Arterial disease most often manifests itself as pain in the legs (so-called intermittent claudication). The pain is of a certain nature: when a person begins to walk, after some time, when covering a certain distance, pain appears in the calves (on one or both sides), which may require rest. This is explained by the fact that when under load, the muscles require a large blood flow, and this is limited due to the pathological narrowing of the arteries. Edema is not typical for arterial insufficiency. As the disease progresses, the walking distance decreases, hair falls out on the legs (hypotrichosis), and the leg muscles atrophy due to constant oxygen starvation. In the later stages of the disease, pain is also bothersome at rest, more at night when the legs are in a horizontal position, which reduces blood flow. When the patient lowers his legs down from the bed, the pain decreases. When the first symptoms of arterial insufficiency appear, you should immediately consult a doctor - this will prevent the development of severe complications - gangrene, etc.
The simplest, most accessible and informative method for studying the arteries of the lower extremities is ultrasound.
Below is a medical overview of the main surgical arterial diseases:
Etiology
The main etiological aspects of atherosclerosis in the arteries of the lower extremities do not differ significantly from the mechanisms of formation of atherosclerosis in any other localization. The main importance is given to lipid metabolism disorders. Against the background of increased cholesterol levels in the blood, cholesterol infiltrates the vascular wall. In this case, the predominance of low-density lipoproteins (LDL) is most important. An indicator reflecting the balance between the level of atherogenic and antiatherogenic lipids is called the atherogenic index (coefficient) and is an important indicator of predisposition to the development of atherosclerosis.
Another important etiological factor is damage to the vascular wall - smoking, hypertension, immunological disorders, etc.
The course of OASNK is significantly complicated by the presence of concomitant diabetes mellitus and atrial fibrillation.
Risk factors for OASNK
Atherosclerosis of the vessels of the lower extremities is characterized by the same risk factors as other arterial diseases, for example: coronary heart disease and cerebrovascular insufficiency.
- High blood pressure (hypertension),
- High blood cholesterol levels,
- Smoking,
- Sedentary lifestyle,
- Obesity,
- Burdened heredity.
A few words about smoking. Complete abstinence from any form of tobacco is necessary. Smoking even 1 cigarette per day of the lightest type is an unfavorable risk factor that causes the progression of obliterating atherosclerosis of the lower extremities and the development of its severe complications. The nicotine contained in tobacco causes the arteries to spasm, thereby preventing blood from moving through the vessels and increasing the risk of blood clots in them.
Pathomorphology
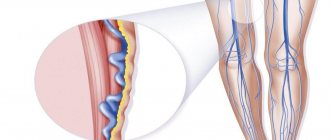
The main changes develop in the intima of the arteries. There are 5 morphological stages of atherosclerosis:
- Prelipidic – characterized by increased endothelial permeability, destruction of the basement membrane, destruction of elastic and collagen fibers.
- Stage of lipoidosis - focal infiltration of the arterial intima with lipids occurs.
- Stage of liposclerosis - a fibrous plaque forms in the intima of the artery.
- Stage of atheromatosis - destruction of the plaque occurs with the formation of an ulcer.
- Stage of atherocalcinosis – plaque calcification occurs.
Based on the type of damage to the vascular bed, segmental and diffuse atherosclerosis are distinguished. In the first case, the process develops in a limited area of the vessel from single plaques to complete occlusion of the lumen. This type is more favorable in terms of the potential for performing bypass reconstructive operations on blood vessels. The diffuse type involves widespread atherosclerotic lesions predominantly in the distal bed, leaving no “window” for the surgeon to apply a shunt or prosthesis. The destiny of such patients is conservative therapy in order to delay the onset of gangrene as much as possible.
Clinical picture
The clinical picture of the disease depends on the stage of chronic arterial insufficiency of the lower extremities (CAI). The main subjective manifestation of the disease is pain in the calf muscles, initially associated with walking at various distances, and then at rest. In the later stages of the disease, pain occurs not only in the legs, but also in the feet and fingers. It should be borne in mind that when the bifurcation of the aorta and iliac arteries is damaged, pain can also occur in the muscles of the thighs and lower back, and impotence often develops (Leriche syndrome). Most clinical classifications of CHANC are based on pain syndrome.
We believe that the Fontan classification with some modifications is most suitable for clinical use.
Stage 1 – patients complain of pain in the calf muscles when walking about 1 km. The pain causes the patient to limp (intermittent claudication), but the lameness goes away with rest. These pains are associated with muscle ischemia caused by difficult access to arterial blood. At this stage, the symptoms are transient, the pulse in the lower extremities is preserved at all levels (may be weakened), the color of the lower extremities is not changed, there is no muscle atrophy, but hypotrichosis (reduced hair growth in the distal extremities) and changes in the nails in the form of brittleness may occur , susceptibility to fungal diseases.
Stage 2A – pain appears when walking a distance of 200 to 500 meters.
Stage 2B – intermittent claudication occurs when walking less than 200 meters. At this stage, one can observe hypotrichosis, changes in the nails, wasting of the muscles of the legs, pallor of the skin of the distal parts of the lower extremities. The pulse in the foot is usually absent; above it, it can be preserved, depending on the level of the lesion. It should be noted that many patients consult a doctor at this stage, because it significantly reduces the quality of life of patients.
Stage 3 is characterized by severe hemodynamic disturbances in the limb, its main symptom being pain when walking less than 50 meters and pain at rest. Pain at rest mainly bothers patients at night, because... horizontal position of the limb in bed reduces the flow of arterial blood to the distal areas. To increase blood flow, and therefore reduce pain, patients have to lower their legs from the bed up to several times a night. Based on this sign, some authors distinguish stages 3A and 3B of the disease.
Stage 3A – patients lower their legs out of bed up to 5 times per night.
3B – more than 5 times a night or sleep half-sitting with legs down.
At the third stage of the disease, all of the above disorders (hypotrichosis, atrophy, etc.) increase, and mental disorders caused by constant pain and lack of sleep are added. Patients become irritable, faith in the success of treatment decreases, many try to resort to “folk” remedies, which often worsens the course of the disease, causing the appearance of trophic disorders and sometimes gangrene. The pulse on the foot is not detected, on the popliteal artery - rarely, on the femoral artery, in the case of high occlusion, the pulse is not detected.
The photo shows skin necrosis in the area of the metatarsophalangeal joint against the background of obliterating atherosclerosis of the arteries of the lower extremities.
During treatment, the wound cleared and granulated (began to heal).
Treatment technologies at the Innovative Vascular Center
The vascular surgeons of our clinic have significant experience in diagnosing and treating both planned and complicated lesions of the popliteal artery. The main method of treatment in our clinic is autovenous replacement of the popliteal aneurysm. This technology shows better immediate and long-term results. For complicated aneurysms, open surgery allows you to restore the patency of not only the popliteal artery, but also the vessels of the leg. Endovascular interventions for extensions of this localization have very poor results due to the high mobility of the knee joint.
Gangrene
The development of gangrene marks stage 4 of HUNC. Between the third stage and the appearance of gangrene, a phase of critical limb ischemia has recently been distinguished, which is characterized by intense pain at rest with the formation of superficial distal necrosis and trophic ulcers.
Gangrene manifests itself by the appearance of bluish lesions on the toes or heels, which subsequently become black. The lesions tend to spread, merge, and involve the proximal parts of the foot and lower leg.
Traditionally, dry and wet gangrene are distinguished. Their main difference is the delimitation (demarcation) of the area of necrosis from other tissues. With dry gangrene, there is an area of black skin, clearly demarcated from the surrounding unchanged tissue, with no tendency to spread. The general condition of the patients does not suffer (except for persistent pain), there are no signs of intoxication, and there is no hyperthermia. This type of gangrene with a small affected area (for example, dry gangrene of the distal phalanx of the toe) can be managed conservatively for a long time, without giving indications for surgery; in some cases, self-rejection of the necrotic area is possible. Haste with surgery in such a situation, due to surgical trauma, can cause progression of the necrotic process.
With wet gangrene, there is no demarcation, there are areas of both black and bluish color on the foot, the skin proximal to the focus of necrosis is hyperemic, and from under the necrosis there is a purulent discharge with an unpleasant odor. There are signs of intoxication (thirst, tachycardia, etc.), hyperthermia to subfebrile and febrile levels. The wet process is characterized by rapid progression, with necrosis spreading in the proximal direction.
In stage 4, some authors distinguish between stage 4A - when there is a prospect of preserving the supporting function of the limb (for example, if it is possible to perform amputation according to Sharp or Chopart while maintaining the supporting function of the heel) and 4B - when the patient is shown a high amputation at the level of the thigh or lower leg.
The presence of concomitant atrial fibrillation in a patient can cause a rapid transition from one stage of arterial insufficiency to another. With atrial fibrillation, in many patients, thrombotic masses accumulate in the left ventricle of the heart, the separation of which and migration in a large circle to the lower extremities can aggravate the existing arterial stenosis with transition to a more severe stage of ischemia, up to the development of gangrene.
Some tests can help in diagnosing limb ischemia, for example, the finger pressing symptom, Oppel's plantar ischemia symptom, Goldflam's test, Panchenko's knee phenomenon, etc.
Course and complications
The main risk from a popliteal aneurysm is associated with embolization - blockage of the underlying arteries with pieces of blood clots or occlusion of the aneurysm cavity. Both of these complications can lead to acute ischemia and gangrene of the legs (sudden loss of blood supply). Blood clots (thrombi) gradually form in the cavity of the vessel. When this clot remains attached to the wall of the vessel, it does not pose any danger. If a clot fragment breaks off, it can travel far from the aneurysm and cause blockages in small arteries, preventing blood flow to downstream tissues. A popliteal aneurysm can rupture (rupture), but this is much less common than embolization. In this case, a pulsating hematoma occurs behind the knee. Simultaneously with the rupture, the next stage is thrombosis of the popliteal artery with the development of signs of acute circulatory failure of the limb. Most people develop severe ischemic changes and death of the leg. Only surgery performed within the next 6-12 hours after the complication will help avoid amputation.
Data from laboratory and instrumental examination methods
Laboratory examination allows us to identify patients at risk of developing atherosclerosis (increased blood cholesterol, atherogenicity index), identify patients with diabetes mellitus (increased blood glucose levels), which significantly complicates the course of the disease, and assess the state of the blood coagulation system (coagulogram). Culture from a trophic ulcer allows you to identify the causative agent of infection and prescribe rational antibiotic therapy.
Instrumental methods.
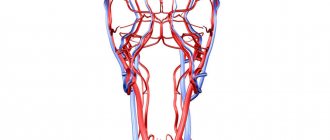
The most accessible and informative method, successfully used in outpatient settings, is currently recognized as duplex ultrasound scanning of the arteries of the lower extremities (USAS) - an ultrasound method that allows you to assess the condition of the vascular wall, identify atherosclerotic plaques, determine the level and extent of arterial occlusion, and assess the type blood flow, measure important indicators (brachial-ankle index, etc.). The study should be carried out in all patients suspected of having any stage of CANDC.
Currently, surgeons in Moscow practically do not use rheovasography (RVG) in the diagnosis of OASNK, because it allows you to determine only the deterioration of the arterial blood supply to the lower extremities, which is easily diagnosed based on clinical signs and USAS data.
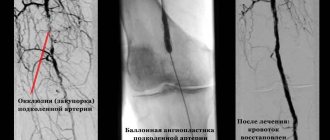
Angiography is a radiopaque research method used in a hospital setting to clarify the localization of the process and select the method of surgical intervention. The method is highly informative, but since it is not used in outpatient practice, we will not dwell on it in detail.
Microcirculation disorders are determined using capillaroscopy, transcutaneous determination of oxygen tension in superficial tissues and laser Dopplerography - they are of more scientific than practical interest.
Preparation for lower extremity vein bypass surgery
Before surgery, the patient should undergo a number of preparatory measures:
- Comprehensive examination of the cardiovascular system (narrowed blood vessels can be in all parts of the body);
- Take a general blood test;
- Get an ECG and ultrasound of blood vessels.
It is important to tell your doctor right away what medications you are taking. Based on this data, the phlebologist will determine which medications you should continue to use and which ones you should exclude before surgery.
Treatment
OASNK is a chronic, continuously progressive disease that requires constant treatment and monitoring of the patient. Treatment tactics depend on the stage of the disease, immediate clinical manifestations, and concomitant pathology.
All patients diagnosed with OASNK must immediately and permanently quit smoking. It is extremely important to control blood cholesterol levels and correct them, which can be carried out together with a cardiologist. All patients need an ECG and consultation with a therapist (cardiologist) to identify risk factors for atherosclerosis such as atrial fibrillation and hypertension. If diabetes mellitus is detected, the patient should be observed by an endocrinologist.
At stages 1 and 2A of the disease, the patient is prescribed a course of treatment with vascular drugs (antiplatelet agents, angioprotectors, agents that improve microcirculation, etc.) - trental, aspirin, nicotinic acid, reopolyglucin, actovegin, etc.
The following treatment regimen can be recommended:
Trental 400 mg x 3 times a day – 1 month
ThromboASS 50 mg/day 2 months
Nicotinic acid 1.0 x 3 r per day IM (can be 1 t x 3 r) – 3 weeks
If intravenous drips are possible (for example, in the presence of a day hospital) -
Reopoliglucin 400.0 IV drip, every other day No. 5.
Actovegin 10.0 in saline solution 400.0 IV drip, every other day No. 5.
Up to three such courses are required per year. The effect is assessed by increasing the walking distance and improving blood flow indicators according to USAS. If, despite the therapy, no positive effect is observed, it makes sense to hospitalize the patient as planned for inpatient examination and treatment.
Stages 1 and 2A CHANC are always subject to conservative treatment. In the presence of stage 2B, as well as in stage 3 CHANC, the patient should be referred for a consultation with an angiosurgeon to decide on the advisability of surgical treatment. Currently, shunt and prosthetic operations are used, as well as lumbar sympathectomy (the effectiveness of the latter method has recently been disputed by many authors). Stenting is gaining increasing acceptance.
In case of stage 3 CHANC, it is advisable to hospitalize the patient as planned for treatment in a hospital setting. If the patient refuses hospitalization, it is advisable to carry out the following course of treatment:
Trental 400 mg x 3r – 1 month
Xanthinol nicotinate 1.0 x 2p – 3 weeks
ThromboASS 50 mg/day continuously
Aevit 1 tablet x 3p 10 days
Neuromultivitis 1t x 3p – 2 weeks
Reopoliglucin 400.0 IV drop daily No. 10
Alprostan 100 mcg per 250 ml of saline solution IV drop, slowly 1 r per day, No. 14. or Vazaprostan 20 mcg per 250 ml saline solution IV drop for at least 2 hours 1 r per day No. 14.
Alprostan and vazaprostan should be administered with caution, under the control of blood pressure, due to the possibility of its decrease in elderly and debilitated patients.
In the complex therapy of OASNK, such drugs as Vesel Due F, Tanakan are also successfully used.
For pain syndrome, it is necessary to prescribe analgesics per os and parenterally (depending on the severity of pain). Both non-narcotic analgesics (ketorol, pentalgin, etc.) and centrally acting drugs (tramal) or combined ones (zaldiar) are used.
In patients with concomitant diabetes mellitus, it is advisable to include in the treatment regimen thioctic acid preparations that improve carbohydrate and lipid metabolism (for example, Espa-lipon or Berlition 600 mg per 250 ml of saline solution intravenously for 2 weeks, then in tablets for 200 mg x 3-4 times a day for 3 months).
At stages 2B – 3 of CANDC, it is advisable for patients to avoid physical activity, especially those related to walking, hypothermia or, conversely, overheating of the lower extremities. It is especially dangerous to steam your feet in hot water, because... disruption of arterial blood flow to the limb due to overheating causes the appearance of trophic disorders, including the development of gangrene.
Critical ischemia and the development of dry or wet gangrene are indications for emergency hospitalization of the patient.
Particularly difficult is the treatment of trophic disorders in the form of ulcers against the background of stage 3 A-B CHANK or critical ischemia of the lower limb. In such patients, pain is constantly present, the ulcers are poorly cleaned, and often with the most adequate and persistent treatment, there is a progression of the necrotic process, ultimately leading to amputation. All patients with trophic disorders should be consulted by an angiosurgeon to decide on the possibility of performing reconstructive vascular surgery or stenting. If such an operation can be performed, it significantly improves hemodynamics in the limb, which significantly accelerates the healing of ulcerative defects. Contraindications to reconstructive operations are usually: damage to the distal vascular bed, which excludes the possibility of applying a shunt, severe concomitant pathology, which gives a high surgical and anesthetic risk of intervention. In such a situation, if appropriate conditions exist (short extent of stenosis, etc.), stenting can be performed as a minimally invasive and fairly safe method.
Conservative therapy of trophic disorders comes down to two areas.
1. Conducting drug therapy aimed at improving microcirculation in the affected limb and relieving pain according to the above schemes. At the beginning of treatment of purulent-necrotic ulcers, it is necessary to carry out antibacterial therapy; a culture should be taken from the wound to determine the sensitivity of the microflora to antibiotics. Pending culture results, a broad-spectrum antibiotic such as a fluoroquinolone or cephalosporin may be prescribed. Further antibacterial therapy is carried out based on the culture results. The parenteral route of administration of the antibiotic is preferable, but if injections are not possible, tablet forms can be prescribed.
2. Local treatment - dressings. When treating a necrotic ulcerative defect, you must first ensure that it is cleansed of necrotic masses. To do this, daily dressings are carried out with enzymes (Chymotrypsin, Himopsin, Daltsex-trypsin wipes, etc.) or water-soluble ointments (Levomekol, Levosin). In case of severe pain in the area of the ulcer, it is preferable to use Levosin, which contains a local anesthetic.
After cleansing the ulcer, you can use ointment-based products for dressings - Solcoseryl, Actovegin, Panthenol-ratiopharm, etc.
For the treatment of almost clean, flaccid granulating ulcers, the drug “Curiosin” in drops has proven itself well - 1-2 drops per 1 cm2 of the wound surface.
If the wound has cleared, but is poorly granulated and epithelialized, Solcoseryl 2 ml intramuscularly, daily, No. 14 can be added to therapy.
Dressings are carried out as follows: a surgeon wearing sterile gloves treats the wound surface with a ball on tweezers moistened with a 3% solution of hydrogen peroxide, achieving maximum leaching of tissue detritus and remnants of medicinal substances from the wound. Then the wound is dried with a dry gauze ball, a medicinal substance is applied, and the wound is closed with sterile gauze pads, which are fixed with a gauze bandage. The bandage should not be applied tightly so as not to impair blood circulation in the limb.
In the initial stages (CHANK stage 1-2) of the disease, patients are prescribed sanatorium treatment - hydrogen sulfide baths, as well as physiotherapy.
More about atherosclerosis of the arteries of the lower extremities
Where is vascular bypass performed?
Vascular bypass is an effective way to restore blood flow after advanced forms of varicose veins. If you have already been diagnosed with a severe form of varicose veins or you want to undergo vein diagnostics, then make an appointment at the Phlebological Center named after. Pirogov. Our doctors will help you restore blood circulation in the veins of your legs.
We are located at the address: Moscow, Gagarinsky Lane, 37/8 (metro station “Smolenskaya”, Arbatsko-Pokrovskaya line, metro station “Kropotkinskaya”).
We are open for you from Monday to Friday from 8:00 to 21:00, Saturday and Sunday from 9:00 to 18:00. Call +7.
Back to articles
Treatment
An important point is to eliminate etiological factors - smoking, hypothermia, etc.
Complex therapy includes antispasmodics (No-spa 2t x 3 times a day or Halidor 200 mg x 2 times a day), desensitizing drugs - for example, Claritin 1t x 1 time a day.
Otherwise, conservative therapy for the disease is practically no different from that for obliterating atherosclerosis. Course treatment should be carried out at least 2 times a year.
For obliterating endarteritis, lumbar sympathectomy is more widely used, which is currently performed using minimally invasive methods. Carrying out reconstructive operations on blood vessels, as a rule, is not possible due to diffuse damage to the arterial bed.
The possibilities of physiotherapy are wider - UHF therapy, Bernard currents, electrophoresis.
Sanatorium-resort treatment is indicated in the form of radon and hydrogen sulfide baths.
Aneurysms
Aneurysms of peripheral arteries are characterized by the appearance of pathologically dilated areas of the arterial wall, resulting from its weakening. As a result, the artery wall bulges and this condition can be complicated by thromboembolism, strokes, or, if the arterial wall is significantly thinned, ruptures.
About 70% of such aneurysms occur in the popliteal arteries, and 20% in the iliofemoral segment. Sometimes they are combined with abdominal aortic aneurysms, which in 50% of cases are bilateral. Typically, aneurysms of peripheral arteries are provoked by atherosclerosis and infectious diseases (in such cases, the protrusion is most often localized in the femoral artery). Sometimes the root cause of their occurrence is entrapment of the popliteal artery or septic emboli, leading to the formation of a mycotic aneurysm.
Peripheral aneurysms are often asymptomatic. In some cases they are manifested by the following symptoms:
- pain when palpating;
- pallor and coldness of the affected limb;
- sensitivity disorders;
- absence of pulse in the affected area due to thromboembolism or rupture of a pathological protrusion;
- pain, fever, general malaise (if the aneurysms are infectious).
The risk of artery rupture in the area of the aneurysm is low - no more than 5% for popliteal bulges and 1 - 14% for iliofemoral aneurysms.
Thromboangiitis obliterans (Buerger's disease)
The disease is quite rare. The course and clinical manifestations are similar to obliterating endarteritis, but differ in a more aggressive course. One of the main symptoms that distinguishes Buerger's disease from other obliterating diseases of the extremities is migrating thrombophlebitis, mainly of the superficial veins. The disease is characterized by a chronic course with periodic exacerbations and remissions.
Treatment of thromboangiitis obliterans is not much different from therapy for endarteritis obliterans. If venous thrombosis occurs, they are treated according to the general rules (see treatment of venous thrombosis).