- home
- Articles about cholelithiasis
- This is useful to know
- About the structure of the human body
- Catalog of useful medical articles
›
›
›
›
There are two types of valves in the human heart.
These are leaflet and semilunar valves. In this article we will understand which valves are called leaflet and why, and which are semilunar. In addition, we will take a close look at the structure and operation of the semilunar valves. Sections of the article
Leaf and semilunar valves
Structure and operation of semilunar valves
Left semilunar valve
Right semilunar valve
The problem of the semilunar valves
Leaf and semilunar valves of the heart
There are two types of valves: leaflet and semilunar.
The leaflet valves are located between the atrium and the ventricle. Valve leaflets are composed of endothelium. A chorda tendineum extends from each leaflet into the ventricle. The chorda tendineum attaches to the papillary muscles of the myocardium (muscle trabecula).
There are two flap valves:
tricuspid valve (TC), or tricuspid - has 3 leaflets and is located between the right atrium and the right ventricle (in the right atrioventricular orifice)
mitral valve (MK), or bicuspid - has 2 leaflets and is located between the left atrium and the left ventricle (in the left atrioventricular orifice)
The valves prevent blood from flowing back from the ventricles into the atria.
Regurgitation is the reverse flow of blood from the ventricles into the atria.
Semilunar valves
Semilunar valves consist of three valves that look like pockets. When the ventricles contract, the valves bend inside the arteries (AO and pulmonary trunk).
There are two semilunar valves:
aortic valve (AK) - located at the entrance to the Ao, between the left ventricle and the Ao
pulmonary valve (VV) - located at the entrance to the pulmonary trunk, between the right ventricle and the pulmonary trunk
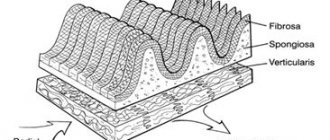
Structure of the heart wall
The wall of the heart consists of 3 layers, each layer has its own name.
The endocardium is the inner layer of the heart. It consists of endothelium.
Myocardium is the middle layer. It consists of cardiac striated muscle tissue. It consists of cardiomyocytes connected by intercalated discs, due to which 2 atria and 2 ventricles contract simultaneously. The myocardium consists of 2 layers (atria) and 3 layers (ventricles).
The myocardium of the atria is thinner than that of the ventricles. The myocardium of the left ventricle is thicker than the right (since the BCC begins there).
The pericardial sac is the outer layer. It consists of 2 layers:
The epicardium - the inner layer of the bag - consists of squamous epithelium and fuses with the myocardium.
The pericardium, the outer layer of the bursa, consists of a single layer of squamous epithelium and connective tissue. Outside, the pericardium fuses with the tendon center of the diaphragm and the sternum.
Between the epicardium and the pericardium there is a small space - the pericardial cavity, filled with serous fluid. Its function is to prevent friction between the two layers of the pericardial sac.
The leaflet valves are located between the atrium and the ventricle. Valve leaflets are composed of endothelium. A chorda tendineum extends from each leaflet into the ventricle. The chorda tendineum attaches to the papillary muscles of the myocardium (muscle trabecula).
There are two flap valves:
tricuspid valve (TC), or tricuspid - has 3 leaflets and is located between the right atrium and the right ventricle (in the right atrioventricular orifice)
mitral valve (MK), or bicuspid - has 2 leaflets and is located between the left atrium and the left ventricle (in the left atrioventricular orifice)
The valves prevent blood from flowing back from the ventricles into the atria.
Regurgitation is the reverse flow of blood from the ventricles into the atria.
Semilunar valves
Semilunar valves consist of three valves that look like pockets.
When the ventricles contract, the valves bend inside the arteries (AO and pulmonary trunk).
There are two semilunar valves:
aortic valve (AK) - located at the entrance to the Ao, between the left ventricle and the Ao
pulmonary valve (VV) - located at the entrance to the pulmonary trunk, between the right ventricle and the pulmonary trunk
Structure of the heart wall
The wall of the heart consists of 3 layers, each layer has its own name.
The endocardium is the inner layer of the heart.
It consists of endothelium.
Myocardium is the middle layer.
It consists of cardiac striated muscle tissue. It consists of cardiomyocytes connected by intercalated discs, due to which 2 atria and 2 ventricles contract simultaneously.
General understanding of anatomical structures
The valve apparatus consists of many structures that prevent the retrograde movement of blood.
It also contains semilunar valves or flaps. Outwardly, they resemble pockets located on the inner walls of blood vessels. The semilunar valves are located at the exit of the pulmonary artery, as well as the aorta from the ventricles. As soon as blood is ejected into the pulmonary artery, aorta, these structures are pressed against the walls of the vessels.
The blood that has flowed into the pockets fills them, and they close tightly. Therefore, when the ventricles relax, blood does not return to the heart. In this way, the movement of matter is maintained strictly in one direction.
The pockets in question do not have chordae tendineae. Moreover, such connections are more reminiscent of vein pockets than atrioventricular valves.
The semilunar valves of the veins are closed
The myocardium consists of 2 layers (atria) and 3 layers (ventricles).
The myocardium of the atria is thinner than that of the ventricles. The myocardium of the left ventricle is thicker than the right (since the BCC begins there).
The pericardial sac is the outer layer. It consists of 2 layers:
The epicardium - the inner layer of the bag - consists of squamous epithelium and fuses with the myocardium.
The pericardium, the outer layer of the bursa, consists of a single layer of squamous epithelium and connective tissue.
Outside, the pericardium fuses with the tendon center of the diaphragm and the sternum.
Between the epicardium and the pericardium there is a small space - the pericardial cavity, filled with serous fluid. Its function is to prevent friction between the two layers of the pericardial sac.
Valves are:
casement
semilunar
The leaflet valves are located between the atrium and the ventricle. Valve leaflets are composed of endothelium. A chorda tendineum extends from each leaflet into the ventricle. The chorda tendineum attaches to the papillary muscles of the myocardium (muscle trabecula).
There are two flap valves:
tricuspid valve (TC), or tricuspid - has 3 leaflets and is located between the right atrium and the right ventricle (in the right atrioventricular orifice)
mitral valve (MK), or bicuspid - has 2 leaflets and is located between the left atrium and the left ventricle (in the left atrioventricular orifice)
The valves prevent blood from flowing back from the ventricles into the atria.
Regurgitation is the reverse flow of blood from the ventricles into the atria.
Semilunar valves
Semilunar valves consist of three valves that look like pockets.
When the ventricles contract, the valves bend inside the arteries (AO and pulmonary trunk).
There are two semilunar valves:
aortic valve (AK) - located at the entrance to the Ao, between the left ventricle and the Ao
pulmonary valve (VV) - located at the entrance to the pulmonary trunk, between the right ventricle and the pulmonary trunk
Structure of the heart wall
The wall of the heart consists of 3 layers, each layer has its own name.
The endocardium is the inner layer of the heart.
It consists of endothelium.
Myocardium is the middle layer. It consists of cardiac striated muscle tissue. It consists of cardiomyocytes connected by intercalated discs, due to which 2 atria and 2 ventricles contract simultaneously.
The myocardium consists of 2 layers (atria) and 3 layers (ventricles).
The myocardium of the atria is thinner than that of the ventricles.
Vessel valves
Semilunar valves in blood vessels perform the same role as in the heart. They interfere with retrograde blood flow. Located in vessels that are not endowed with a well-developed muscular layer, these are lymphatic vessels and veins.
Most of these valves are found in the veins of the lower extremities. For example, the great saphenous vein of the leg contains more than 8 valves. Why? Because the veins are not endowed with a muscular membrane, blood under the influence of gravity will stagnate in the lower extremities. Semilunar valves prevent blood stagnation in the lower extremities, and not only in them.
The leaflet valves in the human heart are located
The myocardium of the left ventricle is thicker than the right (since the BCC begins there).
The pericardial sac is the outer layer. It consists of 2 layers:
The epicardium - the inner layer of the bag - consists of squamous epithelium and fuses with the myocardium.
The pericardium, the outer layer of the bursa, consists of a single layer of squamous epithelium and connective tissue.
Outside, the pericardium fuses with the tendon center of the diaphragm and the sternum.
Between the epicardium and the pericardium there is a small space - the pericardial cavity, filled with serous fluid. Its function is to prevent friction between the two layers of the pericardial sac.
Valves are:
casement
semilunar
The leaflet valves are located between the atrium and the ventricle. Valve leaflets are composed of endothelium. A chorda tendineum extends from each leaflet into the ventricle. The chorda tendineum attaches to the papillary muscles of the myocardium (muscle trabecula).
There are two flap valves:
tricuspid valve (TC), or tricuspid - has 3 leaflets and is located between the right atrium and the right ventricle (in the right atrioventricular orifice)
mitral valve (MK), or bicuspid - has 2 leaflets and is located between the left atrium and the left ventricle (in the left atrioventricular orifice)
The valves prevent blood from flowing back from the ventricles into the atria.
Regurgitation is the reverse flow of blood from the ventricles into the atria.
Semilunar valves
Semilunar valves consist of three valves that look like pockets.
When the ventricles contract, the valves bend inside the arteries (AO and pulmonary trunk).
There are two semilunar valves:
aortic valve (AK) - located at the entrance to the Ao, between the left ventricle and the Ao
pulmonary valve (VV) - located at the entrance to the pulmonary trunk, between the right ventricle and the pulmonary trunk
Structure of the heart wall
The wall of the heart consists of 3 layers, each layer has its own name.
The endocardium is the inner layer of the heart.
It consists of endothelium.
Myocardium is the middle layer. It consists of cardiac striated muscle tissue. It consists of cardiomyocytes connected by intercalated discs, due to which 2 atria and 2 ventricles contract simultaneously. The myocardium consists of 2 layers (atria) and 3 layers (ventricles).
The myocardium of the atria is thinner than that of the ventricles. The myocardium of the left ventricle is thicker than the right (since the BCC begins there).
The pericardial sac is the outer layer.
It consists of 2 layers:
The epicardium - the inner layer of the bag - consists of squamous epithelium and fuses with the myocardium.
The pericardium, the outer layer of the bursa, consists of a single layer of squamous epithelium and connective tissue.
Structure of heart structures
The semilunar valve got its name as a result of the fact that the flap that enters it has a similar shape. Typically, these structures include the aortic valve and the semilunar recess of the pulmonary trunk. Each of them has certain valves (the type and size vary depending on the age category or individual characteristics of the body).
Components of the aortic valve:
- rear flap;
- right flap;
- left flap.
The only difference is that the pulmonary valve contains an anterior valve, not a posterior one. The pockets in question are located near the fibrous ring. As a rule, they are formed by duplication of the endocardium.
Quite often there is a cardiac anomaly when a person’s aortic pouch consists of only two valves.
Normal performance
To study the functioning of the CPA at the primary stage, a general clinical examination of the patient is used. Characteristic signs of violations:
- dyspnea;
- pulsation of the neck veins;
- pallor or cyanosis of the upper part of the body;
- during auscultation – additional noise at the point of valve projection.
Making a final diagnosis and choosing adequate treatment tactics depends on the results of instrumental methods that objectively assess the condition of this structure. The most common tests are electrocardiography (ECG) and echocardiography (echoCG).
ECG
There are no specific electrocardiographic signs of PC defects. Changes in the ECG occur when symptoms of heart failure due to a valve defect appear.
With regurgitation or stenosis of the pulmonary valve, hypertrophy of the right ventricle develops, which is established on the ECG in comparison with the state of the left sections.
Severe pancreatic hypertrophy (mass larger than left):
- the ventricular QRS complex is represented by qR or simply R in precordial lead V1;
- in V6 the QRS complex is deformed in rS, RS (occasionally – Rs);
- the degree of hypertrophy is reflected by the height of the R wave in V1 and the depth of S in V6 - the greater the difference between them, the more significant the increase in the myocardium;
- the ST segment in V1 is under the isoline, the T wave is negative;
- in V6 ST is located above the isoline, T-positive.
Moderate hypertrophy (the mass of the pancreas is less than the left one, but impulse conduction is slow):
- The QRS complex in V1 is observed as rsR or rSR;
- V6 deformation in qRS.
Moderate hypertrophy is represented by deformation of the QRS complex:
- in V1 – rS, RS, Rs;
- in V6 – qR;
- the amplitude of the R wave in V1 is increased;
- the S waves in V1 and R waves in V6 are reduced.
A shift of the electrical axis of the heart to the right is noted at each stage of hypertrophy.
ECHO
Ultrasound examination of the heart is considered the gold standard for diagnosing PC defects. The method allows you to study the anatomical features and functional state of the valves. To visualize internal hemodynamics, Doppler echocardiography is used.
The pulmonary valve on ECHO is depicted in the form of a three-lamellar formation, the elements of which bend into the lumen of the vessel during RV systole.
Standard PC indicators:
- structure – normoechoic, homogeneous;
- peak blood flow velocity – 0.5-1.0 m/s;
- average pressure gradient – up to 9 mm Hg. Art.;
- lumen diameter – 11-22 mm.
During ultrasound, the structure of the coronary artery and the presence of pathological formations are studied. The main changes for various defects are presented in the table.
| PA stenosis | Insufficiency (regurgitation) of the coronary arteries |
|
|
Diagnostic examination methods
If any signs indicating problems with the heart appear, an examination by a cardiologist is immediately required. In addition to collecting anamnesis, the doctor prescribes the necessary types of hardware diagnostics.
The very first method that will reveal the presence of congenital heart disease in the form of a bicuspid aortic valve is echocardiography (a type of ultrasound (you can watch it on video), which allows you to identify not only the presence of an anomaly, but also the degree of regurgitation).
In addition, diagnostics may include:
- radiography;
- electrocardiogram;
- Doppler study;
- cardiac catheterization.
Signs of a cardiac abnormality
Very often, the defect - bicuspid aortic valve in children - occurs without symptoms, it is not suspected for decades, but the older a person gets, they more often show signs of an anomaly.
Typical symptoms include the following:
- the appearance of shortness of breath, which increases significantly after physical exertion. Over time, shortness of breath begins to appear even with light exertion;
- strong pulsation in the head;
- frequent tachycardia (many patients mistake it for palpitations);
- pain in the cardiac region (they are the result of ventricular hypertrophy).
A special symptom that characterizes a congenital heart defect called bicuspid aortic valve is a violation of blood flow in which reverse movement occurs, i.e. blood leaves the aorta back into the ventricle. This manifestation of a defect in a patient can only be identified by a specialist conducting an examination, but it is for this reason that other signs appear.
Causes of the phenomenon
As the main reason for the development of this defect, doctors call the impact of harmful and dangerous factors on the body of a pregnant woman during the formation of elements of the cardiovascular system. This may be radiation exposure, x-ray exposure, infection, poor ecology and other mutagens.
The next factor is a woman’s smoking during pregnancy. Nicotine has a negative effect on the formation of any organs during fetal development.
It affects the development of the bicuspid aortic valve and heredity, it is transmitted from one of the parents. Therefore, doctors strongly recommend that those parents who have this anomaly conduct a full examination of the child immediately after birth in order to take the necessary measures and carry out therapy in a timely manner.
Treatment of diseases
If a bicuspid aortic valve is detected with grade 1 insufficiency, and it does not show any signs and does not affect the patient’s quality of life, does not interfere with physical activity, then the defect can be left for some time without surgical intervention. However, the patient must undergo periodic examinations, ultrasound scans and avoid overloading the heart. However, with age, surgery will still be indicated.
A bicuspid aortic valve requires surgical intervention, which involves:
- prosthetics (replacement with a biological or mechanical prosthesis);
- transcatheter implantation of valve prosthesis (modern method of percutaneous implantation).
Patient prognosis and recommendations
Now, about how long the patient will live after he is diagnosed with “Bivalve aortic valve”, the prognosis will depend on the rate of changes in the functioning of the organ caused by the presence of the defect, and on whether there is a manifestation of heart or coronary insufficiency.
If no serious destructive problems are found, then ten years may pass from the moment of diagnosis, but if destruction occurs and the presence of a defect affects the functioning of the organ, then the forecasts do not exceed two years.
Attention! This defect requires constant monitoring and observation by specialists, and clinical manifestations indicate the need for immediate treatment in a specialized clinic.
Even if the functional bicuspid valve does not affect the rhythm of life, doctors recommend avoiding nervous strain, trying to avoid stress, maintaining a work-rest schedule, eating more vitamins (in the form of vegetables and fruits) and be sure to take daily walks in the fresh air. Prevention should be aimed at protecting against infections such as endocarditis, and it also helps against sclerosis.
As for the question: bicuspid aortic valve and sports, it should be resolved individually in consultation with a doctor.