The cause of fibrosis and how to diagnose it
An important role in the functioning of the valvular apparatus of the heart is played by the valves, which are represented by loose connective tissue consisting of dense collagen and continuously extending into the chordae tendineae (according to Wikipedia).
Under a number of circumstances, the number of blood vessels supplying the structure of the valves is reduced. As a result, elastic fibers are replaced by dense fibrous tissue, which is characterized by sufficient strength. Having lost lability, the valves lose the ability to provide physiological hemodynamics. Most often, the mitral valve is affected by pathology, less often – the aortic valve. Classification of pathology:
- focal. There is moderate damage to the structure of the valve apparatus;
- diffuse. The affected area covers the leaflets and subvalvular space;
- cystic. It is characteristic of an advanced stage and is considered a separate pathology with the formation of cavity formations.
Fibrosis of the aortic and mitral valve leaflets is explained by the following reasons:
- age-related changes with loss of natural collagen potential;
- rheumatic attack (especially repeated), for example, after oropharyngeal infections. The damage is attributed to antibody formation and cross-reactivity between group A streptococcal carbohydrates and heart valve glycoprotein. According to research, almost every five-year-old child has a history of a throat infection. It is possible to develop chronic rheumatic heart disease with damage in the form of post-inflammatory marginal fibrosis;
- Marfan syndrome, dysplasia, in which the anatomical and functional features of the connective tissue are genetically abnormal;
- atherosclerosis of the aorta. Calcification of plaques and subsequent thickening of its wall;
- foci of necrosis (with a heart attack) or inflammation (with myocarditis) near the valve ring.
Diagnosing fibrosis is not very difficult. Initially, clinical blood and urine tests are prescribed to detect the possible presence of inflammation. Biochemical research indicates changes in the levels of cholesterol, sugar, uric acid, total protein, and creatinine.
Ultrasound of the heart reveals the degree of narrowing, valve insufficiency, evaluates the contractile function of the myocardium, blood volume during systole.
X-ray examination reveals myocardial hypertrophy, pulmonary congestion, and calcification of valve fragments.
CT, MRI, CAG are performed if surgical intervention for prosthetic structures is necessary.
Diagnostic examination
Considering the fact that the symptoms of thickened aortic walls do not appear immediately, the patient begins to notice the first signs when the disease has already progressed. In some cases, pathology is detected during a routine medical examination, using fluorography.
Ultrasound of the heart
To clarify the diagnosis, ultrasound of the heart muscle, circulatory system and contrast angiography of blood vessels are performed. For people who have a genetic predisposition to diseases of the cardiovascular system, heart diagnostics should be carried out once a year.
How does this process affect the patient’s quality of life?
The symptoms of the disease depend on which specific valve is affected by fibrosis, although some signs of pathologies may coincide. Most often, the patient does not show any complaints for a long time, his condition remains satisfactory. Deterioration in well-being is typical for an advanced process and the formation of complications.
If the mitral valve leaflets are sealed, it is noted:
fatigue during routine physical activity and sports;- shortness of breath at rest;
- episodes of heart rhythm disturbances in the form of extrasystole or atrial fibrillation;
- chest pain;
- periodic swelling.
If the thickening of the mitral valve leaflets continues to progress in the absence or ineffectiveness of treatment, MVP occurs with varying degrees of regurgitation or without.
Fibrosis of the aortic valve walls causes:
- progressive shortness of breath;
- pain in the heart during exercise;
- dizziness and fainting when playing sports;
- heartbeat disturbances.
Sometimes the life of a patient with cusp fibrosis is complicated by episodes of hemoptysis and asthmatic attacks due to hemodynamic disturbances.
For young patients, issues related to pregnancy and military service come to the fore. The first is decided individually depending on the stage of the fibrotic process, the presence of stenosis and hemodynamic disturbances. A woman carrying a child is observed, in addition to an obstetrician-gynecologist, by a cardiologist. Childbirth takes place by caesarean section.
The army and the opportunity to engage in professional sports depend on the decision of the medical commission. It is taken into account whether the pathology led to a pronounced defect and the presence of concomitant diseases.
Mitral valve prolapse
18.09.2014
Mitral valve prolapse
General information about mitral valve prolapse, its clinical picture and diagnosis.
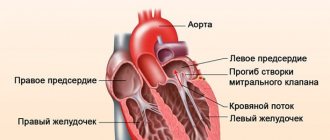
Mitral valve prolapse is sagging (bending) of the mitral valve leaflets into the left atrium.
Mitral valve prolapse syndrome, or Barlow's syndrome , was described by J. Barlow in 1963 and is extremely common - in 5-10% of people in the population.
It is necessary to distinguish between true prolapse of the valves and their wave-like sagging (billowing).
In many cases, mitral valve prolapse is asymptomatic (has no symptoms); in some cases, (heart rhythm disturbances), the presence of a characteristic noise when listening to tones , chest pain , and shortness of breath can be observed . Emotional lability, fatigue and other nonspecific clinical signs are also recognized as associated with mitral valve prolapse .
Prolapse, or sagging, of one or both cusps of the mitral valve during systole into the cavity of the left atrium is considered true only if it is recorded in two echocardiographic positions: apical four-chamber and parasternal along the long axis of the left ventricle.
Diagnosis of mitral valve prolapse is carried out during an echocardiographic study carried out in B-mode, M-mode, color and spectral Doppler modes.
In the expert practice of ultrasound examinations of the heart, only a combination of all modes allows one to obtain a holistic understanding of the nature of the process, the presence and severity of hemodynamic disorders.
In a number of countries, there is a rule to perform any surgical interventions in patients with prolapse syndrome under the guise of antibiotics in order to prevent complications.
Currently in our country there is overdiagnosis of mitral valve prolapse in children and adolescents.
This may be due to incorrect execution of the research procedure (technique) - incorrect identification of the apical position of the heart. In addition, a slight sagging of the base of the anterior leaflet of the mitral valve in children and adolescents up to 3–5 mm is normal if it is not accompanied by pathological regurgitation. In addition, the valve leaflets and chords develop faster than the fibrous rings, therefore, sagging of the leaflets is more often recorded in childhood and adolescence.
It is necessary to distinguish between physiological mitral valve prolapse - without disrupting its function, and pathological mitral valve prolapse - with pathological mitral regurgitation.
Mitral valve prolapse syndrome is characterized by young age of patients - usually 20–50 years; predominance of women; the presence of noise - a “click” during auscultation, thickening of the valves and their systolic displacement during echocardiography, hypotension, as well as mitral regurgitation during Doppler examination, the degree of which exceeds physiological.
Myxomatous degeneration is not uncommon , signs of which are found in older patients - 40-70 years old, among whom males predominate. In these cases, pathological mitral regurgitation is detected by echocardiography, and there are pronounced changes in the leaflets that require cardiac surgical correction.
Myxomatous degeneration of the mitral valve leaflets, as one of the most common causes of mitral valve prolapse, can affect the leaflets of all heart valves, but the most common lesion is the mitral valve.
Over the past few years, the number of people suffering from this pathology has increased significantly throughout the world. Just 10 years ago, the majority of patients with myxomatous degeneration were patients with Marfan syndrome. Currently, the connection between unfavorable environmental factors and the use of a number of weight loss drugs in the occurrence of this pathology has been proven. The number of patients over 70 years of age suffering from myxomatous degeneration has increased significantly.
An echocardiographic examination clearly shows scalloped, “serpentine”, uneven, thickened cusps of the mitral valve. They prolapse into systole into the cavity of the left atrium. Rounded protrusions are formed on the valves, resembling small tumors - myxomas. This is where the name of this pathology comes from. You can often observe separation of the valve chords.
Most patients with myxomatous mitral valve degeneration demonstrate cardiac arrhythmias—atrial fibrillation or frequent ventricular extrasystole. The causes of arrhythmia are pathological mitral regurgitation against the background of myxomatous changes in the valve leaflets and, as a result, increased pressure in the cavity of the left atrium.
Patients with myxomatous degeneration require dynamic monitoring; those with significant mitral regurgitation require consultation with a cardiac surgeon.
The nature of changes in the structure of the mitral valve leaflets and the occurrence of pathological mitral regurgitation can contribute to infection of the valve. Differential echocardiographic diagnosis in this case may be difficult.
The differential diagnosis of myxomatous degeneration of valve leaflets should be made with infective endocarditis and Lamble's growths. Clinical and laboratory diagnostics play an important role in this. Thus, with myxomatous degeneration there is no inflammatory reaction recorded during laboratory testing.
Secondary mitral valve prolapse occurs in the following situations:
- Marfan syndrome is a mesenchymal dysplasia. It is accompanied by a characteristic appearance of the patient (“Marfan-like type”) - increased joint flexibility, aortoanular ectasia, frequent development of aortic aneurysm and intimal detachment of the aorta in the thoracic ascending region and myxomatous degeneration of the valves and subvalvular structures. In this case, all heart valves prolapse. The degree of prolapse is usually significant. Pathological valvular regurgitation is recorded.
- Hypertrophic cardiomyopathy. In this case, mitral valve prolapse is associated with increased pressure in the cavity of the left ventricle during systole. Prolapse is especially pronounced in patients with obstructive hypertrophic cardiomyopathy.
- Ehlers-Danlos syndrome - connective tissue dysplasia syndrome - is a hereditary defect of hemostasis with damage to collagen structures. Accompanied by increased joint flexibility, increased skin stretching, bleeding and prolapse of heart valves
- Dysfunction of the papillary muscle due to myocardial infarction or cardiac injury is accompanied by prolapse of the valve leaflet and significant mitral regurgitation.
- Severance of the chords of the valve leaflet against the background of infective endocarditis, myxomatous degeneration, myocardial infarction, rheumatic lesions, etc. leads to prolapse of the leaflet and pathological valve regurgitation.
Assessment of the degree of mitral valve prolapse is carried out by assessing the severity of sagging of the leaflets:
- Minor mitral valve prolapse – 3–6 mm (1st degree mitral valve prolapse).
- Moderate mitral valve prolapse – 6–9 mm (2nd degree mitral valve prolapse)
- Significant mitral valve prolapse – more than 9 mm (grade 3 mitral valve prolapse).
It must be remembered that the degree of prolapse and the degree of mitral regurgitation may not correlate with each other . For example, when the chords are torn off at the end of the mitral valve leaflet, prolapse of up to 3 mm can be seen and grade 3–4 mitral regurgitation can be recorded.
Mitral valve prolapse is not a difficult diagnosis if echocardiographic examination is performed by an experienced specialist using high-resolution ultrasound systems.
What we offer for mitral valve prolapse:
The multidisciplinary medical professor offers you high-precision diagnostics of minor cardiac anomalies, including mitral valve prolapse, other cardiac and cardiovascular diseases only at an expert level.
Leading Russian specialists cooperate with us -
- Professor Sedov Vsevolod Parisovich,
- Professor Rybakova Marina Konstantinovna,
- Professor Khadzegova Alla Blalovna,
- Professor Tarasova Alla Alekseevna,
consulting cases of any diagnostic complexity in adults (V.P. Sedov, M.K. Rybakova, A.B. Khadzegova) and in children, including infants (A.A. Tarasova). Also, echocardiographic studies in adults in our clinic are carried out by doctors Natalya Vladimirovna Gerasimova and Natalya Mikhailovna Medvedeva. Echocardiography at home is performed by Oleg Evgenievich Isakov.
All echocardiographic studies in our center
(excluding procedures at home) are carried out on one of the world's best specialized ultrasound systems - Acuson Sequoia - 512 (Siemens AG, USA), equipped with all modern technologies and sensors.
See also:
- Echocardiography for adults
- Echocardiography for children
In addition to ultrasound examination of the heart, we also offer a wide range of services, including consultations with experienced cardiologists - Candidate of Medical Sciences Andrey Valentinovich Syrov and Candidate of Medical Sciences Olga Vladimirovna Morozova, electrocardiography, Holter ECG monitoring and 24-hour blood pressure monitoring, bicycle ergometry, any types of ultrasound and laboratory tests, consultations with various specialists.
A number of special programs for the prevention, diagnosis and treatment of the most common cardiovascular diseases have been created for you.
You can find more detailed information in other reviews and articles, as well as in the Services section.
We wish you good health and will be glad to see you at our clinic,
team of MPMC "Vascular Clinic on Patriarch's"
Treatment and observation of a patient with fibrosis of the valve apparatus
Often on forums you can read the question of whether fibrosis can be treated using folk remedies. The answer is clear: there are no such recipes. This process is quite difficult in therapy even for modern medicine.
It is important to know that the prescription of medications is indicated only for the clinical picture of heart failure, in which the following are used:
- cardiac glycosides - Celanide, Digoxin, Strophanthin;
- diuretics - Trifas, Indap, Veroshpiron;
- if indicated, antihypertensive and antiarrhythmic drugs.
Medicines only minimize the symptoms caused by fibrosis without affecting the progression of the disease.
Radical treatment consists of the following methods:
valve prosthetics to replace the diseased structure with a mechanical or biological analogue. As a rule, a median sternotomy using a heart-lung machine is used;- mitral commissurotomy, closed or open, with the task of dissecting pathological connections between the valve leaflets;
- coronary artery bypass grafting;
- endovascular prosthetics. The essence of the method is to insert a catheter with an implant through the femoral vessels without general anesthesia. Indicated for patients with severe chronic diseases;
- valve transplantation (a relatively new technique).
Indications for surgical intervention in fibrosis:
- neglect of the process;
- wrinkling of valves, tendon threads;
- the presence of pronounced calcification.
After the operation, the patient should be under medical supervision of a cardiologist. The patient is indicated for annual examinations and treatment in a cardio- or cardio-rheumatological sanatorium.
Aortic valve stenosis
The answer to the question of aortic stenosis, what it is, is quite simple - it is a narrowing or blockage of the aortic valve, which occurs when the valve leaflets become covered with deposits. Such deposits change the shape of the leaflets and reduce blood flow through the valve. The left ventricle must work to compensate for the decreased blood flow. Over time, the extra work to overcome this narrowing can weaken the heart muscle.
Provoking factors for the development of pathology
The causes of the disease in question are quite varied. Sometimes valve deformation is associated with age-related changes. The disease is often diagnosed in people aged 52 to 60 years. It is at this stage of life that all sorts of negative changes in the body make themselves felt, including:
- blockage of blood vessels;
- abnormal changes in lipid metabolism;
- formation of cholesterol plaques;
- increase in blood viscosity.
Against this background, the cusps of the mitral valve of the human heart also suffer. The described pathology rarely occurs in young children; its occurrence is associated with a hereditary predisposition.
However, if such a disease does not progress so quickly in childhood, then in an adult patient the disease develops very rapidly.
Additional stimulating factors for the occurrence of damper seals can be:
- chronic diseases of infectious or viral origin;
- myocardial infarction;
- allergic manifestations to the irritant;
- rheumatism or endocarditis.
In addition, it has been proven that smoking and drinking alcohol increases the risk of developing the anomaly in question.
Common diagnostic methods and methods
Thanks to modern medicine, the diagnosis of the described disease is carried out with high accuracy and does not take much time. In addition, such an examination is absolutely easy.
During a visual examination, a qualified specialist will undoubtedly pay attention to the pale tint of the epidermis, the cyanosis of the patient’s lips and legs.
Next, more precise methods are used (by the way, the thickness of the dampers over 6 mm is considered a significant deviation). In order to identify compaction of the anterior (posterior) valve of the mitral valve, the attending cardiologist usually prescribes the following procedures:
- Echocardiography (EchoCG). Provides information about the extent of valve damage and the stage of the pathology.
- Electrocardiogram (ECG). Indicates hypertrophy of the cardiac zones.
- Obtaining an x-ray of the chest area. It will help determine the presence of congestion in the lungs.
- Auscultation. Detects heart murmurs.
- MRI. Allows you to detect the slightest neoplasms in the valve apparatus of a characteristic organ.
At the discretion of the doctor, the patient may additionally be required to donate blood (urine) for clinical or biochemical analysis.