 times the doctor doubted that the result was correct.
p, blockquote23,0,0,0,0—>
Answer: 3 days before the test, you need to stop taking medications and expose yourself to significant physical activity. It is advisable to give up fatty foods and moderate the amount of protein foods in the diet. It is worth excluding alcoholic beverages and various “harmful” foods (fast food, processed foods, chips, crackers). The last meal should take place 8–12 hours before the collection of biomaterial. It is forbidden to consume any food or drinks other than pure water (you will also have to skip morning coffee). It is better not to smoke directly on the day of the test. It is worth limiting yourself from stress, overheating or freezing on the way to a medical facility.
p, blockquote24,0,0,1,0—>
Question: Is it possible to take the OAC during menstruation? How can they affect performance?
p, blockquote25,0,0,0,0—>
Answer: It is not worth taking a test during menstruation unless absolutely necessary. During this period, any of the indicators may go beyond the normal range, which is not associated with the disease. Doctors recommend refraining from any laboratory tests 3 days before, immediately during bleeding, and 2-3 days after. However, regarding eosinophils, there is another version. It is believed that the importance of these blood cells may reduce progesterone. If it is eosinophils that cause doubts, it is worth getting tested after menstruation, but before ovulation (7-13 days of the cycle).
p, blockquote26,0,0,0,0—>
Question: Is it possible to reduce the level of eosinophils with drugs used for allergies to critical levels?
- Why are eosinophils elevated in the blood, what does this mean?
p, blockquote27,0,0,0,0—>
Answer: Antihistamines have little effect on the blood picture if they are used correctly and the recommended doses are followed. It is important to observe the duration of the course, take breaks or change medications on time. Significant deviations in the blood picture can be caused by hormonal drugs, so you need to be careful with them and use them only as prescribed by a doctor.
p, blockquote28,0,0,0,0—>
Question: Will herbal remedies from the group of immunostimulants (for example, Immunal or Immupret) help increase the level of eosinophils?
p, blockquote29,0,0,0,0—>
Answer: They will help if the deviation is caused by an infectious disease, exhaustion of the body, or stress. If the nature of the disorders is purulent processes, malignant or hereditary pathologies, immune stimulants will not help, and in diseases of the bone marrow or endocrine glands they can even cause harm.
p, blockquote30,0,0,0,0—>
Correction
Conservative therapy
Patient management tactics depend on the etiology of eosinopenia and the severity of the patient’s condition. Eosinopenia in itself does not have a negative effect on the body. Therefore, if it develops during the use of GCS, their withdrawal is not required. For neurotic disorders, it is necessary to consult a psychotherapist who conducts psychotherapy sessions and prescribes pharmacological drugs (antidepressants, tranquilizers).
People with allergies are advised to avoid contact with the allergen. If COVID-19 is confirmed, in order to prevent the spread of coronavirus infection, patients are moved to an infectious disease isolation ward. In severe bilateral pneumonia with respiratory failure (saturation below 90%), connection to a ventilator is indicated.
The following medications are used to treat conditions that can cause eosinopenia:
- Antihistamines.
To relieve allergy symptoms, drugs are used that block histamine receptors, the main mediator of allergic reactions. - Bronchodilators.
To relieve an attack of bronchial asthma, inhalers containing beta-2-adrenergic receptor agonists and cholinergic receptor blockers are prescribed. - Inhaled glucocorticoids.
As a basic therapy that suppresses the inflammatory process in the bronchi, GCS in the form of inhalations are very effective. - Anthelmintic drugs.
These drugs disrupt the function of the neuromuscular system of helminths, thereby causing their paralysis and death. - Antibiotics.
For purulent processes, broad-spectrum antibacterial drugs are prescribed - cephalosporins, penicillins. - Steroidogenesis blockers.
Inhibitors of cortisol synthesis or glucocorticoid receptor blockers are used in preparation for surgical treatment of Cushing's disease or syndrome to reduce the concentration of cortisol in the blood. - Immunobiological drugs.
To reduce the severity of the cytokine storm in patients with COVID-19, monoclonal antibodies, Janus kinase inhibitors, and intravenous administration of human immunoglobulin are used.
It is worth paying attention to the fact that none of the many antiviral drugs recommended by many experts has demonstrated a positive effect in the treatment of a new coronavirus infection. Also ineffective were drugs prescribed to suppress the inflammatory process in the lungs - synthetic antimalarials and macrolide antibiotics.
Surgery
Patients with Itsenko-Cushing's disease are indicated for neurosurgical surgery - transsphenoidal adenomectomy. For Itsenko-Cushing syndrome, laparoscopic bilateral adrenalectomy is performed, followed by hormonal replacement therapy with glucocorticoids and mineralocorticoids. An hydatid cyst, which is most often localized in the liver, also needs to be surgically removed.
Decrease in eosinophils during exacerbations
Eosinophil counts are reduced to almost 0 in adults with acute appendicitis. With appendicitis, NEUT is sharply increased to 18 * 109/l, and the percentage of EO can decrease to 0.
The number of eosinophils may remain unchanged. The proportion of lymphocytes also decreases with appendicitis.
- Neutrophils are reduced in an adult. Causes of lymphocytes increased, decreased in the analysis
Lymphocytes and eosinophilic granulocytes are predominantly involved in allergic reactions. And their relative decrease with a simultaneous increase in neutrophils indicates a severe bacterial purulent infection, for the elimination of which neutrophils are mainly responsible.
Eosinophils are reduced to 0 in adults with severe inflammatory diseases of the lungs and bronchi, and when blood test values begin to increase, this means that the person is recovering.
Features of eosinopenia in women
During pregnancy, the content of eosinophilic leukocytes is normally reduced, which suggests that such a change is necessary to ensure normal fetal development. The immune system partially blocks the production of granulocytes, since their normal and high activity increases the risk of fetal rejection.
Eosinophils are sharply reduced during childbirth. During childbirth, a woman experiences extreme stress and prolonged pain. Low eosinophils during pregnancy due to the pain shock that a woman experiences during childbirth are reduced to almost 0.
Absolute eosinopenia is observed in women giving birth in 99% of cases. The analysis returns to normal about two weeks after the birth of the child.
The above does not mean that there is no immunity during pregnancy. In pregnant women, other ways of protecting the body are activated. The activity of macrophages and NK cells increases.
Eosinophils decrease under the influence of taking hormonal contraceptives, as well as under the influence of products containing iron, which are prescribed to women for the treatment of iron deficiency anemia. The condition of iron deficiency anemia, which can occur in a latent form, develops in women with heavy periods and frequent childbirth.
Treatment with glucocorticosteroids
When treated with hormonal drugs, the formation of eosinophils in the bone marrow is inhibited, as evidenced by a decrease in their content in the analysis to 0. Such indicators can be caused by taking corticosteroids within 2 to 6 hours after use.
Reduced EO in pathologies of the adrenal glands. Increased secretion of hormones, especially cortisol, one of the hormones of the adrenal cortex, can reduce the number of eosinophils.
Impact of stress
A decrease in the number of eosinophils in adults is observed with sleep disturbances. In people suffering from insomnia, immune defenses gradually weaken and cortisol levels increase.
Elevated cortisol levels cause:
- changes in the leukocyte formula - decreased EO, lymphocytes;
- increased NEUT, red blood cells, platelets;
- immune depression - blocks the production of cytokines, interferon gamma, immunoglobulins.
With prolonged lack of sleep caused by nervous or physical stress, both absolute and relative indicators of eosinophilic leukocytes can drop to almost 0.
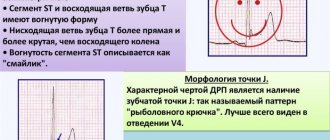
Analysis transcript
Decreased relative eosinophils and increased monocytes in the blood after an infectious disease in both adults and children serve as an indicator of recovery. When the absolute content of eosinophils approaches 0, this indicates inhibition of granulocyte hematopoiesis in the bone marrow.
The proportion of eosinophilic leukocytes in an adult may decrease to 0% during severe bacterial infections. The absolute content of EO may be within normal limits.
Such a change in the leukocyte formula indicates a sharp increase in neutrophils, due to which the proportion of eosinophils is reduced to almost 0%. In adults, similar disorders are observed with acute respiratory infections, inflammatory purulent infectious diseases of the ENT organs, and diseases of the reproductive system.
In women, the percentage of EO is reduced with increased neutrophils in the case of:
- ovarian cysts;
- inflammation of the fallopian tubes;
- endometritis;
- vaginitis;
- cervical canal infections.
In men, decreased relative eosinophils and increased NEUT are observed with prostatitis, sexually transmitted diseases, testicular hydrocele, and prostate adenoma.
A decrease in eosinophils in the blood indicates that an adult or child has reduced immunity, and this means that, in addition to treatment, you need to think about what to feed the patient. A rational diet with sufficient amounts of protein, vitamins, micro- and macroelements is a reliable prevention of eosinopenia and a decrease in the body’s immune reactivity.
Diagnostics
Eosinopenia has a fairly wide range of etiological factors, so if it is detected, you should consult a general practitioner. When collecting anamnesis, it is necessary to clarify whether the patient is taking medications and whether he is registered at a dispensary for a chronic disease. It is also necessary to find out whether the patient has traveled abroad over the past few months, or eaten insufficiently processed meat or fish, unwashed vegetables or fruits.
Much attention is paid to examining the patient. Thus, skin rashes in the form of urticaria indicate the presence of allergies, centripital obesity, stretch marks on the lateral surfaces of the abdomen are characteristic of hypercortisolism. If COVID-19 is suspected, body temperature and saturation are measured, and lung auscultation is performed. It is clarified whether there is a dry cough, difficulty breathing, loss of smell and taste. Additional research methods are prescribed, including:
- General blood analysis.
Patients with coronavirus infection often experience lymphopenia; with purulent infections, general leukocytosis and an increase in ESR are detected; helminthic infestations are characterized by a decrease in hemoglobin levels. - Blood chemistry.
With helminthiasis, a deficiency of iron and ferritin is detected; for patients with hypercortisolism, a high concentration of glucose is typical. - Parasitological studies.
Using various processing methods (sedimentation, enrichment), microscopic examination of feces for helminth eggs is carried out. - Allergological research.
The allergic nature of the disease is confirmed by the high content of immunoglobulin E. The presence of hypersensitivity to certain types of allergens is determined by skin tests, prick tests, and the detection of specific immunoglobulins in the blood. - Hormonal studies.
There are 3 tests for diagnosing hypercortisolism - determination of cortisol in saliva, in daily urine, and also in blood serum after taking tableted dexamethasone (small dexamethasone test). To differentiate the syndrome from Cushing's disease, a large dexamethasone test is performed. - Pathogen identification.
If COVID-19 is suspected, immunoglobulin M is determined in the blood using ELISA or the express method (immunochromatography). An accurate diagnosis can be determined by the presence of viral RNA by PCR of materials from the pharynx and nasopharynx. - CT, MRI.
In patients with Cushing's syndrome, an abdominal CT scan reveals an adrenal tumor. In Itsenko-Cushing's disease, a pituitary adenoma is found on MRI of the brain.
Eosinophil count