Deep vein thrombosis, along with thrombophlebitis of the saphenous veins and thromboembolism of the pulmonary arteries, are combined into a single concept - venous thromboembolic complications (VTEC).
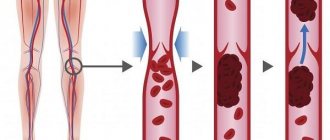
Venous thrombosis is an acute disease characterized by the formation of a blood clot in the lumen of a vein with a more or less pronounced inflammatory process and disruption of blood flow. The presence of an inflammatory component in the area of thrombosis determines another name for this disease - thrombophlebitis.
Most phlebologists, understanding the conventions of such a division of venous thrombosis, use the term “thrombophlebitis” to denote damage to the saphenous veins (in which symptoms of inflammation are pronounced), and the terms “thrombosis”, “deep vein thrombosis”, “phlebothrombosis” to denote damage to the deep veins .
Deep vein thrombosis (DVT) is a disease that negatively affects not only the venous and lymphatic return system, but also worsens the function of the cardiovascular system as a whole.
If you do not take active steps to eliminate this pathology, the further course of the pathological process becomes persistent, prone to self-development and irreversible.
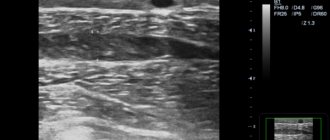
The disease does not have strictly characteristic symptoms and has many risk factors and triggering factors, which requires the additional use of additional high-precision modern instrumental diagnostic tools to clarify its presence and type of course, the main of which in modern clinical conditions is the method of ultrasound angioscanning with color mapping.
- According to the International Consensus Statement, the incidence of deep vein thrombosis in the general population is approximately 160 cases per 100,000 population, with the incidence of fatal pulmonary embolism being 60 per 100,000 population.
- In Russia, venous thrombosis affects 240,000 people annually, and pulmonary embolism, including fatal ones, develops in 100,000 of them, which significantly exceeds the incidence rates of tuberculosis, viral hepatitis, and HIV infection.
- In the United States, approximately 200,000 people are hospitalized each year for deep vein thrombosis. In this case, 1/3 is accounted for by repeated thromboses. Among Italian residents of the most active working age (from 20 to 55 years), deep vein thrombosis is diagnosed within 1%.
- Venous thrombosis occurs in a wide variety of clinical situations and complicates the course of many diseases. The incidence of postoperative thrombosis, according to various authors, is 20-59%.
What is thrombophlebitis
Thrombophlebitis is an inflammation of the venous wall with the formation of a blood clot in the lumen of the vein.
Most often, thrombophlebitis occurs in the veins of the lower extremities, but in some cases it can be localized in the veins of the upper extremities, chest, and neck. Experts usually call inflammation and thrombosis of the superficial saphenous veins thrombophlebitis. In the case of deep vein thrombosis, another term is more often used - “ phlebothrombosis ”.
In the case of inflammation of the vascular wall, in the absence of a blood clot in the lumen of the vein, the term “ phlebitis ” is used.
Diagnosis of thrombosis
Primary diagnosis is based on a detailed history and anthropometry (calf or thigh circumference).
The Wells scale is used to diagnose acute thrombosis and diagnose pulmonary embolism [8,9]. Instrumental diagnostics include compression or duplex scanning of veins, Doppler ultrasound with compression of veins, impedance plethysmography, pulmonary angiography, radiocontrast or MRI venography [6,9], CT and MRI angiography [7,9].
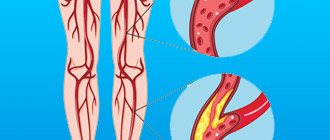
To diagnose arterial thrombosis, physical tests are used (6-minute walk test, treadmill test), determination of pulsation of superficial arteries (arteries of the dorsum of the foot), duplex scanning of the arteries of the extremities, angiography (X-ray of a vessel filled with a radiopaque substance) and measurement of transcutaneous oxygen tension [ 7].
Causes of thrombophlebitis
The main causes of venous thrombosis:
- inflammatory process (local and/or general),
- slowing down the flow of blood through the venous vessels, leading to venous stagnation (for example, due to varicose veins),
- hereditary or acquired tendency of the blood to form blood clots (coagulopathies or thrombophilic conditions),
- damage to the venous wall (sometimes even minor trauma to the vessel, for example, catheterization of a vein).
Symptoms of thrombophlebitis
- soreness,
- the appearance of local swelling of the limb,
- temperature rise,
- thickening and redness along the affected vein.
In the case of thrombophlebitis of the superficial veins, the patient may notice a gradual increase in the intensity of the changes described above over several days.
If you have these symptoms, you should definitely consult a specialist.
However, with deep vein thrombosis (phlebothrombosis), the main symptom is most often swelling of the affected limb, although it should be remembered that many patients with this form of the disease may not have any symptoms for a long time.
If swelling and pain are severe, and are also accompanied by high fever or shortness of breath with coughing attacks or chest pain, it is necessary to call an ambulance team.
These symptoms may indicate the development of deep vein thrombosis, which significantly increases the likelihood of a blood clot breaking off and migrating into the vessels of the lungs.
Thrombosis Clinic
Symptoms of thrombosis can be general, regardless of location, or specific.
Common symptoms include pain with movement and at rest, limited mobility, and decreased function of the affected organ or tissue. Symptoms of arterial obstruction (acute thrombosis, or gradual obstruction of vessel patency):
- asymmetry of blood pressure when measured on both arms [7];
- pallor of the skin, turning into cyanosis [7];
- pain at rest at night [7];
- pain when moving in the thigh, buttock, lower leg, foot, shooting or aching [7];
- sleep disorders [7];
- numbness, coldness of the limb [7];
- absence of peripheral pulsation [7];
- necrosis (necrosis) of affected tissues, trophic ulcers, gangrene [7];
- intermittent claudication [7].
Symptoms of venous thrombosis:
- pain [6];
- swelling, soft and asymmetrical [6];
- blue discoloration of the skin (skin cyanosis) [6];
- increased skin temperature of the extremities [6];
- increased sensitivity and compaction in the projection of the superficial veins [2];
- post-inflammatory hyperpigmentation [2];
- dilated saphenous veins [6];
- erythema [2].
Sometimes the only symptom of venous thrombosis is PE [6].
Risk factors for the development of thrombophlebitis
- pregnancy, childbirth, gynecological operations (including abortions).
- varicose veins;
- prolonged bed rest (for example, after surgical and orthopedic operations);
- infectious diseases;
- stroke leading to paralysis of the limbs;
- motionless body position during a long trip by car or plane;
- obesity;
- oncological diseases (including surgical treatment of malignant neoplasms, radiation therapy and chemotherapy);
- dehydration;
- the use of hormonal contraceptives and other sex hormone preparations for the purpose of replacement therapy;
- increased blood clotting (hyperhomocysteinemia, antiphospholipid syndrome, etc.);
- puncture and/or venous catheterization.
The more risk factors a patient has, the higher the risk of developing thrombophlebitis.
If you have one or more factors from the above list, consult a specialist about methods of preventing venous thrombosis.
Prevention
When the disease is diagnosed, timely treatment and prevention of disease progression are important. To do this, you need to contact a specialist in time and undergo a course of treatment.
Prevention is also:
- active lifestyle and sports;
- timely treatment of varicose veins;
- rejection of bad habits;
- balanced diet and limiting the consumption of fatty foods;
- identification and elimination of foci of infection in the body.
A favorable outcome of the disease is possible only if you consult a doctor and undergo appropriate treatment.
Confirmation of the diagnosis of thrombophlebitis
During the examination, the specialist individually selects the required minimum of research for each specific case. To confirm or exclude thrombophlebitis of the lower extremities, your doctor may choose one of the following diagnostic methods:
- Blood tests (clinical blood test, coagulogram, D-dimer);
- Venography (X-ray examination of the venous bed using the injection of a contrast agent that stains the vessels from the inside). Currently, due to the development of low-traumatic and highly informative research methods (primarily duplex angioscanning), it is used extremely rarely;
- Computed tomography and magnetic resonance imaging in vascular mode - performed in situations where ultrasound diagnostic methods are not very informative;
- Ultrasound diagnostic methods (Dopplerography and duplex angioscanning) are currently the “gold standard” for diagnosing thrombophlebitis.
After a diagnosis has been established, you may need additional diagnostics to identify the causes of thrombophlebitis, as well as control studies to clarify the nature of the dynamics of the pathological process.
Treatment methods for thrombophlebitis
Treatment of thrombophlebitis of superficial veins
In this case, the specialist may recommend treatment on an outpatient basis. The list of recommendations may include medications:
- having an anti-inflammatory effect (non-steroidal anti-inflammatory drugs, for example: Nimesil, Ibuprofen, Diclofenac, Nise, etc.);
- local remedies (compresses and ointments);
- compression methods (elastic bandages or compression hosiery, etc.);
- phlebotonic agents (Detralex, Phlebodia, Antistax, Vasoket, etc.).
With thrombophlebitis of the superficial veins, the patient rarely needs hospitalization and, with proper treatment, as well as careful adherence to medical recommendations, relief usually occurs quickly.
With the progression of superficial thrombophlebitis (growth of the thrombus border), surgical prevention of thromboembolism (separation and migration of thrombotic masses into the vessels of the lungs) and the spread of thrombosis to the deep vein system may be required. Surgical intervention in this case is performed according to urgent indications and most often consists of ligating the thrombosed superficial vein (great or small saphenous vein) at the point where it flows into the deep vein system and, if possible, removing varicose veins (thrombosed and non-thrombosed) veins.
Treatment of deep vein thrombosis
Drug therapy
Injections of blood thinning drugs - anticoagulants (heparin or its modern analogues: Clexane, Fraxiparin, Fragmin). After heparin therapy, long-term use of the tablet form of another blood thinning drug, warfarin, may be prescribed. Treatment with anticoagulants is carried out to prevent the growth of a blood clot and prevent recurrence of venous thrombosis.
If your doctor has prescribed you warfarin, strictly follow the instructions for taking the drug and monitoring your blood clotting.
Warfarin is a powerful drug that can cause a number of dangerous side effects if you do not follow your doctor's instructions.
Compression therapy
The use of elastic bandages and the selection of individual compression hosiery is one of the main tools for therapeutic effects, as well as prevention for deep vein thrombosis. Consult a specialist about possible compression therapy methods in your case.
Implantation of vena cava filter
In some cases, especially if there are contraindications to blood-thinning drugs or their ineffectiveness, a vena cava filter device can be installed in the main vein of the patient's body (inferior vena cava) to prevent the migration of detached fragments of blood clots from the veins of the lower extremities to the vessels of the lungs. The vena cava filter acts as a trap for detached blood clots. The filter can be installed for a certain period of time (3-4 weeks) or permanently. This procedure is most often performed under local anesthesia and does not require a long hospital stay.
Surgery
Thrombectomy, venous angioplasty and venous bypass.
In some cases, it may be necessary to perform a surgical intervention aimed at removing thrombotic masses of large venous trunks (thrombectomy) in the lower extremities, pelvis or abdomen. To treat long-standing blockage, bypass surgery or minimally traumatic intervention (stenting) of the affected segment of the main vein is sometimes performed.
The volume and nature of surgical intervention for deep vein thrombosis is determined individually by the vascular surgeon.
Thrombolysis
Dissolution of thrombotic masses with the help of special drugs - thrombolytics (urokinase, actilise, etc.). This procedure can only be performed in the early stages of the disease and has a number of special contraindications.
Folk remedies
Treatment of thrombophlebitis with folk remedies will help alleviate the course of the disease, reduce pain and swelling in the legs, and relieve other symptoms. These are methods that have been proven over more than one generation.
- Most urban people do not know that in the villages many diseases of the legs and arms (burns, frostbite), as well as ulcers of various origins and thrombophlebitis, were treated with goose fat. Even today it is considered one of the most effective remedies, which is used both in its pure form and in the preparation of ointments with the addition of various herbs, such as calendula or St. John's wort. Complete recovery can be achieved using a 30% ointment with the addition of comfrey roots (larkspur) crushed into a pulp. To do this, add 30 g of comfrey roots to one hundred grams of goose fat. Heat for 15 minutes, strain. The ointment is ready for use.
- Dead bee tincture. The life of bees is short. And by spring, the old individuals who worked through the summer die off. Young bees carry them to the arrival board. This is called death. They need to be collected and filled with vodka (a handful of vodka per 0.5 liters of vodka). Leave for two weeks, strain. Use as a compress, which is applied to the sore spot for 1.5-2 hours.
- A tincture on Kalanchoe leaves helps for rubbing. For this, 2 tbsp. l. spoons of finely chopped leaves are poured with 1 glass of vodka. Close the lid tightly and leave in a cool, dark place for 10 days. Rub your feet in areas where blood clots form with smooth, gentle movements.
- One of the effective remedies for this severe vein disease is homemade apple cider vinegar. It is used in the form of rubbing, after diluting it with water (a tablespoon of vinegar per glass of water).
- Nettle infusion. It not only has a beneficial effect on the circulatory system, but also heals and strengthens the entire body as a whole. It is especially useful in the spring, when there are not enough vitamins.
- Red tomato juice also promotes a speedy recovery. To do this, use a compress made from pieces or in the form of a pulp from the fruit. Apply to the affected area, securing with a bandage overnight. The bandage should not be tight.
All proposed methods of treatment with folk remedies must be agreed upon with the attending physician before use. It is better to use them in combination with drug therapy.
Diet for thrombophlebitis
A large amount of fresh vegetables, fruits, fiber, nuts, cereals, whole grain breads. Among products of plant origin, the following also have a beneficial effect on venous diseases:
- ginkgo biloba,
- ginger,
- red capsicum,
- valerian root,
- garlic,
- hawthorn berries.
Nutritional supplements and vitamins:
- vitamins C, A, E and B6,
- linseed oil,
- magnesium and calcium (in combination),
- Pycnogenol
Recommendations for changing the lifestyle of patients with thrombophlebitis
- Elevated position of the lower extremities during rest and sleep;
- Avoid prolonged static loads;
- Avoiding heavy physical activity (weight lifting);
- Avoid overheating and dehydration (long stay in the bathhouse);
- Wear compression hosiery of the required compression class (determined by a specialist);
- Limiting static loads (avoid sitting for long periods of time, standing without moving);
- Constant physical activity - walking, swimming, cycling;
- Selection of comfortable shoes and orthopedic insoles.