The term “critical ischemia” is usually used for patients whose unfavorable condition persists for 2 weeks or more. In the Fontaine-Pokrovsky classification, ischemia refers to stages 3-4 of arterial pathologies.
In the scientific literature, the course of the disease is associated with the prognosis of cancer patients.
- About 25% of patients with this diagnosis die.
- 30% lose a limb through amputation.
- 75% die from a stroke or myocardial infarction over the next few years.
- Only 55% of patients retain both limbs, subject to timely medical intervention.
As a rule, necrosis affects the lower legs, depriving the oxygen and nutrients transported by the arterial blood flow. Developing gangrene requires urgent surgical intervention, which consists of removing the affected part of the limb. Otherwise, it leads to rapid death.
Diagnosis of acute ischemia during examination by a vascular surgeon
The classic picture of acute ischemia is determined by six symptoms:
- Sudden leg pain
- Pale skin
- Absence or deficit of movement in the affected limb
- Absence of pulse in the affected limb
- Decreased skin sensitivity
- Decreased skin temperature
The pain may be constant or with passive movement of the affected limb. With an embolic blockage, the pain is usually sudden and very intense. With thrombosis, the pain intensity is much less, and sometimes there is a progressive increase in intermittent claudication.
Obliterating atherosclerosis
Obliterating atherosclerosis
| Obliterative atherosclerosis – occlusive-stenotic damage to the arteries of the lower extremities, leading to circulatory failure of varying severity. Obliterating atherosclerosis is manifested by chilliness, numbness of the feet, intermittent claudication, pain, and trophic disorders. Surgical methods include prosthetics , endarterectomy , thromboembolectomy , balloon angioplasty , and bypass surgery . |
- Obliterating atherosclerosis is a chronic disease of peripheral arteries, characterized by occlusive lesions and causing ischemia of the lower extremities. In cardiology and vascular surgery, obliterating atherosclerosis is considered as the leading clinical form of atherosclerosis (the third most common after ischemic heart disease and chronic cerebral ischemia). Obliterating atherosclerosis of the lower extremities occurs in 3-5% of cases, mainly in men over 40 years of age. Occlusive - stenotic lesions often affect large vessels ( aorta , brachiocephalic trunk , common carotid , iliac arteries ) or medium- sized arteries ( vertebral orifices , tibial , femoral ). In obliterating atherosclerosis of the arteries of the upper extremities the subclavian artery usually affected .
Stenosis of the arteries by more than 70% of the normal diameter leads to a change in the nature and speed of blood flow .
Factors predisposing to the occurrence of obliterating atherosclerosis :
- smoking,
- alcohol consumption,
- elevated blood cholesterol levels,
- hereditary predisposition,
- insufficient physical activity,
- nervous overload, menopause.
Obliterating atherosclerosis often develops against the background of existing concomitant diseases - arterial hypertension , diabetes mellitus ( diabetic macroangiopathy ), obesity , hypothyroidism , tuberculosis , rheumatism .
Local factors contributing to occlusive-stenotic damage to the arteries include previous frostbite and leg injuries. Almost all patients with obliterating atherosclerosis have atherosclerosis of the vessels of the heart and brain.
The appearance of plaques on the walls of the internal carotid arteries is fraught with dire consequences. Plaques are sites where blood clots form. This leads to complete blockage of the lumen of the arteries. A so-called ischemic stroke occurs. In addition, thromboembolism may develop. This condition occurs when a small blood clot breaks off from an atherosclerotic plaque, blocking the arteries of the brain. When blockage of small-caliber arteries occurs, a transient ischemic attack develops.
Classification of obliterating atherosclerosis
During obliterating atherosclerosis of the lower extremities, there are
4 stages:
- 1 – pain-free walking is possible over a distance of more than 1000 m. Pain occurs only during heavy physical activity.
- 2a - pain-free walking at a distance of 250-1000 m.
- 2b - pain-free walking at a distance of 50-250 m.
- 3 – stage of critical ischemia. The pain-free walking distance is less than 50 m. Pain also occurs at rest and at night.
- 4 – stage of trophic disorders. Areas of necrosis appear on the heel areas and on the toes, which can subsequently cause gangrene of the limb.
Taking into account the localization of the occlusal - stenotic process the following are distinguished :
- obliterating atherosclerosis of the aorto-iliac segment,
- femoropopliteal segment,
- popliteal tibial segment,
- multi-storey arterial damage. Based on the nature of the lesion, stenosis and occlusion are distinguished.
According to the prevalence of obliterating atherosclerosis of the femoral and popliteal arteries V types of occlusive - stenotic lesions are distinguished :
- I – limited (segmental) occlusion;
- II – widespread lesion of the superficial femoral artery;
- III – widespread occlusion of the superficial femoral and popliteal arteries; the area of trifurcation of the popliteal artery is passable;
- IV – complete obliteration of the superficial femoral and popliteal artery, obliteration of the fork of the popliteal artery; the patency of the deep femoral artery is not impaired;
- V - occlusive-stenotic lesion of the femoral-popliteal segment and deep femoral artery.
Variants of occlusive - stenotic lesions of the popliteal - tibial segment with obliterating atherosclerosis are represented by type III :
- I — obliteration of the popliteal artery in the distal part and the tibial arteries in the initial parts; patency of 1, 2 or 3 arteries of the leg is intact;
- II - obliteration of the arteries of the leg; the distal part of the popliteal and tibial arteries are patent;
- III - obliteration of the popliteal and tibial arteries; individual segments of the arteries of the leg and foot are patent.
Symptoms of obliterating atherosclerosis
The initial manifestations of obliterating atherosclerosis include chilliness and numbness in the feet, increased sensitivity of the legs to cold, “crawling goosebumps”, burning of the skin. Pain soon appears in the calf muscles when walking long distances, which indicates vasoconstriction and a decrease in blood supply to the tissues. After a short stop or rest, the pain subsides, allowing the patient to resume movement. Intermittent claudication or peripheral ischemia syndrome is the most constant and early sign of obliterating atherosclerosis.
With Leriche syndrome - atherosclerotic changes in the aorto-iliac segment, pain is localized in the muscles of the buttocks, thighs, and lumbar region. In 50% of patients, occlusion of the aortoiliac segment is manifested by impotence .
Tissue ischemia in obliterating atherosclerosis is accompanied by a change in the color of the skin of the lower extremities: at the beginning of the disease, the skin becomes pale or ivory; in the late stages of obliterating atherosclerosis, the feet and fingers acquire a purple-bluish color. There is atrophy of the subcutaneous tissue, hair loss on the legs and thighs, hyperkeratosis, hypertrophy and layering of the nail plates. Signs of impending gangrene are the appearance of non-healing trophic ulcers in the lower third of the leg or foot . The slightest damage ( bruises , scratches , abrasions , calluses ) of an ischemic limb can lead to the development of skin necrosis and gangrene .
In acute form of obliterating atherosclerosis (14%), obstruction of the artery site rapidly increases, trophic disorders develop rapidly and rapidly, up to gangrene. Patients require urgent hospitalization and limb amputation . _
In approximately 44% of patients, the clinical picture of obliterating atherosclerosis develops subacutely and occurs with recurrent seasonal exacerbations. In this case, a course of inpatient and outpatient treatment is carried out, which allows to slow down the progression of obliterating atherosclerosis.
The chronic form of obliterating atherosclerosis proceeds relatively favorably : due to the well-preserved patency of the great vessels and the developed collateral network, there are no trophic disorders for a long time. With this clinical variant, outpatient treatment provides a good therapeutic effect.
Diagnosis of obliterating atherosclerosis
The algorithm for diagnostic examination of a patient with suspected obliterating atherosclerosis includes:
- consultation vascular surgeon ,
- determination of pulsation of the arteries of the extremities , measurement of blood pressure with calculation of the ankle - brachial index ,
- Doppler ultrasound ( duplex scanning ) of peripheral arteries ,
- peripheral aorto-arteriography ,
- MSCT - angiography and MR - angiography
Treatment of obliterating atherosclerosis
- medicinal
- physiotherapeutic
- sanatorium
- angiosurgical treatment
To slow down the progression of atherosclerotic changes in the arteries , it is necessary to eliminate risk factors - correction of arterial hypertension , disorders of carbohydrate and lipid metabolism , quitting smoking , preventing foot injuries , hygienic and preventive foot care , wearing comfortable shoes .
Drug treatment of obliterating atherosclerosis is carried out with drugs that reduce erythrocyte aggregation (infusions of rheopolyglucin, rheomacrodex, pentoxifylline), antithrombotic drugs (aspirin), antispasmodics (papaverine, xanthinol nicotinate, no-spa), and vitamins. To relieve pain, analgesics, paranephric and paravertebral blockades are used.
In case of acute occlusion (thrombosis or embolism), the administration of anticoagulants (subcutaneous and intravenous heparin) and thrombolytics (intravenous streptokinase, urokinase) is indicated.
Physiotherapeutic treatment:
- hyperbaric oxygenation,
- physiotherapeutic (electrophoresis, UHF, magnetic therapy, interference therapy)
- balneological procedures (hydrogen sulfide, pine, radon, pearl baths; mud applications),
- ozone therapy,
- ILBI.
When trophic ulcers form , dressings are performed with topical preparations .
Surgical treatment of stage 2-3 obliterating atherosclerosis can be carried out through endovascular or open interventions .
Methods of revascularization the lower extremities include
- dilatation / stenting of affected arteries ,
- endarterectomy,
- thromboembolectomy,
- bypass operations ( aorto - femoral , aorto - iliac - femoral , ilio - femoral , femoral - femoral , axillary - femoral , subclavian - femoral , femoral - tibial , femoral - popliteal , popliteal - foot bypass ),
- prosthetics ( replacement ) of the affected vessel with a synthetic prosthesis or autovenous
Palliative interventions for obliterating atherosclerosis are carried out when radical surgical treatment is impossible and are aimed at strengthening collateral circulation in the affected limb. These include lumbar sympathectomy, revascularizing osteotrepanation, periarterial sympathectomy, etc.
At stage 4 of obliterating atherosclerosis, amputation of a limb to an optimal level that takes into account the boundaries of ischemic disorders most often indicated .
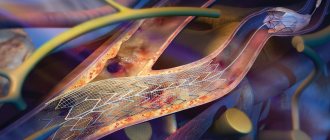
The least invasive method of surgical treatment peripheral artery disease is the technique of angioplasty and stenting . It is used if large arteries have been damaged. Angioplasty involves inserting a flexible catheter into the arterial lumen through the femoral vein. After this, a conductor is inserted, delivering a special balloon to the place where the vessel is narrowed. By inflating the balloon, the normal lumen of the vessel is restored.
In more serious cases, arterial bypass surgery . For this purpose, an additional vessel is created. Blood flow passes through it, bypassing the affected area of the artery. Both artificial prostheses and the patient’s veins are used for the shunt.
The endarterectomy method involves surgical removal of the atherosclerotic plaque. To do this, you need to open the artery. However, it is important to consider that such a procedure may disrupt the overall blood flow through the artery. Consequently, the advisability of using endarterectomy is determined taking into account the location of the lesion and the degree of disruption of blood flow in a particular artery.
The absolute indications for surgical treatment are :
1. Chronic critical limb ischemia with patent arteries of the leg .
2. Aneurysm with threat of rupture .
3. Hemodynamically significant (> 60%) stenosis of the internal carotid artery or ulcerated plaque in the presence of symptoms of cerebral ischemia .
4. Embolism , thrombosis or vascular injury with decompensation of blood circulation in the limb .
Other indications for surgery , such as intermittent claudication corresponding to stage II b , sharply reducing the quality of life and not correctable by other treatment methods , asymptomatic stenosis the carotid arteries more than 60%, small abdominal aortic aneurysms , etc. , are considered relative and determined the general condition patient and the capabilities of the medical institution .
Contraindications to surgical treatment :
- wet gangrene with septic condition ,
- the presence of severe dysfunction of vital organs that makes surgical intervention impossible ( myocardial infarction , cerebrovascular accident , heart failure , low coronary circulatory reserve , respiratory , renal , liver failure )
Endarterectomy , as a rule, is performed on patients with segmental arterial occlusions not exceeding 7–9 cm in length. Open endarterectomy is performed within the arteriotomy wound and involves removing the altered intima along with plaques and mural thrombi.
Endarterectomy can be performed in a semi-closed manner: the obliterating masses are peeled off and removed using long vascular rings or other devices. With a significant spread of the occlusive process and severe calcification, endarterectomy is ineffective. In these cases, shunting of the affected segment , the purpose of which is to restore blood flow bypassing the affected area. Prosthetics are performed in patients who require resection of the altered vascular wall.
For occlusive lesions the branches of the aortic arch open endarterectomy most often performed from the common and internal carotid arteries or from the mouth of the vertebral artery .
Carotid endarterectomy , the operation of choice for atherosclerotic lesions of the carotid arteries, has become the standard of preventive surgery.
The surgical operation consists of removing the atherosclerotic plaque. The operation is performed under anesthesia. Its essence is to dissect the tissue above the carotid artery, isolate the vessel, dissect the wall of the carotid artery, and remove the plaque. After this, the vessel is sutured.
This operation is more traumatic, usually takes longer, is performed under anesthesia and carries more complications. The sutures are removed on the 7th day, patients are discharged with a normal course of the postoperative period on the 9-10th day. According to modern international requirements, the level of complications in a clinic where such operations on the carotid arteries are performed should be no higher than 5%. This means that 5 out of 100 patients experience various complications. The operation is contraindicated in the presence of serious somatic diseases (diabetes mellitus with high sugar levels, arterial hypertension, etc.)
Possible postoperative complications of carotid endarterectomy
As with any other surgical operation, complications are possible after carotid endarterectomy. the most serious of these is stroke. The risk of its development is 1–3%. In addition to stroke, there is a complication such as repeated blockage of the carotid artery, called restenosis . It most often occurs in those patients who have not given up smoking. The risk of developing restenosis is 2-3%. Another complication is nerve damage, which leads to voice disturbance (hoarseness), difficulty swallowing, and numbness in the face or tongue. Usually these complications do not require special treatment and resolve on their own within a month.
In case of occlusion of the subclavian artery, leading to the development of subclavian steal syndrome, the operation of choice is carotid - subclavian bypass or resection of the subclavian artery with implantation into the common carotid .
In case of widespread damage to the main arteries of the aortic arch (brachiocephalic trunk, common carotid), their resection with prosthetics or bypass surgery .
open endarterectomy is also most often performed ; in case of widespread damage bypass surgery ( prosthetics is performed .
In the treatment of occlusive lesions of the abdominal aorta and arteries of the lower extremities, the most popular operations are aorto - femoral ( iliac - femoral ) bypass and femoral - popliteal ( femoral - tibial ) bypass . In the aortofemoral position, the most widely used are synthetic prostheses made of fluorlon-lavsan, dacron and polytetrafluoroethylene (PTFE), the five-year patency of which is 85–90%.
| Endoprosthetics at aneurysm peripheral arteries – a method of minimally invasive X-ray surgical treatment of local asymmetric bulging of the arterial wall by installing an intravascular endoprosthesis. Aneurysms of peripheral arteries are a consequence of inflammatory, atherosclerotic, traumatic changes in the walls of the arteries. The endoprosthesis is installed into the lumen of the peripheral artery using the X-ray endovascular method using a special delivery catheter. After implantation of the endoprosthesis, the aneurysmally altered wall is isolated from the blood flow and is not subject to pressure, which eliminates the rupture of the aneurysm. |
Nowadays, reconstructive surgery of the abdominal aorta, carotid arteries, arteries of the lower extremities with atherosclerosis is considered one of the most developed sections of angiosurgery. Despite this, the results of the operations are still far from perfect. The frequency of early postoperative thrombosis of grafts or reconstructed arteries can be 4–13 % , late reocclusions – 8.5–30 % for the aorto - iliac and 22–60 % for the femoral - popliteal segments . In 10% of patients, attempts at reconstructive surgery end in amputation of limbs in the early postoperative period .
Throughout the world, the last decade has been a time of rapid development of X-ray endovascular surgery - one of the highest priority areas. The endovascular technique has emerged as a beneficial alternative to open surgery.
Intravascular ( endovascular ) stents are intraluminal retention devices that look like a thin mesh of metal threads that are strong enough to withstand the resistance of the arterial wall and maintain good patency of the recanalized area .
Preoperative preparation and postoperative management of patients usually carried out according to the following scheme .
The day before stenting, ticlid is prescribed at a dose of 500 mg/day. During the intervention, rheolytics and anticoagulants are administered, symptomatic therapy is carried out (antispasmodics, atropine); After the intervention, patients receive low molecular weight heparin (fraxiparin 0.3–0.6 2 times a day for 3 days), symptomatic therapy continues for 3–5 days. Patients are discharged 3–7 days after surgery. Patients take antiplatelet agents (ticlid or plavix, and in some patients aspirin) for at least 1 month. after the intervention.
According to indications ( if thrombosis or restenosis is suspected in stenting area or if lesions of previously unoperated arteries are detected ) , CTA and / or control angiography is performed .
If these changes are detected , multiple repeated endovascular interventions can be successfully used , thereby significantly delaying the time when a patient with progressive occlusive lesions will require traditional surgical intervention , or avoiding it altogether .
The range of diseases that are subject to minimally invasive treatment in the first place :
l Lesions of an isolated nature ( segmental stenoses , short occlusions ;
l Lesions that are difficult to access for open surgical interventions ( renal arteries , branches the aortic arch , visceral arteries );
l Restenosis after traditional operations , stenosis of vascular anastomoses ;
l Severe concomitant diseases that increase the risk of traditional operations .
Complicated ( embolic-dangerous ) atherosclerotic plaques , as well as a combination of stenotic lesions of the carotid arteries with kinks , tortuosity and looping , accompanied by significant lengthening of the artery and requiring traditional reconstructive surgery are considered a contraindication to stenting .
Stenting of the vertebrobasilar arteries has proven itself in surgical practice and is already the method of choice . Balloon angioplasty and stenting are indicated for stenosis and occlusion of the proximal part of the subclavian artery, accompanied by significant compromise of the vertebrobasilar blood flow, up to the development of steal syndrome, and damage to the brachiocephalic trunk.
Stenting of the arteries of the lower extremities is indicated in patients starting from stage II of ischemia according to the Fontaine-Pokrovsky classification. The ideal type of lesion for stenting is a short concentric stenosis or an isolated occlusion of less than 5 cm in length for the iliac artery and less than 10 cm in length for the superficial femoral artery. The most commonly performed stenting is the iliac, superficial femoral, and popliteal arteries.
In the late postoperative period, due to the progression of atherosclerotic changes in the proximal or distal vascular bed, repeated stenting is possible. Stenting can be used for anastomotic stenoses after previously performed bypass operations. Renal artery stenting is the most advantageous location
Preparation for carotid artery stenting surgery
Typically, preparation for carotid stenting involves taking aspirin a week before surgery. This is necessary to reduce blood clotting.
Are you a candidate for carotid stenting ?
Currently, carotid stenting surgery is indicated for patients at high risk of complications from endarterectomy. Indications for carotid stenting include significant narrowing (60%) of the lumen of the carotid arteries, symptoms of microstroke and stroke. If you do not have any symptoms, the indications for stenting are significant narrowing (80%) of the lumen of the carotid arteries and a high risk of complications from endarterectomy. In addition, carotid stenting is indicated for patients who have previously undergone endarterectomy in cases of recurrent narrowing of the arterial lumen.
Carotid stenting is not recommended for :
- Presence of abnormal heart rhythm
- Allergy to drugs used during the procedure
- Brain hemorrhages within the previous 2 months
- Complete blockage of the carotid artery
Risk factors for complications of carotid stenting
- High blood pressure
- Allergy to
Ultrasound duplex scanning
Ultrasound duplex scanning allows you to determine the patency of the arteries, localize the site of blockage of the vessel and the state of blood flow below the site of occlusion. Often, in acute ischemia, this diagnosis is enough to determine treatment tactics and send the patient to the operating table. With an embolism or rupture, the arteries below the blockage are usually empty or thrombosed, and blood flow in them is not detectable. Blood flow in the veins is sharply slowed down. With thrombosis, blood flow can be detected below the site of blockage, but its speed is sharply reduced; most often, blood flow through the main vessels cannot be detected, but blood flow can be seen through collaterals. As a rule, this is due to
Angiography
To resolve the issue, surgical tactics require information about the patency of the arteries of the affected limb. The choice of technique for restoring blood circulation depends on the condition of the inflow pathways to the affected limb and the vascular bed below the site of blockage. In addition, angiography can distinguish embolism from thrombosis against the background of atherosclerotic narrowing. During an angiographic examination, endovascular treatment can be undertaken in the form of thrombectomy and angioplasty of the affected segments or local thrombolytic therapy can be performed.
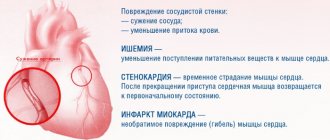
Arterial embolism is an acute blockage of a vessel by a thrombus or other object brought from other parts of the vascular bed. Most often, vascular surgeons deal with thromboembolism from the heart cavity during a heart attack or atrial fibrillation, from the cavity of the aneurysm of the vessel overlying the blocked artery.
Consequences of acute cessation of blood flow
The sudden cessation of blood flow leads to the phenomenon of acute ischemia. The organs and tissues that are supplied by this artery lack nutrition and oxygen, so they begin to slowly die. The most specialized tissues are affected first—nervous, muscle, and finally skin. The body tries to restore blood circulation by opening additional bypass pathways for blood flow, so sometimes tissue death is stopped. But the likelihood of such an outcome is low. In any case, acute ischemia leads either to gangrene or to the development of chronic circulatory deficiency - critical ischemia.
Improving collateral blood flow
- Prostaglandins
Discovering all possible bypass routes to the blood supply. For this purpose, prostaglandin preparations (alprostan, vazaprostan) have proven themselves best. They are used in the form of long-term 3-5 hour intravenous infusions. The use of prostaglandins can sometimes reduce critical ischemia and save the limb. Physiotherapy (magnetic field, laser) serves the same purposes. These patients can be treated with conservative therapy for no longer than two weeks. If there is no effect, then resolve the issue with revascularization.
- Improving blood flow
It is necessary to examine the coagulation and anticoagulation system, blood viscosity, cholesterol, fat and protein content, and other indicators. It is necessary to eliminate the identified violations as much as possible. For this purpose, intravenous infusions of various drugs rheopolyglucin, dextrans, and trental are used. Increasing the oxygen content in the blood Hyperbaric oxygenation (a chamber with increased oxygen pressure) is used. The principle is simple - as pressure increases, the solubility of oxygen in the blood increases; more oxygen in the blood means more is released into the tissue. Infusions of perftoran, artificial blood that stimulates the release of oxygen into tissues, can be used.
- Stimulation of new vessel growth – Neovasculgen
To date, genetic drugs aimed at stimulating vascular growth have proven ineffective. Neovasculgen, the most advertised and expensive drug, was tested in our clinic, but we did not observe any effect in patients with critical ischemia. The basis of the treatment of chronic ischemia is to improve blood circulation in the lower leg and foot. The hope for drug treatment, including the use of prostaglandins (vasaprostan, ilomedil, alprostan), did not materialize, since the drugs do not reach the tissues due to serious damage to small vessels. Another therapeutic method that was of interest to surgeons and their patients was the Neovasculgen gene therapy complex. The drug is a virus-like particle that carries a gene that enhances the growth of small blood vessels. We used this drug in our clinic in patients with complex vascular pathology, but did not notice a noticeable effect. These patients required vascular surgery, and some even required amputation.
Stages of acute ischemia
1. Sudden pain in the leg, coldness, reduction in walking distance. If the collateral vessels are good, ischemia may stop at this stage with the development of intermittent claudication or critical ischemia. Most often, this stage is observed with thrombosis of altered arteries, if their lumen was previously narrowed and collateral circulation developed. At this stage, the operation is carried out after the necessary additional examination and preparation. The color of the leg may be pale or take on a bluish tint (cyanosis). The result of surgical treatment is excellent. Recovery of leg function is most often complete.
2. The symptoms described above are accompanied by weakness in the leg, which gradually worsens to the point of paralysis. However, passive movements in the fingers and other joints are possible. Such phenomena are associated with the death of nerve endings and blockade of nerve impulse transmission along the nerves. This stage of ischemia is an absolute indication for emergency surgery, since independent restoration of blood flow is impossible, and delay in intervention will lead to gangrene. Timely surgery restores blood flow with minimal loss of limb function. Numbness of the foot and fingers remains, and swelling of the leg persists for a long time.
3. Muscle death begins, first there are foci of muscle necrosis, muscle pain, and dense swelling of the lower leg. Then comes numbness of the fingers, ankle joint, and knee joint (muscle contracture). The muscles die completely. If the muscles are partially lost after restoration of blood flow and a long postoperative period, the leg may be preserved, but walking will be difficult. In the case of muscle contracture, amputation is necessary, since restoration of blood flow leads to the death of a person from poisoning with decay products.
4.Treatment
In the first stages of ischemia of the lower extremities, an attempt is made to control the process using conservative methods. Antiplatelet agents, thrombolytics and antispasmodics, hemodynamic stimulants, lipid metabolism correctors, antioxidants, and physiotherapy are widely used (according to indications). If all used and available means are ineffective, as well as in rapidly progressing and/or life-threatening cases, the only option is surgical intervention, and the most advanced and complicated situations can result in death even after amputation of the limbs.
To avoid this, certain methods of angioplasty, bypass surgery, and angioprosthetics are used in order to restore the patency of the main blood supplying arteries of the lower extremities. If amputation is inevitable, the time factor plays a critical role, and any subjective delays are unacceptable here. Self-medication is also too risky: its effectiveness in any case tends to zero, moreover: the use of some “proven folk remedies” can radically aggravate the situation.
It should also be especially noted that treatment of ischemia of the lower extremities, both conservative and surgical, makes no sense even to begin if the patient is not ready to unconditionally, once and for all, eliminate smoking. It will also require serious normalization of lifestyle (in some cases, in particular, the question of changing professions is raised), a certain diet, constant monitoring of blood pressure, and special home procedures to maintain the feet in optimal and safe condition.
Diagnosis of thrombosis or embolism
In addition to the clinical picture, it is necessary to use special research methods for diagnosis.
Ultrasound diagnostics makes it possible to clarify the nature of occlusion and identify atherosclerotic plaques during thrombosis. Thrombosis differs from embolism in the initial damage to the arteries; in embolism, the arteries are most often not affected.
Angiography is performed on the operating table to clarify the receiving vascular bed and allows you to determine the nature of the surgical intervention
Multislice computed tomography is performed when there is time for a detailed diagnosis and allows you to very accurately identify the nature of the lesions and determine treatment tactics.
Causes and risk factors
The main causes of critical ischemia of the lower extremities are:
- Obliterating atherosclerosis - vascular lumens are blocked by cholesterol (atherosclerotic) plaques;
- Thrombosis - an artery is blocked by a blood clot (thrombus) at the site of its initial formation or subsequent movement (embolism);
- Endarteritis – the inflammatory process persists, provoking vasospasm;
- Thrombangiitis, or Buerger's disease - inflammation occurs that affects arteries and veins of small and large caliber;
- Diabetic angiopathy (vascular damage caused by decompensated diabetes mellitus);
- Mechanical injuries of large arteries.