What are the features of the symptoms of this disease?
In the presence of an ischemic stroke in the territory of the right middle cerebral artery, it is possible to identify symptoms of lesions of the midbrain and cerebral hemisphere, depending on the location and conditions of collateral blood supply in the clinical pictures. Quite often you can find a combination of damage to the thalamus and the cerebral hemisphere or isolated infarctions of the thalamus. It should be noted that in most cases, the symptoms of the disease in patients can be combined. The most common symptoms include visual damage, neuropsychological damage, and hemiparesis.
Acute cerebrovascular accidents (ACI)
A stroke is an acute disorder of cerebral circulation, the symptoms of which persist for more than one day.
There are three types of stroke: ischemic stroke, hemorrhagic stroke and subarachnoid hemorrhage.
Ischemic stroke most often develops when the arteries, the vessels that carry blood to the brain, become narrowed or blocked. Brain cells die without receiving the oxygen and nutrients they need. This type of stroke is also called cerebral infarction, by analogy with myocardial infarction.
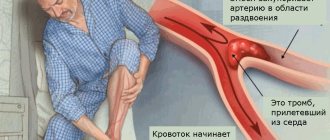
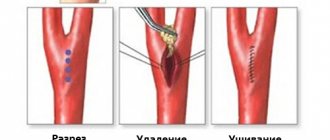
The reasons for blockage of a vessel can be different. The vessel can be closed by an embolus - a piece of intracardiac thrombus that occurs in certain heart diseases, or a piece of atherosclerotic plaque located on the wall of a large vessel. The cause of blockage of the vessel may be thrombosis - the formation of a blood clot (similar to the one that forms when the skin is cut with injury to the superficial vessels). A thrombus usually forms on the surface of an atherosclerotic plaque. Thrombosis is promoted by increased blood clotting and an increased ability for blood platelets (platelets) to stick together (aggregate).
With frequent increases in blood pressure, changes can develop in the walls of small vessels that supply deep structures of the brain. These changes lead to narrowing and often closure of these vessels. Sometimes, after another sharp rise in blood pressure (hypertensive crisis), a small infarction develops in the circulatory system of such a vessel (called a “lacunar” infarction in the scientific literature). Ischemic stroke occurs 4 times more often than the other type of stroke, hemorrhagic.
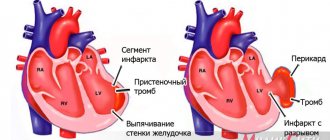
Hemorrhagic stroke most often develops when arteries rupture. The spilled blood soaks part of the brain, which is why this type of stroke is also called a cerebral hemorrhage. Most often, hemorrhagic stroke occurs in people suffering from arterial hypertension and develops against the background of increased blood pressure. At some point, the vascular wall cannot withstand the sharp rise in blood and ruptures. A more rare cause of hemorrhagic stroke is a ruptured aneurysm. An arterial aneurysm is usually a congenital saccular protrusion on the wall of a vessel. The wall of such a protrusion is thinner than the wall of the vessel itself, and a slight increase in blood pressure in stressful situations or during physical exertion is often enough to rupture it.
A rupture of a vessel on the surface of the brain allows blood to enter the space surrounding the brain (subarachnoid space). This type of stroke is called subarachnoid hemorrhage. The most common cause is a ruptured aneurysm.
The brain catastrophe itself occurs quite quickly: from several minutes to several hours (less often than several days). The time after a stroke is conventionally divided into acute (up to 3 weeks), recovery (up to 1 year) and residual (over a year) periods. During the acute period, both pathological processes occur (for example, an increase in cerebral edema) and processes that promote recovery (improved blood supply to the areas surrounding the lesion, a decrease in the size of the hemorrhage, a decrease in the compression of the surrounding brain matter by the hematoma).
Very rarely, a stroke is asymptomatic. When the first symptoms of a stroke appear, you should immediately consult a doctor. After all, a stroke is brain damage!
Risk factors for stroke
Risk factors for stroke can be divided into controllable (those that can be influenced by the doctor by issuing recommendations or by the patient himself by changing lifestyle) and uncontrollable (which cannot be influenced, but must be taken into account).
Controlled (adjustable) risk factors:
- high blood pressure (above 140/90 mmHg)
- smoking cigarettes
- alcohol abuse
- atrial fibrillation and other heart diseases
- lifestyle factors (excess weight, physical inactivity, poor diet and stress factors)
- increased blood cholesterol
- diabetes
- previous transient ischemic attack (TIA) and stroke
- use of oral contraceptives
Uncontrolled (unregulated) risk factors:
- age
- floor
- heredity
Stroke Prevention
1. Monitor your blood pressure. As statistics show, out of 100 patients with hypertension, only half know about their high blood pressure (although hypertension, as a rule, is visible a mile away - by the characteristic complexion, tense facial expressions, and often solid dimensions). And only 10-15 people out of 100 keep it, so to speak, in check with daily monitoring and medication. If you suffer from arterial hypertension, monitor your blood pressure regularly (twice a day!). A simple thing: you should have a blood pressure monitor at work and at home. According to the criteria of the World Health Organization, pressure above 140/90 mmHg is recognized as arterial hypertension. However, it is necessary to keep in mind that there are no hard numbers, and you cannot adhere to this guideline. If a person has had a blood pressure of 90/60 all his life (this is especially common in women), then its increase to 130/80 often results in a hypertensive crisis. On the other hand, it would be illiterate to “bring down” the pressure to 130/80 for those who have had it at 170/100 for a long time: after all, sharp fluctuations are extremely dangerous. However, in any case, the “pass” beyond 140/90 is a reason to see a doctor and take special medications.
2. Reduce the number of cigarettes you smoke per day if you smoke, and in the future completely give up this bad habit.
3. Drink alcohol in moderation (no more than 2 glasses of wine per day or 50 ml of spirits).
4. It is necessary to know about the presence or absence of any heart rhythm disturbances. To do this, it is enough to take an ECG once every six months. The main direction of preventing stroke in atrial fibrillation is to reduce the likelihood of blood clots forming in the cavities of the heart, which is achieved by taking medications.
5. Find out your blood cholesterol level. If it increases, consult a doctor. Follow all of his recommendations for controlling your cholesterol levels.
6. If you suffer from diabetes, follow your doctor's recommendations and do not let your blood sugar levels rise above normal.
7. Exercise. Lead an active lifestyle. Physical activity should be chosen according to your ability, age, health and on the advice of a specialist.
8. Eat a balanced diet, avoiding too much salty and spicy food, especially at night.
9. Maintain emotional balance, taking a position “above the fray” whenever possible. If you overreact to events, are very worried, or angry, do a very simple thing: try squeezing a tennis ball. You will not only throw out unnecessary emotions, but also... you will not be able to be angry anymore, since you have already switched psychologically.
If the first symptoms of a stroke occur, consult a doctor immediately!!!
The symptoms of the disease are quite obvious and allow even an ordinary person, not a specialist, to diagnose a stroke, in some cases even a type of stroke.
Signs and symptoms do not differ significantly by gender:
- weakness and impaired coordination of limb movements;
- short-term speech disorders, difficulties with understanding speech and speaking;
- numbness of one half of the body (face, tongue, hands, etc.);
- temporary or complete loss of vision;
- dizziness, double vision;
- walking disorders and problems;
- unsteadiness of gait
- severe headaches, nausea, vomiting, increased blood pressure, etc.;
- disturbance of consciousness.
It is extremely desirable for every person to know what the main signs of this disease are. Knowing how to recognize a stroke or symptoms of cerebrovascular disease and signs of acute cerebrovascular accidents (ACVA), you can help a sick person, and in especially serious cases, save his life.
If you suspect a stroke, ask the person to do three simple things (if possible):
- smile (a person will not be able to do this - there will be either asymmetry or a distortion of one side of the face);
- say a simple sentence (speech should be slurred and meaningless, or absent altogether);
- raise both arms (the person will be able to raise only one or will raise one arm lower than the other).
In some cases, if you ask a person to stick out their tongue, the tongue will be skewed to one side (although this does not always indicate a stroke, it may be one of the symptoms of a diagnosis of cerebrovascular disease, CVD).
A person who has had a stroke will not be able to fulfill these requests if the stage of development of the condition is deep. A severe stroke is accompanied by loss of consciousness and convulsions. The rate of stroke development is high, so it is quite easy to suspect it.
In any case, if a person feels unwell, whether or not you suspect a stroke, you need to call an ambulance.
The quality, quantity and degree of consequences and complications after a stroke depend not only on the severity of the injury, but also on the symptoms, on the interval between the incident and the diagnosis, on the time and volume of assistance provided and treatment provided, on the rehabilitation completed, its nature and intensity.
A small or quickly “caught” stroke occurs with minimal consequences, and sometimes they may even be absent, but these are extremely rare cases. Most often, violations are more serious and persistent.
The main and most significant disorders after a stroke:
decreased muscle strength on one side opposite the one where the brain is damaged (right-sided or left-sided hemiparesis after a stroke): difficulty moving (sometimes aids are needed), caring for oneself (dressing, eating, personal care, etc.) and etc.;
facial asymmetry and disorders of facial muscles;
speech impairment (can be not only a consequence, but also the first sign of a stroke): partial or complete loss of the ability and ability to speak and understand the speech of another person;
impaired coordination of movement if there has been damage to the brain stem (impairments vary in degree and may subside for some time after brain damage);
visual impairment: loss of half or a quarter of the visual image;
impairment of hearing, smell and habitual skills in normal life.
Stages of stroke (stroke and cerebral hemorrhages)
The stages of circulatory disorders depend on their type:
acute form (stroke itself), which occurs suddenly and symptoms can last up to one day;
chronic cerebrovascular accident.
Acute forms of stroke with all the characteristic signs usually develop within a few hours, but not more than one day. Acute forms are easily recognized, and the main thing here is not to miss the moment and quickly seek help from a doctor.
Stages of chronic cerebrovascular disease (cerebrovascular disease):
the first stage is similar to chronic fatigue syndrome: fatigue, insomnia, headaches and dizziness, frequent mood swings and absent-mindedness; transient numbness in the arms or legs;
the second stage is characterized by impaired movement, tinnitus, loss of concentration, decreased performance, constant dizziness and pain in the head;
The third stage is characterized by personality degradation, development of dementia, hand tremors, speech impairment, etc.
Treatment. Treatment Goals
Correction of disorders of vital functions and body systems.
Minimization of neurological defect.
Prevention and treatment of neurological and somatic complications.
Treatment goals
Normalization of respiratory function.
Normalization of blood circulation.
Regulation of homeostasis.
Reducing cerebral edema.
Symptomatic therapy.
In ischemic stroke, restoration of blood flow in areas of cerebral hypoperfusion (reperfusion).
In case of cerebral hemorrhage - reducing high blood pressure, stopping bleeding and removing the hematoma, in some cases eliminating the source of bleeding (aneurysm).
In SAH – stopping bleeding, eliminating the source of bleeding (aneurysm).
Neuroprotection and reparative therapy.
What are the features of diagnosing ischemic stroke in the territory of the right middle cerebral artery?
It is worth noting that often computed tomography does not allow identifying any ischemic changes in the brain parenchyma for a certain moment after the onset of strokes, precisely the time that is very important as the beginning of the treatment of this type of disease.
Thanks to the use of magnetic resonance imaging, it becomes possible to more accurately determine the presence and nature of any ischemic changes in the main brain during strokes. After obtaining data from magnetic resonance imaging, it becomes possible to identify early ischemic changes. Today it has become possible to combine different modes, which makes it possible to determine more severe, subacute and congenital ischemic changes in the brain parenchyma.
Main services of Dr. Zavalishin’s clinic:
- consultation with a neurosurgeon
- treatment of spinal hernia
- brain surgery
- spine surgery
What's the prognosis?
People who have had a cerebral infarction have a good chance of recovering and even making a full recovery. If the patient’s condition remains stable within 60 days after the attack, this means that he will be able to return to normal life within a year.
In order to prevent this disease from affecting you, you need to adhere to the right lifestyle , nutrition, exercise, avoid stressful situations, monitor your body weight, and give up bad habits.
| Atherothrombotic | Formation of cholesterol plaques in large and medium-sized arteries, gradually blocking blood flow |
| Cardioembolic | Embolism by a blood clot in one of the vessels of the middle artery of the brain, large areas of brain tissue are affected, the process begins abruptly |
| Lacunar | The lumen of small arteries is blocked, causing focal ischemia (the size of one lesion is no more than 1.5 cm), gradually affecting the brain stem |
| Rheological | Associated with disturbances in blood composition and hemostasis |
| Hemodynamic | Associated with fluctuations in blood pressure or changes in cardiac output |
What is the procedure for treating ischemic stroke in the territory of the right middle cerebral artery?
To begin with, it is worth noting that the healing process is quite long and requires patience on the part of patients. At the very beginning of the healing process, you should normalize your lifestyle and attend rehabilitation events. The motor rehabilitation process includes strength and dexterity in each limb, self-care skills, all of which can be fully or partially rehabilitated. The speech rehabilitation process includes every session with specialists, in particular with speech therapists and neuropsychologists, every exercise necessary to restore common reading or counting disorders. As for the psychological and social healing processes, a healthy climate should be created in families, participation in any cultural event within social circles.
Quite often, specialists in this field of activity prescribe their patients to use various types of antidepressants, which are selected individually for each patient. Great attention should be paid to this, because using your own assumptions about taking antidepressants can only lead to various complications and side effects that can provoke undesirable consequences. That is why only the attending physician can prescribe the period of taking the drugs and the immediate dosage. The use of antiaggregates can reduce the risk of stroke recurrence, and in cases of no therapy, the disease may also return.
Danger and consequences
The disease is extremely dangerous. In 40% of cases it ends in death in the first hours after the attack. However, with timely first aid, the patient is able not only to survive, but also to subsequently lead normal life activities.
The consequences of a cerebral infarction can be very different, ranging from numbness of the limbs to complete paralysis and even death.
Here we will talk about all the stages of rehabilitation of patients who have suffered a myocardial infarction.
Whether or not a disability group is given for myocardial infarction, you will find out separately.
Prevention
To prevent pathology, doctors recommend leading a healthy lifestyle and eliminating provoking factors. Risk factors include consumption of salty, fatty foods, low physical activity, excess weight, habits that are harmful to blood vessels and health in general - smoking, abuse of alcoholic beverages.
Ischemic attacks are the first signs of serious disturbances in the functioning of the blood flow system and the entire body. More than 30% of people who have suffered an attack are subsequently diagnosed with a cerebral infarction or stroke. At the initial stages of development, the pathology is treatable. Based on the diagnostic results, the doctor will determine the cause of the disorders and prescribe a course of treatment.
Short description
The middle cerebral artery (ICD-10 code - I63.0 - I63.8) is the largest branch of the internal carotid artery. It is divided into the left and right MCA and serves as the source of blood supply to the cerebrum, insula and cortex. Since the SMA is part of the circle of Willis, blood flow in the areas supplied by it does not occur through this circle, but through the cortical and meningeal branches.
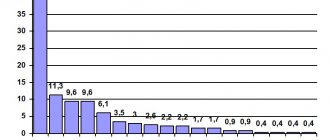
The incidence rate of this type of pathology is small. Middle cerebral artery stroke is diagnosed in 3% of all cases.
Appendix A1. Composition of the working group
| Krylov Vladimir Viktorovich | Academician of the Russian Academy of Sciences, Director of the Clinical Medical Center of the Moscow State Medical and Dental University named after. A.I. Evdokimova, head of the department of emergency neurosurgery at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky, Head of the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Dreval Oleg Nikolaevich | Doctor of Medical Sciences, Professor, Head of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Dzhindzhikhadze Revaz Semenovich | Candidate of Medical Sciences, Associate Professor of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Lazarev Valery Alexandrovich | Doctor of Medical Sciences, Professor of the Department of Neurosurgery of the Russian Academy of Postgraduate Education of the Ministry of Health of the Russian Federation |
| Dashyan Vladimir Grigorievich | Doctor of Medical Sciences, Professor of the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Nikitin Andrey Sergeevich | Candidate of Medical Sciences, assistant at the Department of Neurosurgery and Neuroresuscitation, Moscow State Medical and Dental University. A.I. Evdokimova |
| Petrikov Sergey Sergeevich | Doctor of Medical Sciences, Professor of the Russian Academy of Sciences, Deputy Director of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky, professor of the department of neurosurgery and neuroreanimation of the Moscow State Medical and Dental University named after. A.I. Evdokimova |