Chronic cerebrovascular accident (cerebral vascular insufficiency) is characterized by a decrease in blood supply to the brain. This condition is very common among older people in developed countries due to the high prevalence of atherosclerosis. In most cases, the carotid artery is damaged. A pair of carotid arteries, one on each side of the neck, running parallel to the jugular vein, are the main arteries that supply blood to the brain.
As a rule, cerebral vascular insufficiency develops in the area of the bifurcation of the carotid artery - the splitting of the carotid artery into internal and external branches. This splitting is similar to a stream that has split into two streams. In bifurcation, as well as during bifurcation in a water flow, accumulation of slag occurs. Severe symptoms begin to appear in most cases only when the artery blockage reaches 90 percent. This situation is similar to what happens with coronary heart disease.
Symptoms of chronic cerebrovascular accident are caused by decreased blood flow and oxygen supply to the brain. Stopping the flow of blood and oxygen leads to a stroke. The official definition of stroke is "loss of nerve function for at least 24 hours due to lack of oxygen." Some strokes are mild; others result in paralysis, coma, or speech impairment, depending on what part of the brain is involved. Mini-strokes, or transient ischemic attacks, can result in loss of nerve function for an hour or more, but less than 24 hours. TIAs can lead to transient symptoms of cerebral vascular insufficiency: dizziness, ringing in the ears, blurred vision, confusion, and so on.
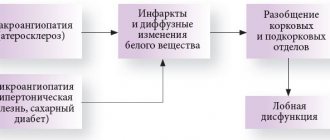
Atherosclerosis is one of the main causes of cerebrovascular insufficiency. As this process progresses, high cholesterol levels combined with inflammation in the walls of the arteries in the brain can cause cholesterol to accumulate on the vessel wall in the form of a thick, waxy plaque. This plaque can restrict or completely prevent blood flow to the brain, causing stroke, transient ischemic attacks, or dementia, which can lead to a variety of other health complications.
The most common forms of cerebrovascular disease of the brain are thrombosis (40% of cases) and cerebral embolism (30%), followed by cerebral hemorrhages (20%).
Another form of cerebrovascular disease includes aneurysms. In women with defective collagen, weak key arterial branch points result in ridges with a very thin endothelial covering that can easily rupture with minimal increase in blood pressure. It can also occur with poor capillaries caused by cholesterol deposition in tissues, especially in hypertensive patients with or without dyslipidemia. If bleeding occurs, the result is a hemorrhagic stroke in the form of subarachnoid hemorrhage, intracerebral hemorrhage, or both.
A drop in blood pressure during sleep can lead to a marked decrease in blood flow in narrowed blood vessels, causing ischemic stroke in the morning. Conversely, a sharp increase in blood pressure due to daytime agitation can lead to rupture of blood vessels, resulting in intracranial hemorrhage. Cerebrovascular disease primarily affects people who are elderly or have a history of diabetes, smoking, or coronary heart disease.
Symptoms
Symptoms of a cerebrovascular accident depend on the degree of damage to brain cells and the location of the area of the brain with impaired blood flow. In acute cerebrovascular accidents (hemorrhagic or ischemic stroke), movement disorders such as hemiplegia or hemiparesis develop.
In chronic cerebral circulatory disorders (also called discirculatory encephalopathy), symptoms develop gradually and are manifested by symptoms such as memory impairment, dizziness, headaches. At first, the patient does not have any impairment of intellectual abilities. But as there is a chronic lack of oxygen in the brain tissue, memory impairment begins to progress, personality disorders arise, and intelligence decreases significantly. Subsequently, the patient develops severe intellectual-mnestic and cognitive impairments and dementia develops; extrapyramidal disorders and cerebellar ataxia may also develop.
Transient cerebrovascular accident
Typically sudden and acute development. General cerebral symptoms of PNMK are headache, weakness, nausea (maybe vomiting), blurred vision, vegetative-vascular reactions (hot flashes, trembling, sweating, etc.), short-term disturbances of consciousness. Focal symptoms depend entirely on the topic of the ischemic process. On average, PNMK lasts from several minutes to several hours. Pathognomonic is the complete restoration of impaired neurological functions within 24 hours.
PNMK in the ICA (internal carotid artery) system is characterized by variable zones of hypoesthesia and/or paresthesia, covering individual areas of the skin of the extremities or face on the side opposite (heterolateral) to the ischemic focus. Central paresis may be observed, spreading to local muscle groups or one limb. Less common are hemihypesthesia and hemiparesis. Muscle strength is usually moderately reduced. Anisoreflexia is typical, sometimes pathological Rossolimo and Babinsky reflexes are present. Aphasia or dysarthria is often noted. There may be a decrease in visual acuity in one eye and the appearance of paroxysm of Jacksonian epilepsy, in some cases turning into a generalized seizure.
PNMK in the vertebrobasilar basin manifests itself with systemic dizziness with tinnitus, autonomic disorders, vestibular ataxia (discoordination of movements, unsteadiness of gait, instability in the Romberg position, etc.), visual disturbances in the form of metamorphopsia, photopsia, loss of visual fields. Horizontal nystagmus is noted. Dysarthria, dysphonia, diplopia, dysphagia, and the occurrence of alternating syndromes are possible. PNMK in the vertebrobasilar area is usually accompanied by a headache in the back of the head, the intensity of which is associated with head movements.
A transient disorder of cerebral circulation in the brain stem area is manifested by systemic dizziness, paresis of the extraocular muscles, hearing loss, and double vision. Transient disturbances in swallowing and articulation, hemianopia, and local hypoesthesia of the facial skin may appear. With PNMK in the region of the medulla oblongata (reticular formation, inferior olives), the so-called. drop attacks are transient paroxysms of immobility as a result of severe muscle weakness. With PNMK in the medial parts of the temporal lobe, short-term Korsakoff's syndrome is observed - loss of orientation in the environment and time, combined with a memory disorder about current events.
It should be noted that simultaneous stenosis of several arteries of the head is possible, leading to transient ischemia in several vascular territories. In such cases, the clinical picture of PNMK combines symptoms of damage to all cerebral areas involved in the ischemic process.
Causes
Chronic cerebral circulatory failure is most often associated with atherosclerosis, hypertension, and heart disease accompanied by chronic circulatory failure. In addition, CNMK may be associated with vascular anomalies and diseases (vasculitis), venous anomalies, diabetes mellitus and various blood diseases, which result in chronic cerebral hypoxia.
Also, chronic cerebrovascular accident occurs as a consequence of acute cerebral circulatory disorders such as ischemic or hemorrhagic stroke.
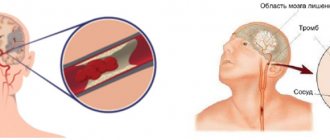
An ischemic stroke occurs when a blood vessel that supplies blood to the brain is blocked by a blood clot. A clot can form in an artery that is already narrowed. Also, a clot can break off from the wall of a vessel somewhere in the body and travel through the bloodstream to the brain.
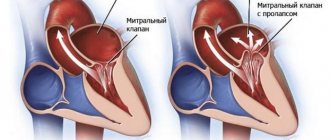
Ischemic strokes can also be caused by blood clots that form in the heart. These clots travel to the brain through the bloodstream and can become lodged in small arteries in the brain.
Certain medications and medical conditions can increase blood clotting and cause blood clot formation and increase the risk of ischemic stroke. A hemorrhagic stroke occurs when a blood vessel in a certain part of the brain becomes weak and ruptures, causing blood to leak into the brain and the blood damages brain cells. Some people have defects in the blood vessels in the brain that make a hemorrhagic stroke more likely.
Wait. Add the book to the cart.
The problem of damage to the venous system of the brain is a real “Cinderella” of modern angioneurology. The attention of researchers and practitioners is primarily drawn to the pathology of the arterial bed of the brain. Meanwhile, the venous system is important for the blood supply to the brain.
Prevention and treatment of venous encephalopathy is, first of all, the prevention and treatment of diseases that can complicate the characteristics of manifestations and the course of the pathological process. If the cause of venous circulation disorders in the brain is established, then treatment is aimed at eliminating it. For example, in case of heart failure, cardiac drugs are the main ones; when veins are compressed by a tumor, scar after injury or inflammation, which impede the outflow of blood from the cranial cavity, the issue of surgical intervention is decided.
Glivenol reduces congestion in the veins - the average daily dose is 0.6–1.2 g; aescusan - 250 mg tablets or oral solution, active ingredient - zecin; Troxevosin, Detrolex - 500 mg tablets; diosmin - 450 mg; hesperidin - 50 mg; Take 2 tablets per day, day and evening with meals. Improves blood supply to the brain, lowers venous pressure and cerebrospinal fluid pressure, reduces cerebral edema euphilin orally 0.1-0.2 g 2-3 times a day, intravenously 5-10 ml of a 2.4% solution in 10-20 ml 40 % glucose, intramuscularly 1–2 ml of 2.4% solution. Diuretics have a decongestant effect: diacarb, furosimide, mannitol (200–400 ml of a 15% solution intravenously in a stream, slowly or drip, used only in a hospital). Magnesia sulfate is also used (25% solution is administered intramuscularly or intravenously, 5–20 ml). Orally or parenterally B1, B6, B12, PP, etc. According to indications, tranquilizers, hypnotics and anticonvulsants are prescribed.
For severe signs of venous stasis and cerebral edema, as well as for cardiovascular failure with severe shortness of breath and cyanosis, bloodletting (300–400 ml) is recommended, including with the help of leeches (hirudotherapy). Maintaining hygiene is of great importance.
The choice of forms of work and physical activity depends on the underlying disease. Professions that require heavy physical stress, which may increase venous stagnation (loader, digger, etc.), as well as those associated with prolonged bending of the head or incorrect posture, are contraindicated. Do not work at heights, underground, or in high, low, or extreme temperatures.
If you have venous pathology of the brain, you should also not perform sports exercises, for example, on rings and others associated with great physical stress.
An increase in venous pressure in the cranial cavity can be promoted by prolonged reading, writing, drawing, performing minor instrumental work, as well as frequent strain associated with holding the breath. You need to take short breaks while working, during which, with your hands behind your head, take a few deep breaths. When writing, you should use an inclined desk-lectern to avoid slouching or bending your head.
It is preferable to live in a temperate climate, since patients do not tolerate temperature fluctuations well. Venous pressure may increase at high altitudes.
The patient should stay in the fresh air as long as possible, work and rest in a well-ventilated area. You need to sleep with a high pillow under your head. Sleep should be long enough, but not excessive. Daytime rest or sleep for 1–2 hours is recommended. During the day you need to sit with your head thrown back several times (5-6 minutes each). You need to rest in a half-sitting position. At the same time, your well-being improves, headaches go away even with obvious signs of venous stagnation.
Impetuous movements and sudden bends are harmful. Patients should walk at a moderate pace, monitor their breathing, and short breaks from work should be used for warm-up and breathing exercises.
Clothing should be loose and not tight around the neck. A tight collar can cause headaches, which disappear if you release its pressure. Do not tighten the belt too tightly, which also increases venous and internal pressure.
If you are prone to constipation, you need to follow a diet: food with limited liquid (3–4 glasses per day), salt (up to 5 g per day), carbohydrates and fats is recommended; food rich in proteins, vitamins, fiber (brown bread, vegetables and fruits). To prevent constipation, it is recommended to take laxatives.
If there are venous circulation disorders in the brain, smoking is strictly not recommended. Everyone knows the expression “smoker's cough.” In this case, venous pressure increases and signs of bettolepsy may occur. Moderation in sexual activity should be observed. Pregnant women with signs of severe venous congestion in the brain, if it is impossible to eliminate its cause, are advised to terminate the pregnancy or deliver by caesarean section. Childbirth represents excessive stress for them with a life-threatening increase in venous and internal pressure. Venous pressure often increases with negative emotions. Therefore, patients need a calm, friendly environment both at home and at work.
For venous cerebral insufficiency, systematic light breathing exercises have a beneficial effect: intensive inhalation through the nose and slow exhalation through the mouth. It should be noted that a rise in venous pressure may occur during a conversation. Older speakers who engage in extreme exertion are at risk of experiencing severe headaches, dizziness, and other brain symptoms. To be convinced of the significant impact of speakers' overstrain on the vessels, it is enough to observe their neck: the play of tension and collapse of the jugular veins, caused by fluctuations in intrathoracic pressure, is noticeable. Interrupting speech with frequent breaths can eliminate the increase in venous pressure.
Venous pressure is significantly reduced under the influence of a course of physical therapy, head and neck massage using the stroking method. Systematic air baths after morning sleep are useful. The naked patient walks around the room at a temperature of 21–22 °C for 10–15 minutes, after which he wipes himself with warm water (38–39 °C). In summer, air baths are taken outdoors in the morning, in the warmth. Patients with venous pathology of the brain are prescribed galvanic collars, warm seats and foot baths. If the state of health allows, then foot baths are carried out with the addition of hot water. Narzan, carbon dioxide and hydrogen sulfide baths are shown.
One of the important methods of combating venous encephalopathy is oxygen therapy, which normalizes vascular tone, improves overall well-being, and reduces headaches.
Sanatorium-resort treatment is recommended mainly in the middle zone. Staying in southern resorts during the hot season is contraindicated.
Diagnostics
The diagnosis of chronic cerebrovascular accident is made based on a combination of examination data, symptoms, neurological signs, results of brain neuroimaging (MRI, or MSCT), and angiography of cerebral vessels.
The doctor may detect the presence of certain neurological, motor, and sensory deficits, such as changes in vision or visual fields, abnormal reflexes, abnormal eye movements, muscle weakness, decreased sensation, and other changes. In addition, certain tests help determine the presence of intellectual-mnestic disorders.
Laboratory research methods are prescribed for the diagnosis of somatic diseases.
Synonyms:
- encephalopathy,
- chronic cerebral ischemia,
- slowly progressive cerebrovascular accident,
- chronic ischemic brain disease,
- cerebrovascular insufficiency,
- vascular encephalopathy,
- atherosclerotic encephalopathy,
- hypertensive encephalopathy,
- atherosclerotic angioencephalopathy,
- vascular (atherosclerotic) parkinsonism,
- vascular (late) epilepsy,
- vascular dementia.
The most widely used term in domestic neurological practice is “dyscirculatory encephalopathy ,” which retains its meaning to this day.
Treatment
If there are diseases such as hypertension, diabetes mellitus or other diseases, then, first of all, it is necessary to compensate for the underlying disease.
To treat chronic cerebrovascular accidents, various medications are used - vascular drugs (Trental, Cavinton, Sermion, etc.), nootropics, metabolic drugs, antioxidants. To prevent the formation of blood clots, antiplatelet agents such as aspirin, dipyridamole are prescribed. For high cholesterol levels in the blood Statins may be used.
Sometimes surgical treatment is required to eliminate the blood flow disorder - for example, carotid endarterectomy. Treatment methods such as carotid angioplasty and stenting are also used.