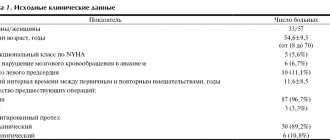
Structure and functions of the pulmonary valve
The pulmonary valve consists of three movable semilunar leaflets, attached at their base to the fibrous ring surrounding the exit from the right ventricle of the heart. The valve is designed to prevent blood from flowing back from the pulmonary trunk into the right ventricle. In the phase of cardiac contraction (systole), an increase in pressure in the right ventricle leads to deflection of the valve leaflets towards the pulmonary artery, and blood flows freely into the pulmonary circulation. In the resting phase (diastole), the valve leaflets, under the influence of high pressure in the pulmonary trunk basin, completely close the outlet.
Publications in the media
Pulmonary valve insufficiency is the inability of the pulmonary valve to prevent the reverse flow of blood from the pulmonary trunk into the right ventricle during diastole.
Etiology • Relative deficiency in pulmonary hypertension • Congenital defects • Infectious endocarditis in drug addicts • Marfan syndrome • Rheumatism • Carcinoid syndrome • Syphilis • Idiopathic dilatation of the pulmonary artery. Pathophysiology • Pulmonary valve regurgitation leads to volume overload of the right ventricle • In the absence of pulmonary hypertension, the right ventricle is able to cope with significant volume overload as long as its normal contractility is maintained and there is no severe tricuspid valve regurgitation • When pulmonary valve regurgitation and pulmonary hypertension combine, overload occurs right ventricle both volume and pressure • In acute severe pulmonary valve insufficiency - right ventricular failure.
Clinical picture and diagnosis • Complaints arise due to associated right ventricular failure and tricuspid insufficiency. • Objective data •• Swelling of the jugular veins •• Palpation detectable pulsation of the right ventricle •• Palpation detectable II tone and diastolic tremor •• Strengthening of the pulmonary component of the II sound •• In case of leaflet defects, the pulmonary component of the II tone is weakened or absent •• Decreasing diastolic Graham Still murmur . The duration of the noise depends on the rate of equalization of diastolic pressure in the pulmonary artery and right ventricle.
Special studies • ECG: signs of hypertrophy and overload of the right heart. • Jugular venogram: wave V indicates tricuspid regurgitation due to right ventricular failure. • Chest X-ray •• Bulging of the pulmonary artery arch •• Increased pulmonary vascular pattern and dilatation of the right heart depend on the presence or absence of pulmonary hypertension. • EchoCG •• Vegetations, dilatation of the fibrous ring of the pulmonary artery, bulging of the interventricular septum into the cavity of the left ventricle •• Severity of regurgitation (see Aortic valve insufficiency) •• Increased systolic pressure in the right ventricle and pulmonary artery. • Catheterization of the cardiac cavities •• Increasing end-diastolic pressure in the right ventricle and central ventricle •• Carrying out tests with aminophylline and oxygen to determine the reversibility of pulmonary hypertension. • Pulmonary angiography: the flow of contrast material from the pulmonary artery into the right ventricle during its diastole.
TREATMENT • Drug therapy •• Treatment of right ventricular failure (diuretics and venous vasodilators) •• For any organic damage to the valve - prevention of infective endocarditis; for relative failure, prevention is not indicated. • Surgical treatment •• Indications: clinically pronounced right ventricular failure in severe infective endocarditis that does not respond to antibiotic therapy •• Methods of surgical treatment: valve replacement with a biological or, less commonly, mechanical prosthesis. See also Tricuspid valve insufficiency.
Specific complications • PE • Secondary infective endocarditis • Thrombosis of the prosthesis • Degenerative changes in the biological prosthesis and the need for re-prosthesis. The prognosis depends on complications and concomitant pathology; Pulmonary valve insufficiency itself usually does not affect the prognosis.
ICD-10 • I37 Pulmonary valve lesions
Pulmonary valve defects
There are several types of pulmonary valve defects:
- Pulmonary valve insufficiency. In this disease, the failure of the semilunar valves to completely close the outlet leads to reverse flow of blood from the pulmonary artery into the right ventricle. Pulmonary valve insufficiency leads to a decrease in the volume of blood entering the lungs and makes it difficult to fill the ventricle, causing overload and hypertrophy of the right side of the heart;
- Stenosis (narrowing) of the pulmonary valve. With stenosis, pathological changes in the leaflets and the fibrous ring narrow the lumen of the exit from the right ventricle, significantly reducing the volume of pulmonary blood flow. The right ventricle of the heart is forced to constantly overcome high resistance caused by stenosis, which quickly leads to its hypertrophy, and then to irreversible dystrophic changes. Decompensated pulmonary stenosis manifests as severe symptoms of decreased pulmonary perfusion and right-sided heart failure. This defect is often combined with complex congenital cardiac malformations, such as the triad and tetralogy of Fallot;
- Pulmonary atresia is a severe congenital heart defect characterized by the absence of an opening between the right ventricle and the pulmonary trunk. A completely closed valve prevents blood from entering the lungs. During the prenatal period, due to the absence of pulmonary respiration of the fetus, this defect does not interfere with normal development. Immediately after the birth of a child, pulmonary atresia leads to a critical condition requiring intensive resuscitation measures. Pulmonary blood flow with this defect is supported by an open arterial duct, the throughput of which does not meet the body's requirements.
Correction or replacement (prosthetics) of heart valves
Indications
There are 2 valves that separate the upper chambers of the heart (atria) from the lower ones (ventricles) - mitral (bicuspid) and tricuspid (tricuspid), as well as 2 valves that separate the lower chambers of the heart from the large arteries - aortic and pulmonary.
Each of these four valves is responsible for the unidirectional flow of blood during contraction of the atria and ventricles - so that the blood entering the heart enters the large arteries and then throughout the body. If one of the valves is damaged - whether due to leaky closure of the leaflets (valvular insufficiency) or severe narrowing of the opening (stenosis), blood flow is disrupted, and as a result, the function of the entire heart is impaired. In the first case, during ventricular contraction, the valve is unable to prevent retrograde blood flow from the ventricle into the atrium (so-called regurgitation occurs). In the second case, the valve does not open enough to allow free blood flow from the atrium to the ventricle or from the ventricle to the aorta/pulmonary trunk.
Valvular insufficiency can be the result of rupture of several chordae tendineae connecting each of the valve leaflets with the papillary muscles - this is possible with some heart diseases, with connective tissue diseases (including congenital), as well as with traumatic lesions. Stenosis often occurs against the background of rheumatic diseases.
Correction or replacement of heart valves is indicated in both cases - both with valvular insufficiency and with stenosis. The need for surgical intervention is decided depending on the severity of the insufficiency/stenosis.
For valve insufficiency, various types of surgical interventions are used. Here are some of them:
1) installation of synthetic chords instead of broken ones;
2) triangular/quadrangular resection of the valve;
3) transplantation of own chords;
4) edge-to-edge plastic surgery using the Alfieri method;
5) in case of mitral valve insufficiency due to coronary heart disease, annuloplasty or implantation of a biological prosthesis without removing the own valve is used.
Upon completion of the correction, transesophageal echocardiography is performed to assess the effectiveness of the intervention. If the results are unsatisfactory, either additional correction or valve replacement is performed.
Various types of surgical interventions are also used for valve stenosis. Including:
Causes of pulmonary valve damage
Among the causes of pulmonary valve defects, it is important to note:
- Congenital heart pathologies caused by genetic mutations, as well as exposure during pregnancy to infectious agents and external teratogenic factors;
- Hereditary connective tissue diseases leading to changes in the area of the pulmonary trunk and the fibrous ring of the valve (Marfan syndrome);
- Complications caused by rheumatic endocarditis or inflammation of the endocardium of non-rheumatic origin;
- A consequence of diseases that cause dilatation of the right side of the heart (stretching of the fibrous ring can lead to relative insufficiency of the pulmonary valve);
- Tumors of the heart and mediastinum;
- Consequences of chest injuries.
Clinical picture of pulmonary valve defects
Symptoms depend on the type of defect, the degree of damage to the valve and the age of the patient. The most severe symptoms are observed in newborns suffering from pulmonary atresia. Severe cardiac and respiratory failure threatens the lives of young patients in the first minutes after birth and requires intensive treatment. Isolated stenosis and complex defects with a narrowing of the exit to the pulmonary artery are classified as cyanotic (or “blue”) defects, due to the characteristic skin color. Cyanosis is caused by reduced pulmonary blood flow and lack of oxygen in organs and tissues.
In addition to signs of reduced pulmonary blood flow, patients with aortic valve defects suffer from heart failure, the symptoms of which include:
- Difficulty breathing (shortness of breath), which occurs with minimal physical exertion, and in severe forms of the disease even at rest;
- Rapid heartbeat (tachycardia), often accompanied by other heart rhythm disturbances;
- Edema of the lower extremities, and in severe cases of the pelvis, abdomen, as well as accumulation of fluid in the abdominal cavity;
- Infant patients experience difficulties during feeding, refusal to eat, malnutrition;
- In children, pulmonary valve defects lead to severe delays in physical development.
Diagnosis of pulmonary valve defects
Diagnosis of severe congenital defects is carried out immediately after the birth of the child. Mild forms of valvular insufficiency, as well as acquired pathologies, are diagnosed at a more mature age when symptoms appear or during clinical observation. A characteristic objective sign of the defect is a murmur detected by a doctor during auscultation of the heart. For the final diagnosis of congenital and acquired pulmonary valve defects, the clinic’s cardiologists use high-precision research methods, including:
- Echocardiography – visualization of the heart using an ultrasound scanner;
- Chest X-ray to evaluate heart size and pulmonary changes;
- Contrast radiography according to the vascular research protocol (angiography), including coronary angiography;
- Measuring oxygen levels and pressure in the chambers of the heart using minimally invasive catheterization;
- Pulse oximetry – non-invasive monitoring of blood oxygen saturation;
- Electrocardiographic studies (real-time ECG recording and long-term heart rate monitoring). Recording the electrical potentials of the heart helps cardiologists diagnose ischemic disorders, arrhythmias and myocardial hypertrophy accompanying valvular disease;
- Tomographic methods for studying the heart (computer and magnetic resonance imaging);
- Isotope scanning of pulmonary perfusion.
Treatment of pulmonary valve stenosis
In certain cases, only medical monitoring of the patient's health condition or symptomatic treatment is required. As the severity of symptoms of pulmonary valve stenosis or insufficiency increases, surgery to correct or replace the valve is indicated. The Assuta Clinic™ is one of the best medical centers in Israel where such operations are performed.
Specialists at the Assuta™ clinic diagnose pulmonary valve disease, assess the severity of the disease, the presence of symptoms, and draw up an individual treatment plan, taking into account, among other things, the patient’s personal preferences.
Treatment for pulmonary valve stenosis may include:
- Constant medical supervision. If the disease is asymptomatic and its severity is diagnosed as mild or moderate, your doctor will recommend regular diagnostic tests and ongoing medical monitoring. This is necessary for timely diagnosis of changes in the condition of the pulmonary valve. You will need prophylactic antibiotics before undergoing any surgical procedures and before dental treatment. Antibiotic therapy is prescribed to prevent a serious infection of the heart valves called bacterial endocarditis.
- Drug therapy. Your doctor may prescribe medications to treat shortness of breath, reduce cardiac stress, and regulate your heart rhythm. However, in most patients, drug therapy is not able to effectively combat the progression of heart valve disease.
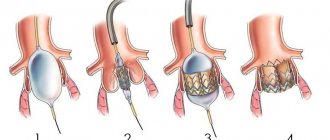
- Therapeutic cardiac catheterization. During cardiac catheterization, the doctor inserts a thin tube (catheter) through a peripheral vein in the lower limb. The catheter is passed through the vessels and reaches the heart. Instruments are then inserted through the catheter to perform fine manipulations on the heart. The Assuta™ clinic performs percutaneous interventions for the treatment of pulmonary valves and balloon repair of heart valves. These procedures are indicated for patients who meet certain criteria.
- Surgery. During surgery, it is possible to separate the fused valve leaflets or stitch their ruptures. It is also possible to recreate the natural shape of the valve to ensure complete closure of the leaflets and closure of the valve. Most often, surgeons replace the pulmonary valve with a prosthesis. Such a prosthesis will most likely need to be updated after a few years.
Specialists at the Assuta™ clinic have developed a number of new surgical techniques for performing minimally invasive surgical interventions. During such operations, the valve is replaced through several small incisions in the skin.
At the Assuta™ clinic, a treatment plan is drawn up individually for each patient, based on the nature of the disease, the presence of symptoms, the patient’s age and various risk factors.
Modern methods of treatment of pulmonary valve defects
Drug treatment of pulmonary artery defects is aimed at preventing the development and progression of heart failure. Infants with pulmonary atresia are given drugs to prevent closure of the ductus arteriosus until emergency surgery is performed. Surgical treatment, in most cases, can normalize hemodynamics by eliminating the heart defect.
The following operations for pulmonary valve defects are performed at the Herzliya Medical Center Hospital:
- Percutaneous puncture for pulmonary atresia followed by balloon dilation. The procedure is performed to restore pulmonary perfusion in newborns;
- Balloon expansion of stenosis, stenting and the use of an innovative cutting balloon technique, which allows not only to expand the narrowed area, but also to remove excess fibrous tissue, leading to relapse of stenosis;
- Organ-preserving procedures for the reconstruction of a damaged valve, preventing the need for its replacement;
- Open heart surgery to restore normal patency in atresia and stenosis of the pulmonary trunk;
- Pulmonary valve replacement surgery. Artificial biological or mechanical valves fully cope with their function, guaranteeing the restoration of hemodynamics for many years.
Innovative technologies of open and minimally invasive cardiac surgery, widely introduced at Herzliya Medical Center, have changed the prognosis of severe heart defects. Thanks to the combination of experienced surgeons, excellent hospital conditions, highly professional post-operative care and intensive rehabilitation therapy, thousands of patients from all over the world have been restored to a full and active lifestyle.