Causes of thrombosis
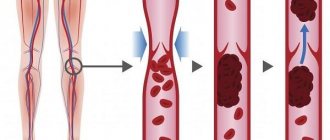
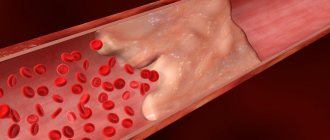
In order for a blood clot to form in a vein, a number of conditions or factors are necessary. In the classical version, there are three factors that contribute to thrombus formation (Virchow’s triad).
- hypercoagulable state (increased coagulability). There are many reasons for increased blood clotting - surgery on any part of the body, pregnancy, childbirth, diabetes, excess dietary fat, oral contraceptives, dehydration, genetic factors (rare), etc.
- injury to the inner wall of the vessel (endothelium). The vascular wall can be injured during the installation of a venous catheter, injection into a vein (due to this, thrombosis is very common in drug addicts who inject into the veins of the legs, in the groin), injuries, during radiation therapy, chemotherapy, etc.
- slowing down blood flow. It can be observed in various conditions - varicose veins, pregnancy, obesity, immobilization of a limb (for example, when wearing a cast after fractures), heart failure, forced sedentary position of the body (for example, during long air travel), compression of veins by tumors, etc.
Thrombosis can occur due to the action of one factor or a combination of them. For example, in case of a fracture of the leg bones, all three factors can be involved - increased coagulability in the case of extensive hemorrhages in the area of injury, damage to the vascular wall as a result of a mechanical shock, and a slowdown in blood flow as a result of wearing a cast.
Most often, thrombosis occurs in the veins of the lower extremities. This is due to the fact that stagnation most often occurs in these veins (obesity, varicose veins, edema, etc.).
Diagnostics
To diagnose popliteal vein thrombosis, the doctor performs a physical examination of the affected area and checks the person's heart rate. To clarify the diagnosis, the doctor may refer the patient to:
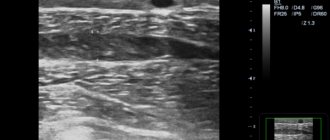
Ultrasound
The doctor may use an ultrasound to examine the popliteal and calf areas and check for signs of a blood clot. Ultrasound uses high-frequency sound waves to create images of the inside of the veins.
CT scan
CT scan takes pictures of internal organs. Your doctor may use CT scans to check for blood clots in your veins. The doctor may also check the chest for signs of TE, which can happen when a blood clot travels to the lungs.
D-dimer test
This test requires blood to check the level of D-dimer, a type of protein that can be an indicator of blood clotting. However, this test can sometimes give false-positive results, especially if the person has previously had VTE or has certain medical conditions, including:
- rheumatological;
- heart failure;
- cancer;
- inflammation.
Superficial vein thrombosis
ATTENTION! Deep vein thrombosis is dangerous due to the detachment of a blood clot and its migration into the pulmonary artery (pulmonary embolism), which most often leads to serious consequences or instant death!
Superficial veins are affected by thrombosis most often with varicose veins. Blockage of the vessel is accompanied by inflammation of the surrounding tissues. That is why the terms “thrombophlebitis” (phlebitis - inflammation of a vein), “varicothrombophlebitis” (inflammation of varicose veins) are used for this type of thrombosis.
Usually, in the area of varicose veins on the lower leg, pain and redness appear along the vein; in the area of redness, the vein itself is palpated as a dense, painful “cord”. There may be a slight increase in body temperature. In general, thrombophlebitis of the superficial veins is not dangerous; there is no detachment of a blood clot with pulmonary embolism (with the exception of inflammation of the great saphenous vein on the thigh and the small saphenous vein in the popliteal region, this will be discussed below). With adequate treatment, the inflammatory phenomena subside, and the patency of the veins is partially or completely restored over time.
The great saphenous vein (GSV) runs under the skin from the ankle joint along the inner surface of the leg to the groin fold. In the groin it flows into the deep femoral vein. That is why thrombophlebitis of the GSV is dangerous due to the transition of thrombosis from the superficial (GSV) to the deep (femoral) vein - ascending thrombophlebitis of the GSV. But thrombosis of the femoral vein is dangerous due to the detachment of a blood clot and pulmonary embolism. Therefore, if there are signs of GSV thrombosis (redness, pain along the inner surface of the thigh), you should urgently consult a surgeon or call an ambulance. Such patients are hospitalized and, if there is a threat of thrombosis spreading to the femoral vein, the GSV is ligated closer to the groin - this is a simple operation under local anesthesia.
A similar situation, but much less frequently, occurs with thrombophlebitis of the small saphenous vein (SSV). It runs along the back of the leg and drains into the popliteal (deep) vein in the popliteal fossa.
How does the venous system of the legs work?
Relatively speaking, the veins in the legs form two levels - superficial and deep.
Superficial veins provide only about 10% of venous blood flow, but they perform a very important function. In addition to collecting blood and moving it to the heart, these veins can act as a kind of reservoir, which, if necessary, can receive blood from the deep veins. Thus, the load on the veins is regulated by internal mechanisms. Veins from the deep and superficial layers are connected to each other by so-called perforating veins. Due to this, balance is maintained in the venous system.
Superficial veins are at risk of excessive stretching: if a person moves little, eats poorly, is overweight or simply has a hereditary predisposition, then the blood flow slows down and the vein wall stretches. Special valves that block the reverse flow of blood do not close tightly, and we are talking about varicose veins. Deep veins are located in the thickness of the tissues and ensure that the main volume of blood moves to the heart. The surrounding muscles maintain the tone of these vessels and facilitate blood flow, so the deep veins are not susceptible to varicose veins.
Deep vein thrombosis
Deep vein thrombosis is a more severe disease, usually requiring the patient to remain in the hospital.
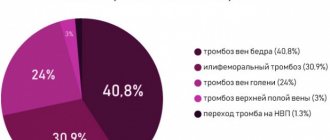
There are deep vein thrombosis of the leg, popliteal vein, femoral vein, iliofemoral (ileofemoral) thrombosis. Often there is damage to thrombosis of several sections (for example, the popliteal and femoral veins, deep veins of the leg and popliteal vein, etc.).
Deep vein thrombosis manifests itself primarily as swelling and moderate pain. Moreover, the higher the level of thrombosis, the more pronounced the edema. Thus, with thrombosis of the deep veins of the leg, there may be moderate swelling of the leg, sometimes the swelling is so insignificant that it is detected only when measuring the circumference of the leg (compared to the healthy leg). With thrombosis of the femoral or iliac (continuation of the femoral) veins, the entire leg, up to the groin, and in severe cases, the lower part of the abdominal wall swells.
In the photo - the left lower limb is cyanotic, thickened to the groin - deep vein thrombosis at the level of the iliofemoral segment (ileofemoral thrombosis).
Thrombosis, as a rule, is unilateral, so only one leg swells. Bilateral edema is observed with thrombosis of the inferior vena cava, deep vein thrombosis in both legs (which is quite rare).
Another symptom of thrombosis is pain. It is usually moderately expressed, pulling, sometimes bursting, is relatively constant in nature, and can intensify in a standing position. In case of deep vein thrombosis of the leg, the Homans, Lowenberg, Luvellubri, Meyer, Payra symptoms are positive.
With deep vein thrombosis, there may also be a slight increase in temperature, increased venous pattern, etc.
Symptoms
They do not make themselves felt immediately, but as the blood clot grows. Often, the presence of the disease is discovered only if a blood clot breaks off and enters the lungs. The most striking symptoms include:
- bursting pain in the legs, which appears when walking and disappears when the lower extremities are elevated;
- cyanosis of the skin;
- frequent swelling in the leg area (thigh, foot, calf or calf muscle);
- sore calves;
- increased temperature of the calf muscle (heat flush);
- brown skin tone (late stage).
Treatment of thrombophlebitis of superficial veins
The main therapeutic measures are reduced to elastic compression (elastic bandage or compression hosiery) and the prescription of medications.
Medicines used include phlebotropic drugs (detralex, phlebodia), antiplatelet agents (thrombo-ACC), and anti-inflammatory drugs (Voltaren). Lyoton-gel is applied topically.
All patients require venous ultrasound to exclude concomitant deep vein thrombosis and clarify the prevalence of superficial vein thrombophlebitis.
Treatment of deep vein thrombosis
In almost all cases, deep vein thrombosis is treated in a hospital. An exception may be deep vein thrombosis of the leg, provided there is no threat of thromboembolism. The danger of thromboembolism can only be determined by ultrasound examination.
If deep vein thrombosis is suspected, the patient should be hospitalized immediately. In the hospital, an examination is carried out to clarify the prevalence of thrombosis, the degree of threat of pulmonary embolism, and treatment is started immediately.
Anticoagulants (anticoagulants), antiplatelet agents, anti-inflammatory drugs, and phlebotropic drugs are usually prescribed.
In case of massive thrombosis, in the early stages it is possible to carry out thrombolysis - the introduction of agents that “dissolve” thrombotic masses.
If there is a threat of thromboembolism, when the thrombus is attached to the vessel wall only in some part, and the tip of the thrombus “dangles” in the lumen of the vessel (floating thrombus), thromboembolism is prevented (installation of a vena cava filter, plication of the inferior vena cava, ligation of the femoral vein, etc. ).
The consequences of deep vein thrombosis vary. With a small thrombosis on the lower leg there may be no consequences. With massive thrombosis, especially “high” (at the level of the hip or above), swelling of the leg may persist for a long time, and in severe cases there may be trophic disorders, even the appearance of ulcers (post-thrombophlebitic disease (PTSD)). Therefore, after deep vein thrombosis, the patient is prescribed treatment for a long time in the form of elastic compression (special stockings), indirect anticoagulants (warfarin under the control of blood clotting), and other drugs.
You should see a phlebologist for at least six months after thrombosis.
In case of recurrent thrombosis, a genetic study is carried out; if the tests are positive, the issue of lifelong prescription of anticoagulants is decided.
Causes of thrombosis in the superior vena cava system
The causes of thrombosis in the superior vena cava system are basically the same as other venous thrombosis. It may also develop as a complication of venous catheterization (cubital, subclavian catheter), sometimes arising as a result of prolonged compression or uncomfortable position of the upper limb (for example, during sleep).
The most common is thrombosis of the axillary or subclavian vein (Paget-Schrötter syndrome). Within 24 hours, swelling of the entire upper limb occurs with cushion-like swelling of the hand. There may be slight bursting pain. The color of the limb is unchanged or slightly cyanotic.
Prevention
Doctors usually prescribe anticoagulant drugs to people at high risk of blood clots, those recovering from certain types of surgery, or those who have previously had VTE. People taking anticoagulant medications should take them as directed.
A person can also reduce their risk of VTE by:
- wearing compression stockings;
- maintaining a healthy weight or losing weight as needed;
- regular exercise;
- getting up and moving around every 1-2 hours where possible;
- changing body position or bending legs from time to time;
- consuming large amounts of water;
- avoiding crossing your legs for long periods of time;
- stopping for breaks or stretching and walking every hour or so if you are traveling by car, train, bus or plane;
- quitting smoking.