Blockage of arteries in the vertebrobasilar region leads to the development of ischemic stroke with localization of the infarction zone in various parts of the brain stem, thalamus, occipital lobes and cerebellum. Individual characteristics of the location of the arteries and the variety of pathogenetic mechanisms very often determine the individual characteristics of the neurological clinic in acute ischemic strokes in this area. Along with the presence of typical neurological syndromes, doctors at the Yusupov Hospital often note atypical symptoms of acute cerebrovascular accident. In this clinical situation, they use brain neuroimaging methods that help confirm the diagnosis (computed tomography and magnetic resonance imaging).
Neurologists at the Yusupov Hospital assess the degree of impairment of neurological functions during patient hospitalization, during treatment and at the end of therapy. All patients admitted to the neurology clinic undergo the following examinations:
- Doppler ultrasound of the great vessels of the head in the extracranial region;
- transcranial Doppler sonography;
- duplex scanning.
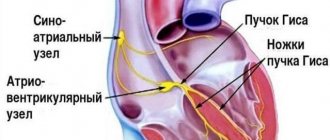
A 12-electrode ECG is also performed, blood pressure is monitored, and the volumetric maximum blood flow through the internal carotid and vertebral arteries is determined. Spiral computed tomography of the brain at the Yusupov Hospital is performed in all cases immediately upon admission of patients to the hospital. In the presence of several foci of cerebral infarction, neurologists use a more sensitive neuroimaging technique - diffusion-weighted magnetic resonance imaging.
A modern sensitive technique for neuroimaging of the brain - perfusion-weighted magnetic resonance imaging - allows doctors at the Yusupov Hospital to obtain information about the state of blood supply to brain tissue, and identifies blood supply disturbances both in the ischemic core zone and in surrounding areas.
general description
Vertebrobasilar insufficiency
is a condition in which there is a decrease in blood supply in the arterial system: basilar and vertebral. As a result of this condition, the nutrition and functions of the brain are disrupted, resulting in irreversible morphological changes in the brain matter.
According to statistical literature, people with vertebrobasilar insufficiency are most often susceptible to strokes in about 25-30% and transient cerebrovascular accidents in 65-70%.
Vertebrobasilar insufficiency (Vertebrobasilar arterial system syndrome)
Acute VBI
Clinical manifestations of acute vertebrobasilar insufficiency are very polymorphic.
The degree of their severity is determined by the etiopathogenesis, strength and duration of the pathological effect. In the acute form, the neurological deficit is short-term and completely reversible - all symptoms disappear within 24 hours. It is characterized by rapid development, when less than 2 minutes pass from the beginning to the most pronounced picture. Vestibular disorders occupy a central place in the clinical picture of transient neurological disorders. Paroxysms of systemic dizziness often occur, lasting from several minutes to several hours. Other symptoms include imbalance, small-scale nystagmus, nausea and vomiting. The picture is complemented by cerebellar syndrome, characterized by intention tremor and adiadochokinesis.
Visual and oculomotor disturbances are common - deterioration of visual acuity, photopsia, hemianopsia. Transient motor deficit (weakness, paresis or paralysis) is combined with numbness of the face and limbs. During examination, elements of alternating syndromes (Weber, Millard-Gübler, Wallenberg-Zakharchenko) may be revealed. Sometimes cerebral damage occurs as lacunar strokes with isolated hemiparesis, hemihypesthesia, and hemiataxia.
Chronic VBI
Chronic forms of vertebrobasilar insufficiency are permanent, rarely influenced by provoking factors, and their symptoms persist between ischemic attacks. Discirculatory encephalopathy is manifested by non-systemic dizziness without vestibular disorders, moderate cerebellar ataxia, and periodic headaches in the cervical-occipital region. The picture is complemented by tinnitus with gradual weakening of hearing, pyramidal insufficiency. Cognitive, psychoemotional, and autonomic disorders are noted.
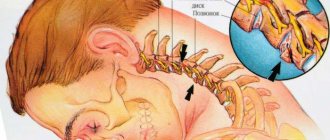
Spondylogenic VBI
Vertebrogenic disorders are considered as part of the clinical picture of vertebral artery syndrome. Symptoms occur suddenly, with sudden movements of the head (hyperextension, turns to the healthy side, lateral bends), and clearly depend on the position of the cervical spine. Typical signs are syncope or falls without loss of consciousness (drop attacks), cerebellar syndrome with statolocomotor ataxia.
Patients report dizziness, noise in the ear, and unilateral hearing loss. Transient visual disturbances are represented by a feeling of “sand” or “veil” before the eyes, photopsia. Cephalgia is hemicranial in nature, spreading from the cervical-occipital to the frontotemporal-orbital region. With cervicogenic syndromes, pain radiates to the shoulder and arm. Local vegetative reactions (pallor, marbling, dryness or hyperhidrosis) are visible on the skin of the cervical region.
Symptoms of ischemic stroke in the vertebrobasilar region
Lacunar strokes in the vertebrobasilar region occur as a result of damage to a separate paramedian branch of the vertebral artery, common artery or branch of the posterior cerebral artery against the background of arterial hypertension, which is often combined with high levels of lipids in the blood or diabetes mellitus. The disease begins suddenly and is accompanied by dizziness, nausea, and vomiting. There are disturbances in motor function caused by damage to the motor pathways in the area of the base of the bridge, which are supplied with blood by small arteries branching from the main artery:
- incomplete paralysis of facial muscles;
- arm paralysis;
- impaired movement of the arm and leg on one side of the body.
Lacunar infarctions in the thalamus cause the development of a purely sensory syndrome, the cause of which is damage to the lateral parts of the thalamus due to blockage of the thalamogenicular artery. Complete hemisensory syndrome is manifested by a decrease in superficial or deep sensitivity, or numbness of the skin of one half of the body. Some patients have unilateral decrease in sensitivity of the corner of the mouth, palm and foot.
When ischemia spreads towards the internal capsule, a sensorimotor stroke develops. It is manifested by motor impairments, which are preceded by sensory disorders. If the lacunae are located in the area of the bridge, doctors at the Yusupov Hospital determine the following signs of ischemic stroke:
- impaired coordination of movements on one half of the body;
- moderate leg weakness;
- Mild paresis of the arm.
Nonlacunar ischemic infarction in the vertebrobasilar region develops as a result of damage to the short or long circumflex branches of the vertebral or basilar arteries and is manifested by the following symptoms:
- systemic dizziness;
- headache;
- hearing loss with noise in the same ear;
- motor and cerebellar disorders;
- sensory disturbances in one or both limbs of one side of the body.
Blockage of the posterior inferior cerebellar artery is manifested by the following symptoms:
- systemic dizziness;
- nausea;
- vomit;
- swallowing disorder;
- speech and hearing impairment;
- sensitivity disorders on the face of a segmental type;
- cerebellar ataxia (impaired stability) on the side of the ischemic lesion;
- movement disorders, decreased pain and temperature sensitivity on the limbs and torso on the opposite side.
When the branches of the main artery supplying the midbrain are blocked, paresis of the muscles innervated by the oculomotor nerve occurs on the side of the lesion and paralysis of the limbs on the opposite side. With a heart attack in the quadrigeminal artery basin, upward gaze paralysis and convergence insufficiency develop, which is combined with involuntary high-frequency oscillatory eye movements.
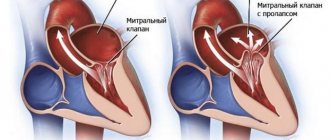
Cerebellar infarction in most cases occurs due to cardiac or arterial embolism of the anterior inferior cerebellar artery or superior cerebellar artery.
Blockage of the vertebral artery can occur both inside and outside the skull. When the extracranial section is blocked, the following symptoms are noted:
- short-term loss of consciousness;
- systemic dizziness;
- visual impairment;
- oculomotor and vestibular disorders;
- violations of statics and coordination of movements.
Often, patients suddenly fall, their muscle tone is impaired, autonomic disorders develop, breathing and cardiac activity are impaired.
Diagnosis and treatment of patients diagnosed with vertebrobasilar insufficiency
V.A. PARFENOV
,
L.M.
ANTONENKO ,
First Moscow State Medical University named after.
THEM. Sechenov, Department of Nervous Diseases The article describes modern approaches to the diagnosis and treatment of the most common causes of dizziness - vertebrobasilar insufficiency, benign paroxysmal positional vertigo, phobic postural vertigo.
One of the most common diagnoses in outpatient neurological practice in our country is vertebrobasilar insufficiency (VBI). A number of studies have shown that in a large percentage of cases, when conducting a specialized examination in patients diagnosed with VBI, completely different causes are revealed that explain the existing neurological disorders [4, 6, 8, 25]. Previous studies at our department showed that among patients sent to the hospital due to intense isolated dizziness, patients with benign paroxysmal positional vertigo, vestibular neuronitis, Meniere's syndrome or disease predominated [7, 8].
VBI is a reversible disorder of brain function caused by a decrease in blood supply to the area supplied by the vertebral and basilar arteries. The pathogenetic basis of this condition is cerebrovascular pathology, manifested by transient ischemic attacks or small strokes in the vertebrobasilar arterial system, although a gradual increase in neurological deficit is possible [3]. The vascular nature of VBI is also reflected in the International Classification of Diseases, X Revision, where VBN is classified as “vertebrobasilar arterial system syndrome” (G45) and belongs to class V (“Vascular diseases of the nervous system”).
To better understand the processes occurring when the vertebrobasilar arterial system is damaged, one should dwell on the anatomical features of the structure of this vascular system. The vertebral artery (VA), steam room, on the right departs from the innominate artery, on the left - directly from the subclavian artery. There are four anatomical segments of the VA. The interval from the origin of the artery from the innominate (right) or subclavian (left) arteries to its entry into the openings of the transverse processes of the C5 or C6 vertebrae is called the first segment. The second segment makes up the section of the VA, where it passes through the openings of the transverse processes of the C6-C2 vertebrae. The third segment is the distance over which the VA bends around the arch of the atlas and pierces the dura mater at the level of the foramen magnum. The last, fourth segment begins from the point of perforation of the VA of the dura mater and continues to the border between the pons and the medulla oblongata, where the right and left vertebral arteries merge and the basilar artery is formed. The basilar artery divides into two posterior cerebral arteries. From these large arteries branch circumflex branches and small penetrating arteries, which pass into the deep parts of the brain. The first and fourth segments of the vertebral arteries are most susceptible to atherothrombotic damage. Cerebral atherosclerosis is the most common cause of stenotic lesions of the extracranial part of the vertebral arteries, the predisposing factors for the occurrence of which are developmental anomalies: hypo- or aplasia, pathological tortuosity of the vertebral arteries [10, 11]. This pathology can lead to the development of VBI. Much less often, VBI is caused by a violation of the patency of the basilar artery or small arteries of the brain stem and cerebellum [10, 11]. A dangerous complication of atherosclerotic stenosis of the vertebral and (or) basilar artery is increasing thrombosis of these arteries. Clinically, it can manifest itself as repeated transient ischemic attacks in the vertebrobasilar system, and in severe cases develop into a brainstem stroke. Studies have shown that 43% of infarctions in the vertebrobasilar system occurred via an arteriothrombotic mechanism [21]. Small arterio-arterial emboli caused by the disintegration of an atherosclerotic plaque or mural thrombus are the cause of transient ischemic attacks in the vertebrobasilar system in approximately 20% of cases [21].
Microangiopathy of the arteries of the vertebrobasilar system can also cause VBI. The main etiological factors in the development of cerebral microangiopathy are arterial hypertension and diabetes mellitus [1, 6, 12].
The diversity of the clinical picture of VBI is due to the fact that the blood supply to the vertebrobasilar system includes various parts of the central nervous system: the cervical spinal cord, medulla oblongata, pons, midbrain, cerebellum, part of the thalamus and hypothalamic region, occipital lobe, posterior and mediobasal sections of the temporal lobes brain.
In most cases, VBI manifests itself only as transient ischemic attacks, which are an acute short-term disorder of the blood supply to the brain that does not lead to persistent changes in the brain matter, with complete regression of the neurological deficit within 24 hours. The clinical picture of VBI can consist of a various combination of motor disorders in the form weakness in the limbs of varying severity, sensory disorders: hypoesthesia or paresthesia of the limbs, face, often bilateral, homonymous hemianopia or cortical blindness, imbalance, attacks of dizziness. The isolated occurrence of one of the described neurological syndromes cannot be considered as a manifestation of a transient ischemic attack [21, 22].
Dizziness and imbalance are the most common reasons for overdiagnosis of VBI. Often, “vertebrobasilar insufficiency” and “hypertensive cerebral crisis” hide a variety of disorders, often having nothing to do with the pathology of the vascular system of the brain [1, 2, 4, 6, 9].
The complaint of dizziness is one of the most common reasons for visiting an outpatient doctor after a headache [18]. The causes of dizziness, along with VBI, can be a wide variety of pathological processes: diseases of the cochleo-vestibular apparatus, psychogenic disorders, degenerative diseases of the central nervous system (CNS).
In medical practice, dizziness is a condition in which the patient has a sensation of rotation of surrounding objects or the illusion of his own rotation or movement [10, 18]. Patients use this term to refer to a number of other symptoms, many of which do not fit this definition at all: a feeling of lightness in the head, weakness, blurred vision, blurred vision, “wooliness” in the legs, darkening in the eyes after a sharp rise to one’s feet from sitting or lying position. Therefore, taking an anamnesis is of great importance to identify the cause of dizziness. The doctor must first find out what exactly the patient calls dizziness. To do this, you can ask the patient to describe his complaints without using the word dizziness. A description of a feeling of instability, aggravated in the dark, a feeling of a “cushion” under the feet when walking is a sign of sensory ataxia with damage to peripheral nerves and conductors of deep sensitivity of the central nervous system. A complaint of darkening of the eyes with a sharp transition to a vertical position indicates dysfunction of the autonomic nervous system. The feeling of weakness, blurred vision, and blurred vision described by the patient in the absence of objective signs of damage to the nervous system during a neurological examination can most often be a sign of chronic fatigue, anemia, or hypovitaminosis. If the patient describes the sensation of rotation of surrounding objects or his own body, then this most often indicates the interest of the vestibular analyzer. To carry out a differential diagnosis, the most important parameters are the following: the nature and duration of dizziness, the provoking factor, and accompanying symptoms.
To clarify the nature of dizziness, you can ask the patient to draw an analogy and describe what the dizziness he is experiencing is like. For example, attacks of intense dizziness with a sensation of objects spinning, as when riding on a merry-go-round, may be a sign of vestibular neuronitis; the illusion of the floor swaying, like the deck of a ship, when walking, most often may indicate psychogenic dizziness.
The duration of attacks of dizziness can be short-term: from several seconds to several minutes, which is typical, for example, for vestibular paroxysm. Dizziness lasting from 5 to 20 minutes in combination with other neurological syndromes described above may be a sign of a transient ischemic attack. An attack of dizziness that lasts for several days may be a sign of vestibular neuronitis [10, 18].
When talking with the patient, it is necessary to find out what factors provoke dizziness. For example, dizziness that occurs while lying down when turning in bed is most typical for benign paroxysmal positional vertigo; if an attack of dizziness is provoked by coughing, straining, loud sounds, then this allows us to suspect a perilymphatic fistula in the patient. When the patient points to a certain environment that provokes dizziness and instability, for example on a street with many people, in the subway, this may be a sign of phobic postural vertigo [10, 18, 20].
It is very important to make a correct diagnosis by identifying the symptoms that accompany an attack of dizziness. Acute dizziness and decreased hearing in one ear allows one to suspect labyrinthine infarction (anterior inferior cerebellar artery syndrome) [4, 8]. Attacks of dizziness accompanied by subacute hearing loss in one ear and paresis of facial muscles on this side are often a manifestation of a tumor of the cerebellopontine angle [18]. If it is indicated that before repeated attacks of dizziness the patient experiences increasing noise in the ear, a feeling of fullness, or decreased hearing in this ear, a diagnostic search for Meniere’s syndrome and/or disease should be carried out [18].
The most difficult to diagnose cause of dizziness caused by vascular lesions of the brain in the vertebrobasilar region is isolated dizziness. According to a study, about 0.7% of cases of isolated vestibular vertigo were caused by stroke [4, 8]. Other variants of cerebral infarction in the vertebrobasilar region, accompanied by dizziness, are combined with damage to the structures of the brain stem and manifest themselves with symptoms of focal brain damage. The pathomorphological basis of isolated vertigo caused by stroke is a selective lesion of the cerebellar nodule or part of the brain stem in the area of entry of the vestibular nerve root. These structures are located in the area of the blood supply of the medial branch of the posterior inferior cerebellar artery. With this pathology, patients complain of acute rotational dizziness lasting up to several hours, often accompanied by nausea and vomiting, which is also characteristic of diseases of the peripheral vestibular system. A differential diagnosis should be made primarily with vestibular neuronitis [4, 8]. A patient's history of persistent arterial hypertension, atrial fibrillation, stenotic atherosclerosis of the cerebral arteries, a previous stroke, or a history of repeated transient ischemic attacks can suggest a vascular cause of isolated dizziness. To diagnose these disorders, an important role is played by a thorough history taking into account vascular risk factors, neurovestibular examination and magnetic resonance imaging of the brain, which reveals focal ischemic brain damage in the area of the cerebellar nodule or the area of the brain stem at the entry site of the vestibular nerve root [ 4, 8]. Patients with cerebral atherosclerosis and hypertensive angiopathy of the cerebral arteries in the vertebrobasilar system often complain of dizziness [11, 13, 22]. Upon closer questioning, it is possible to find out that when patients complain of dizziness, they mean a feeling of instability, staggering when walking, which intensifies when turning or bending. In older patients, instability may be accompanied by falls. These disorders in most cases are caused by damage to the frontal-subcortical-stem-cerebellar connections due to silent lacunar strokes or leukoaraiosis [3]. A neurological examination of these patients often reveals scattered focal neurological symptoms: reflexes of oral automatism, anisoreflexia, dysdiadochokinesis, intention when performing pointing tests. When examining the function of the vestibular analyzer, minor deviations from the norm may be detected in the form of disturbances in smooth pursuit eye movements and visual saccades [4]. In patients with vascular dementia, the phenomenon of frontal-subcortical dysbasia occurs, which is a higher-level gait disorder and is associated with a violation of frontal-subcortical-brain-stem interactions [3]. Studies have shown that stability disorders associated with a violation of the highest level of movement regulation occur in 40% of this category of patients [13].
It is necessary to dwell in more detail on the differential diagnosis of VBI with diseases that, according to various studies, are the most common reason for seeking neurological help in patients complaining of dizziness. These include benign paroxysmal positional vertigo (BPPV) - found in 18.3% of patients - and phobic postural vertigo, found in 15.9% of cases [10, 18].
BPPV is one of the most common forms of peripheral vestibular vertigo [10, 14, 15, 25]. The main clinical sign of BPPV is attacks of rotational dizziness lasting up to several minutes, in most cases accompanied by nausea, often vomiting, that occur when the position of the head changes. The most typical occurrence of dizziness is when the patient turns in bed from side to side, sits down after sleep, bends over or throws his head back. Sometimes the patient may wake up at night with a feeling of dizziness and nausea. The most severe attacks of dizziness occur when you first change your body position after sleep. With repeated movements the dizziness weakens. This is one of those diseases in which the complaints are so characteristic that a diagnosis can be made after collecting an anamnesis, and quite often the patient even indicates the side of the lesion. BPPV most often occurs in people aged 50–70 years, although it can develop at any age; it occurs 2 times more often in women [16, 18].
The pathogenetic mechanisms of BPPV development are associated with irritation of vestibular apparatus receptors by otoliths (calcium carbonate crystals). Otoliths are separated from the otolithic membrane due to injury or degenerative processes. As a result, different impulses from the two labyrinths enter the brain stem, which leads to dizziness and nystagmus. Given the proximity of the autonomic nuclei, an attack of dizziness with BPPV is almost always accompanied by autonomic reactions: nausea, vomiting, and increased blood pressure. Therefore, patients suffering from arterial hypertension often regard an attack of dizziness with a rise in blood pressure as a manifestation of a hypertensive crisis and turn to a therapist to correct antihypertensive therapy. The clinical picture of BPPV has characteristic features. Attacks of rotational vertigo occur suddenly when the patient's position changes. One of the most common onset of the disease is the occurrence of dizziness when turning in bed at night or in the morning after waking up. An attack of dizziness lasts no more than a minute, but is usually very severe and is often accompanied by nausea and vomiting. When trying to stand up, instability occurs; in severe cases, the patient cannot move without assistance or additional support. A characteristic clinical sign of a BPPV attack is positional horizontal rotatory nystagmus. It has a latent period of 1-5 s, initially increases, lasts about 10 s, and then gradually subsides. The direction of nystagmus is determined by which semicircular canal is affected. Often, an attack of dizziness with BPPV can occur when throwing the head back or bending down. Moreover, if a person is standing, a fall may occur due to loss of balance. Falls during an attack of BPPV occur more often in elderly and senile people. The average duration of the disease is about 2 weeks. [10, 18]. Diagnosis of BPPV is based on characteristic complaints, history and clinical picture of the disease. The diagnosis of BPPV is confirmed by the occurrence of a typical episode of dizziness with peripheral positional nystagmus in the patient during provocative tests. The most commonly used test is the Dix-Hallpike test to diagnose otolithiasis of the posterior semicircular canal, and the McClure-Pagnini test to identify lesions of the horizontal semicircular canal [10, 17-19].
The second most common reason for patients complaining of dizziness after BPPV is psychogenic dizziness [18, 20]. Psychogenic dizziness can be primary when it develops independently, and even with a careful history and examination, it is not possible to identify signs of damage to the vestibular system [10, 18, 19]. Often the cause of psychogenic dizziness is an episode of true vestibular dizziness with a disturbance in orientation in space, a pronounced autonomic reaction, a feeling of anxiety, fear, for example, vestibular neuronitis, an attack of BPPV [10, 24]. Phobic postural dizziness is a variant of psychogenic dizziness, in which the complaint of dizziness is the main and almost the only one [10, 24]. Often these patients note poor tolerance to transport, swings, and carousels since childhood, which some authors regard as existing minimal dysfunction of the vestibular system, which can cause a feeling of instability [10]. When asked to describe their complaints without using the word dizziness, patients often characterize their sensations as a feeling of derealization, instability, swaying as if on a deck, fear of falling. Provoking factors may be: crowded places or, conversely, an empty room; staying on the bridge; car driving; stressful situations. Upon questioning, it can be revealed that during or immediately after attacks, anxiety and autonomic disturbances (palpitations, nausea, sweating, irregular breathing) are observed. Often, patients suffering from phobic postural dizziness have a tendency to obsessive states and anxiety and depressive disorders. Diagnosis of phobic postural dizziness is based on a characteristic combination of complaints of dizziness and balance disorder, which occurs in attacks while standing or while walking, can be provoked by a certain environment, and is often accompanied by anxiety in the absence of objective signs of vestibular disorders. However, when making this diagnosis, the doctor must be very careful, it is necessary to exclude the organic origin of dizziness, conduct a thorough clinical examination of the balance system, vestibulometry and stabilography. Long-term, undiagnosed vestibular disorders can lead to the development of anxiety disorders and/or depression [24]. The absence of a provoking factor or anxiety should also make the doctor doubt the psychogenic nature of the disease.
Treatment of VBI is a complex multi-level task. It includes the treatment of hypertension, atherosclerosis, cardiac pathology, disorders of the blood coagulation system, which are the cause of the development of transient ischemic attacks, infarctions in the vertebrobasilar system. In patients who have suffered a transient ischemic attack or stroke, it is necessary to carry out long-term prevention of recurrent stroke, including taking antiplatelet or anticoagulants, antihypertensive drugs and lipid-lowering drugs.
To improve cerebral blood flow and brain metabolism, it is advisable to conduct courses of vascular and nootropic drugs.
In order to improve vestibular compensation, it is recommended to combine drug therapy with vestibular rehabilitation [23]. Modern hardware rehabilitation methods have shown high efficiency, including rehabilitation on a stabilographic platform with biofeedback [5].
Thus, VBN is a vascular disease of the brain, the diagnosis of which requires a careful collection of anamnesis, clarification of the nature of the patient’s dizziness, duration, frequency, provoking factors for the attack of dizziness and accompanying symptoms. A well-collected anamnesis and assessment of the function of the vestibular analyzer using a neurovestibular examination in most cases allow one to avoid diagnostic errors. The most effective treatment for VBI is a combination of drug therapy and vestibular rehabilitation.
Literature
1. Abdulina O.V., Parfenov V.L. Vestibular dizziness in emergency neurology. Clinical Gerontology, 2005, 11: 15-18. 2. Weiss G. Dizziness. Neurology. Ed. M. Samuels. M.: Praktika, 1997. P. 9-120. 3. Gusev E.I., Nikiforov A.S., Burd G.S. Main neurological syndromes and symptoms. M., 2001. 4. Zamergrad M.V. Dizziness: the role of vascular factors. Effective pharmacotherapy. Neurology and Psychiatry, 2013, 4(45): 4-5. 5. Zinovieva G.A. Impaired stability of vertical posture in elderly patients and their correction using biofeedback using a stabilogram. Author's abstract. diss. Ph.D. M., 2001. 6. Parfenov V.A. Differential diagnosis and treatment of dizziness in patients with arterial hypertension. Therapeutic Archives, 2005, 1: 56-58. 7. Parfenov V.A., Abdulina O.V., Zamergrad M.V. Differential diagnosis, prognosis and treatment of acute vestibular vertigo. Neurological Journal, 2007, 6: 21-25. 8. Parfenov V.A., Abdulina O.V., Zamergrad M.V. Peripheral vestibulopathy under the guise of a stroke. Neurological Journal, 2005, 6: 28-32. 9. Parfenov V.A., Zamergrad M.V. What is hidden behind the diagnosis of hypertensive cerebral crisis. Neurological Journal, 1998, 5: 29-33. 10. Parfenov V.A., Zamergrad M.V., Melnikov O.A. Dizziness diagnosis, treatment, common diagnostic errors. Textbook allowance. M.: Publishing House “Medical Information Agency”, 2011. 11. Suslina Z.A., Varakin Yu.Ya., Vereshchagin N.V. Vascular diseases of the brain. M., 2006. 12. Shevchenko O.P., Praskurnichy E.A., Yakhno N.N., Parfenov V.A. Arterial hypertension and cerebral stroke. M., 2001. 13. Shtulman D.R. Dizziness and imbalance. In the book: Diseases of the nervous system. Ed. N.N. Yakhno. M., 2005. pp. 125-130. 14. Brandt T, Huppert I, Hecht J et al. Benign paroxysmal positioning vertigo: a long-term follow-up (6-17 years) of 125 patients. ActaOtolaryngol., 2006, 126(2): 160-163. 15. Brandt T, Huppert T, Nifner K et al. Long-term course and relapses of vestibular and balance disorders. Restor. Neurol. Neurosci., 2010, 28(1): 69-82. 16. Brandt T. Vertigo. Its Multisensory Syndromes. London: Springer, 2000. 17. Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Arch. Otolaryngol., 1980, 106: 484-485. 18. Brandt T, Dieterich M. Vertigo and dizziness: common complains. London: Springer, 2004. 19. Brandt T, Huppert D, Hecht J et al. Benign paroxysmal positional vertigo: A long-term follow-up (6-17 years) of 125 patients. ActaOtolaryngol., 2006, 126: 160-163. 20. Bronstein AM, Gresty MA et al. Phobic postural vertigo. Neurology, 1997, 46: 1480-1481. 21. Сaplan LR. Vertebrobasilar occlussion disease: riviewof selected aspects. Cerebrovascular disease, 1992, 2: 320-326. 22. Caplan LR. Posterior circulation ischemia: then, now, and tomorrow. The Thomas Willis Lecture. Stroke, 2000, 31: 2011-2023. 23. Cass SP, Borello-France D, Furman JM. Functional out¬come of vestibular rehabilitation in patients with ab¬normal sensory-organization testing. Am. J. Otol., 1996, 17: 581-94. 24. Huppert D, Kunihiro T, Brandt T. Phobic postural vertigo (154 patients) its association with vestibular disorders. J Audio Med 1995, 4: 97-103. 25. Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol., 2007, 20: 40-46.
Source:
Medical Council, No. 17, 2014
Types of ischemic strokes in the vertebrobasilar region
The following ischemic cerebral infarctions in the vertebrobasilar region are distinguished:
- lacunar strokes due to damage to small perforating arteries, caused by microangiopathies against the background of arterial hypertension and diabetes mellitus;
- non-lacunar strokes that developed due to damage to the short or long circumflex branches of the vertebral and basilar arteries in the presence of sources of cardioembolism and the absence of narrowing of the large vertebrobasilar arteries;
- non-lacunar strokes due to blockage of the vertebral and basilar arteries in the intracranial and extracranial parts, caused by their damage.
They have different symptoms and require differentiated therapy.
Treatment of ischemic stroke in the vertebrobasilar region
Neurologists at the Yusupov Hospital take an individual approach to the treatment of each patient diagnosed with ischemic stroke of the basilar artery. In the presence of high blood pressure, antihypertensive therapy is carried out. To stimulate spontaneous formation of channels in a blocked artery and prevent re-embolization in atherothrombotic and cardioembolic subtypes of nonlacunar ischemic infarction, direct anticoagulants, as well as antiplatelet agents, are used.
Complex therapy of acute ischemic strokes in the vertebrobasilar region also involves the prior use of neuroprotectors. In order to determine the feasibility of neuroprotective therapy, doctors at the Yusupov Hospital use diffusion-perfusion MRI studies, which help identify viable areas of the ischemic penumbra. After this, neuroprotective drugs are prescribed.
The Neurology Clinic of the Yusupov Hospital is equipped with the necessary equipment to diagnose complex locations of cerebral infarction. Neurologists treat patients with modern medications that have a pronounced effect on blockage of the vertebrobasilar artery. Call and they will make an appointment with a neurologist.