Our clinic is unique for Russia, as we use revolutionary methods of restoring blood flow, including microsurgical, endovascular and plastic surgeries. We manage to save more than 95% of limbs in patients with critical ischemia.
Critical leg ischemia is an emergency condition that requires immediate measures to improve blood supply. If the blood supply is not improved, then amputation of the limb is the only method that can save the patient from suffering and death. The danger of critical ischemia is that blood, through clogged vessels, very poorly fills the lower parts of the legs and causes their gradual death. Insufficient blood circulation does not allow the necessary medications to be delivered to the tissues of the foot and toes, which reduces the possibilities of therapy.
Anesthesia
An exhausted person needs a break from suffering. Without such rest it is impossible to continue treatment. The body simply cannot withstand any active methods. Long-term epidural anesthesia relieves pain best. A thin catheter is installed in the back, into which a painkiller is injected as needed. Anesthesia allows you to lay the patient horizontally and somewhat eliminate the swelling of the limb, and conduct the necessary studies.
Narcotic analgesics (tramadol, promedol, morphine) do not have a sufficient analgesic effect, but they allow you to dull the sensations and fall asleep. The downside is the development of tolerance and drug dependence. In some surgical departments, the use of drugs and their subsequent withdrawal can persuade the patient to amputate. Non-narcotic analgesics and sleeping pills have a very weak effect on pain, do not counteract the development of depression, and contribute to the development of acute psychosis after restoration of blood flow.
Neurostimulation is an effect on the sensitive bundles of the spinal cord using a special electrical device. Good and long-term pain relief without the administration of drugs. Allows pain relief for patients who refuse surgery. The downside is that gangrene continues, and the price for the device is about $30,000.
Classification
The classification of ischemic lesions of the lower extremities with the formation of a sudden decrease in the vascular lumen (occlusion) provides for the level of blockage.
- Abdominoaortic obstruction:
- high (above the arteries of the kidneys).
- average;
- low (behind the mesenteric artery, which arises from the aorta).
- Blockage of arterial vessels of the lower extremities:
- high;
- low.
Taking into account the intensity of clogging manifestations, the following forms are provided:
- acute;
- chronic;
- critical.
Of great importance is the division of the pathological process according to the degree of hypoxia - I-IV degrees.
Improving collateral blood flow
- Prostaglandins
Discovering all possible bypass routes to the blood supply. For this purpose, prostaglandin preparations (alprostan, vazaprostan) have proven themselves best. They are used in the form of long-term 3-5 hour intravenous infusions. The use of prostaglandins can sometimes reduce critical ischemia and save the limb. Physiotherapy (magnetic field, laser) serves the same purposes. These patients can be treated with conservative therapy for no longer than two weeks. If there is no effect, then resolve the issue with revascularization.
- Improving blood flow
It is necessary to examine the coagulation and anticoagulation system, blood viscosity, cholesterol, fat and protein content, and other indicators. It is necessary to eliminate the identified violations as much as possible. For this purpose, intravenous infusions of various drugs rheopolyglucin, dextrans, and trental are used. Increasing the oxygen content in the blood Hyperbaric oxygenation (a chamber with increased oxygen pressure) is used. The principle is simple - as pressure increases, the solubility of oxygen in the blood increases; more oxygen in the blood means more is released into the tissue. Infusions of perftoran, artificial blood that stimulates the release of oxygen into tissues, can be used.
- Stimulation of new vessel growth – Neovasculgen
To date, genetic drugs aimed at stimulating vascular growth have proven ineffective. Neovasculgen, the most advertised and expensive drug, was tested in our clinic, but we did not observe any effect in patients with critical ischemia. The basis of the treatment of chronic ischemia is to improve blood circulation in the lower leg and foot. The hope for drug treatment, including the use of prostaglandins (vasaprostan, ilomedil, alprostan), did not materialize, since the drugs do not reach the tissues due to serious damage to small vessels. Another therapeutic method that was of interest to surgeons and their patients was the Neovasculgen gene therapy complex. The drug is a virus-like particle that carries a gene that enhances the growth of small blood vessels. We used this drug in our clinic in patients with complex vascular pathology, but did not notice a noticeable effect. These patients required vascular surgery, and some even required amputation.
Stages of development and clinical picture
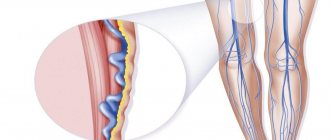
- Against the background of inflammatory and diabetic lesions of blood vessels, a gradual narrowing of their lumens occurs and subsequent blockage by blood clots or atherosclerotic plaques. In this regard, the nutrition of the lower extremities is significantly impaired.
- First, the body tries to compensate for the deficiency of nutrients and oxygen by activating the work of smaller bypass vessels. It is this process that entails the development of the first alarming symptoms - acute pain in the legs and intermittent claudication when covering a distance of no more than 30-35 m.
- Next, stagnant edematous phenomena occur, which further disrupt blood and lymph flow, squeezing the arteries. The nerve endings become inflamed, aggravating the already severe pain syndrome. Now it is characteristic of the patient and in a state of complete rest, even sleep.
- With the inevitable failure of compensation, the peak of critical ischemia occurs. If emergency medical intervention does not occur at this moment, tissue necrosis (death) begins. A gangrenous limb should be amputated, otherwise death is inevitable.
Symptoms of ischemia of the lower extremities are quite specific:
· Acute pain in the muscle tissue of the leg at rest;
· Intermittent claudication (forced stoppage of movement due to severe pain in the calf muscles);
· Deficiency of blood supply to the legs, accompanied by numbness, cooling and tingling;
· Formation of trophic ulcers, mainly in the area of the feet and toes;
· Presence of necrotic (dead) tissues;
· Blackening or bluish discoloration of the skin at the affected sites;
· Signs of decomposition of the tissues of the fingers or feet;
· Gangrene.
The pain syndrome is so intense that it cannot be relieved with conventional painkillers. During the active progression of the pathology, patients manage to relieve pain by changing body position and lowering their legs. Some patients sleep with their limbs down from the bed. In this case, the outflow of venous blood is disrupted, it accumulates in the tissues and puts more pressure on the vessels, which provokes the accelerated appearance of ulcers and necrosis.
Intermittent claudication is another obvious clinical manifestation of this pathology. It is characterized by acute pain in the calf muscles when walking short distances. An acute attack forces the patient to stop for a break, after which the pain gradually recedes. A similar sign can be noted after traveling a kilometer distance, and this is already a good reason to contact a specialist, since “painless” distances are quickly reduced due to the progression of the disease.
Considering the extremely dangerous consequences of critical ischemia of the lower extremities, if any symptom appears, you should urgently contact an angiologist or phlebologist.
Etiological factors and pathogenetic mechanism
The main reasons are all pathological conditions and processes that lead to impaired vascular patency:
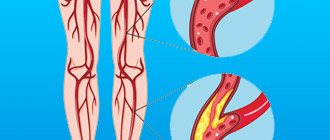
- atherosclerotic disease;
- diabetes;
- prolonged smoking;
- inflammatory process in the wall of the vessel;
- congenital vascular anomalies;
- thrombosis and thromboembolism of arterial vessels of the legs.
HAN can provoke four groups of pathologies:
- pathological processes manifested in metabolic disorders (atherosclerotic lesions, diabetes mellitus);
- prolonged inflammation in the arteries with the presence of an autoimmune component (nonspecific aortoarteritis, thromboangitis obliterans, vasculitis);
- pathologies with a disorder of the innervation of arterial vessels (Raynaud's disease and syndrome);
- exocompression of arterial vessels.
Arterial insufficiency of the legs is mostly caused by damage to the abdominal segment of the aorta or great vessels as a result of atherosclerosis (80%). Nonspecific aortoarteritis is recorded in about 10% of patients, mainly young women.
Diabetes mellitus provokes microangiopathies in 5% of patients. Thromboangiitis obliterans accounts for less than 2%, mainly affects males 20-40 years old, and is characterized by an undulating course with exacerbations and remissions.
The main risk factors for CA are: smoking, dyslipid metabolism, high blood pressure, diabetes mellitus, excess body weight, physical inactivity, alcohol abuse, psycho-emotional factors, genetic predisposition, infections, etc.
Causes of ischemia of the lower extremities
The cause of ischemia of the lower extremities may be one of the following diseases:
- atherosclerosis of the lower extremities. In this case, the lumen of the arteries is blocked by atherosclerotic deposits on the walls of the vessels;
- endarteritis (thromboangiitis) – inflammation of the artery walls, causing vessel spasm;
- thrombosis – blockage of an artery by a blood clot at the site of its formation (thrombus); or embolism - blockage (occlusion) of an artery displaced by such a clot;
- diabetic vascular damage.
Forecasts
In the absence of timely adequate treatment, critical ischemia will lead to the need for limb amputation.
Without timely surgery, a year after the first signs of critical ischemia appear, most patients undergo limb amputation due to the onset of gangrene. When performing endovascular treatment using angioplasty, in most patients the effect lasts for 6-24 months, and after that the patient has to undergo repeated intervention. Surgical treatment of critical ischemia using arterial bypass is more long-term and effective, despite the high risk of postoperative complications and the technical complexity of the operation. As a rule, the patency of the artery after such an intervention is maintained for 3-5 years, and the risk of recurrence of critical leg ischemia is very low.
Diagnosis
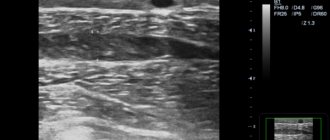
- Special examination techniques are non-invasive and invasive. The most common non-invasive method is segmental manometry with assessment of the ankle-brachial index. It allows you to measure blood pressure in different parts of the legs in comparison with that in the arms. The normal index is 1.2-1.3, in case of pathology it is less than 1.0.
- Ultrasound. Including duplex scanning. Helps in assessing arterial lumen, speed and direction of blood flow.
- Aortoarteriography is the main method of diagnosing and determining treatment tactics.
- X-ray CT with contrast, MRI or electron emission angiography.
Staged course
- The initial stage is characterized by a minimum of symptoms: the unreasonable occurrence of fatigue in the legs with little physical activity (walking up to 1 km), the appearance of stabbing sensations and chilliness in the feet, the skin is cold and pale to the touch.
- At subsequent stages, more intense manifestations occur:
- pain in the legs with the inability to move at the usual speed (“intermittent claudication”), which occurs after covering a distance of 200 m;
- pallor of the skin of the legs, hair loss, decreased elasticity of the skin, and trophic lesions appear.
Chronic ischemia with severe vascular occlusion leads to:
- pain at rest or with minimal physical activity (inability to overcome 25 m);
- muscle transformations (atrophic phenomena and weakness);
- the appearance of cracks due to minor injuries, ulcers, in the nail plates of the toes - inflammatory processes (felons).
When the lumen is blocked in the upper parts of the abdominal aorta, there are necessarily signs of ischemia of the pelvic organs (disorder of stool, urination, dysfunction of the genital organs).