In neurological practice, dizziness (vertigo) is one of the most common complaints of patients. For older people, the feeling of disorientation in space can become a serious problem: the risk of falls and injuries increases, the condition is often accompanied by phobias, depression, and deterioration of auditory and visual functions.
You can get rid of this unpleasant syndrome at any age. To do this, it is important to establish the causes of dizziness, especially since sometimes they turn out to be dangerous diseases that can be fatal. Complex diagnosis and timely treatment can help avoid severe complications.
How does dizziness manifest?
We recommend
“How to care for a bedridden elderly person” More details
During dizziness, it seems to a person that not only his head is spinning, but that he himself is spinning, or that the objects around him are spinning. When dizziness occurs in older people, nausea may occur, a feeling similar to intoxication and other unpleasant symptoms may occur, including loss of consciousness and falling.
Old people begin to blur before their eyes not only from external influences, but also due to the occurrence of diseases. Perhaps any person over the age of sixty has at least once felt suddenly dizzy. If this happens regularly, it becomes a serious problem that interferes with a normal life. In order to properly deal with the disease, it is important to determine the causes of its occurrence.
What is dizziness?
True dizziness or vertigo is a condition during which patients have a feeling of rotation of surrounding objects around them or a false sensation of their own movement or rotation.
An example of true dizziness, but not in any way related to the disease, is the dizziness that appears in people after riding a carousel, when, after an abrupt stop, they continue to see the movement of surrounding objects relative to themselves, as if the carousel were still in motion.
In most cases, the occurrence of true dizziness is a symptom of diseases of the system of control of balance and body position in space. This system includes the eyes, the vestibular apparatus of the inner ear, and sensory receptors in the human muscles, joints, and bones. Very often, dizziness, which is caused by a disruption in the balance system, is accompanied by nausea and vomiting.
Causes of dizziness in older people
Why might an elderly person feel dizzy? Most often, this is an age-related manifestation, caused by problems with the vestibular apparatus, neurological abnormalities, vascular diseases, and damage to nerve cells. Here are some of the most common causes of dizziness in older people:
- Consequences of injury.
- Sudden changes in pressure.
- Chondrosis of the cervical spine.
- Brain tumor.
- Diabetes.
- Arrhythmia.
- Ischemic disease.
- Damage to the eardrum.
- Meniere's disease (fluid accumulation in the inner ear).
- Benign tumor of the auditory nerve (neurinoma).
- Depression, fatigue, lack of sleep.
But the main thing that causes dizziness in older people is:
1. For 30–35% of cases - BPPV (benign positional paroxysmal vertigo). In older people, this is usually a consequence of degenerative changes in the area of the inner ear. The receptors of the vestibular apparatus are irritated by microscopic deposits (otoliths), resulting in dizziness. More often, older people feel such symptoms when they wake up in the morning.
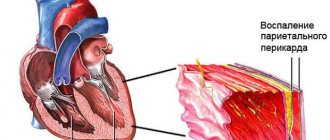
2. Diseases of the cerebral vessels, so-called cerebrovascular diseases, and atherosclerosis. A characteristic manifestation of these ailments is insufficient blood supply to the brain due to partial damage to blood vessels. This is a very dangerous condition, and dizziness with it is the most harmless symptom.
3. Poor blood circulation in the brain (stroke). According to statistics, stroke occurs in 450 thousand people in the world every day, and over 80% of them are old people. One of the manifestations of a stroke is dizziness, which can recur in a person even after undergoing a course of treatment.
4. Drug abuse (polypharmacy). Taking a large number of drugs at the same time increases the risk of adverse symptoms. It is impossible to list at once all the pills that cause dizziness in older people. Typically these are heart medications, blood pressure medications, painkillers (analgesics), antibiotics, beta blockers, diuretics, non-steroidal anti-inflammatory drugs, tranquilizers and antidepressants, sleeping pills, anti-seizure medications.
We recommend
“Lonely elderly people: how to help them” More details
5. Dizziness in elderly people with normal blood pressure is rare; rather, the cause of mild weakness and faintness is too high or too low blood pressure.
6. Weakened (due to old age) vestibular apparatus. This can cause not only a feeling of unsteadiness, but also dizziness in older people.
7. There are a number of concomitant diseases for which you have to take a large number of medications (diabetes mellitus, Alzheimer's and Parkinson's disease). Then the cause of dizziness in the elderly can be both medications and the disease itself.
8. Many older people have a very difficult time psychologically and emotionally experiencing the changes in the body that come with age. They are afraid of losing consciousness or falling if they suddenly feel dizzy. Attacks of anxiety and even panic can cause so-called psychogenic dizziness, and with them comes chills, arrhythmia, general weakness, lack of air and faintness.
A serious problem that requires treatment is severe dizziness in older people with a weak vestibular system. Objects seem to be moving in a circle; a person cannot clearly perceive their outlines. This is a common occurrence in older people with hypertension. There are also other symptoms:
- spots before the eyes;
- feeling of blindness;
- feeling that the head has become heavy;
- feeling as before loss of consciousness;
- weak legs and arms, apathetic state.
Sometimes isolated manifestations of such symptoms occur, then this most likely means that the person is simply overtired. After rest, the unpleasant feeling will pass.
However, such signs should not be ignored if they occur after a stroke or, for example, during menopause. This has serious health consequences. An elderly person may become frightened during an attack, faint, or injure himself - all this is very unsafe.
Even one of the listed symptoms is a reason to immediately consult a doctor. The reasons for poor health must be found out. Let a therapist, endocrinologist, or neurologist examine you. The process can be complex and lengthy; you will have to examine the central nervous system and other organs and take the necessary tests.
Recommended articles on this topic:
- Boarding home for the elderly: features and rules of choice
- Low blood pressure in older people: causes, symptoms and treatment
- Health of the elderly: old age is not a problem
Semiotics of systemic and non-systemic vertigo
You should always remember that when complaining of “dizziness,” different patients understand this word as completely different subjective sensations. Therefore, each time it is necessary to clarify what exactly is bothering the patient. It is necessary to invite the patient to describe his feelings in ordinary words - without using any special medical terms or figurative comparisons. This is not always easy, and the greatest difficulties are experienced by patients with a low level of education, cognitive disorders, especially elderly patients. However, one should not be content with the patient’s explanation as “he’s spinning and that’s it,” or the like. An attempt to understand the patient’s subjective sensations is the first and very important step in diagnosing the type, topical diagnosis and, ultimately, establishing the cause of dizziness.
In Russian neurology, it is customary to distinguish between systemic and non-systemic dizziness. The first always reflects dysfunction of the vestibular analyzer or disruption of its connections with the visual system or cerebellum. Patients describe vestibular (systemic) vertigo as the illusion of objects rotating in front of the eyes or the illusion of the body rotating around its axis (rotational vertigo, vertigo), or as a feeling of “sinking” or “flying.” Systemic dizziness is always extremely unpleasant, usually accompanied by a strong vegetative reaction (change in skin color, tachycardia or bradycardia), nausea, and vomiting. Very often, systemic dizziness, especially when occurring for the first time, is also accompanied by severe reactive anxiety. An objective indicator of the systemic nature of dizziness is nystagmus, which is always detected in the patient during dizziness, and often persists after it [5, 11, 14, 16].
In contrast to systemic, non-systemic dizziness is a very heterogeneous group of subjective sensations in pathophysiology and etiology.
The most common types of non-systemic dizziness include the following [3, 14–16]: • feeling of impending fainting: general weakness, lightheadedness, darkening in the eyes, “spots” before the eyes, etc. As a rule, it occurs only in a standing position, less often when sitting, passes or decreases when taking a horizontal position; • a feeling of instability, staggering when walking, objective difficulties in maintaining balance or fear of losing balance and falling. These complaints also occur only in an upright position; • difficulty concentrating, lack of concentration, “fog in the head,” feeling slightly intoxicated.
As can be seen from the above, the word “dizziness” refers to very different phenomena, which is acceptable from the standpoint of the rules of the Russian language, but should not mislead clinicians. For the clinician, “true” dizziness is one that meets the criteria for systemic dizziness.
First aid for severe dizziness in an elderly person
Here's what to do if there are complaints of weakness and dizziness in older people:
- put the person horizontally as soon as possible;
- ensure air flow into the room;
- eliminate possible sources of noise: loud music, radio, TV;
- remove too bright light (but there should be enough lighting).
If the person is dizzy but not vomiting, give the person water or tea with sugar. You can wipe your face with a damp cloth (not too cold). Atropine (0.1% solution, 8–10 drops) helps well. If the patient's condition does not improve within an hour, call an ambulance.
Often, older people immediately experience dizziness and nausea, and black spots appear before the eyes. At the same time, the person turns pale, body temperature drops. Such symptoms can be heralds of a hypertensive crisis, and if you do not quickly call an ambulance, it will lead to myocardial infarction.
It is also worth paying attention if a person experiences speech impairment, numbness in half of the face, headaches, or fainting. All these are signs of a cerebral stroke, and if doctors are not called urgently, the life of the pensioner will be threatened.
We recommend
“Interests of older people: how to improve the life of a pensioner” Read more
What is unsteadiness of movements?
Unstable movements – permanent or temporary loss of coordination. If they occur systematically, this indicates the presence of abnormal disorders in the body. Extra-systemic indicate that inflammatory processes are occurring in the body.
Most often, unsteadiness of walking manifests itself in combination with other symptoms:
- headache;
- unexplained sudden weakness;
- tingling in the legs;
- dizziness.
To better understand, it is necessary to know why a person may stagger when walking and why this is so important.
Movement is achieved through a healthy bone structure, developed muscles and healthy joints. The cerebellum is the part of the brain responsible for coordination; it is also controlled by vision and the vestibular apparatus.
Impulses pass through the spinal cord, sending a signal to the lower parts of the body that a movement needs to be performed. Only after this the muscles begin to work.
When these impulses are disrupted, the entire system is disrupted. This is where the gait disorder comes from. A transmission failure causes the legs to become unresponsive.
Failures in the musculoskeletal system lead to exactly the same result. The legs cannot correctly carry out the necessary “commands”.
If the functioning of the cerebellum is disrupted, the impulse itself does not reach, therefore, the command does not arrive at all. Consequently, a person cannot move, his legs do not obey.
Diagnosis of dizziness in older people
The success of treating dizziness in older people depends on correct diagnosis. Often the cause of dizziness is changes in the functioning of the brain. In this case, it is necessary to conduct appropriate research. Surveys of this kind are carried out according to the following scheme:
- Determine what type of dizziness is.
- Find the reasons for its appearance.
- The presence of neurological or ENT symptoms is determined.
- Additional methods are used to study the patient’s condition, depending on what pathologies were identified during the examination and interview.
1. History taking and external examination.
First you need to make sure that you really have dizziness. Old people often mistake one condition for another and may mistake nausea or blurred vision for dizziness.
An examination is very important; you need to take a closer look at how the person’s coordination of movements is, and whether the reflexes work normally. You should understand why weakness and dizziness occur in older people, what factors influence the development of the disease, and how it progresses.
If the head begins to feel dizzy gradually, this is classified as dizziness of central origin, and if suddenly and quickly, this is classified as peripheral. The latter are characterized by tinnitus and poor hearing (these symptoms are called local disorders). Central vertigo is accompanied by damage to the cortex and brain stem. A general serious condition with frequently recurring vomiting are signs of vestibular disorders.
To identify the diagnosis, the patient is asked to change the position of the head, for example, tilt it to the left or to the right. If the head becomes more dizzy when bending over, then we are talking (most often) about benign dizziness in older people, the cause of which is a weak vestibular apparatus.
Through a survey, they will find out what autoimmune or inflammatory diseases, intoxications (medicines or alcohol), and head injuries have been suffered. Check to see if the person being examined has nystagmus. Nystagmus is an oscillatory movement of the eyes independent of the patient. They study the spontaneous form of nystagmus (caused by gaze), when a person first looks straight ahead and then moves his eyes to the side.
Another diagnostic method is the Hallpike test. The patient is placed on the couch in a sitting position, he looks to the right, turning his head about 45 degrees. Holding the person by the shoulders, he is asked to quickly lie on his back so that his head hangs off the couch. The same is repeated by turning the head to the left.
An otolaryngologist examines the outer, middle, inner ear, eardrum, removes wax plugs, checks for infections (acute or chronic), and finds the consequences of injuries.
2. Laboratory and instrumental diagnostics.
CT and MRI are prescribed to ensure the absence of neoplasms and demyelinating processes. Structural pathologies (congenital or acquired) are identified. It may be necessary to take an X-ray of the skull (if there is an assumption that the person has new or old fractures).
We recommend
“Adaptation of older people: in modern society and boarding homes” Read more
The cause of weakness and dizziness in older people may be vascular dysfunction. In case of such suspicions, Doppler ultrasound of the cervical and cephalic great vessels is performed.
A complete blood test will help rule out the possibility of infection. If a pathogen is found, antibodies are determined for it.
If there is concomitant hearing impairment, the patient undergoes pure-tone audiometry. A person drinks Glycerol, after which one can notice better speech perception and recognition of low-frequency sounds. If such signs are found, then we are talking about Meniere's disease, which, as a rule, is accompanied by dizziness.
Dizziness against a background of apathy, hypochondria, accompanied by a decrease in mental activity and causeless painful health, indicate that the patient has a diagnosis of a psychiatric or neurological nature.
Dizziness in the daily practice of a doctor
The problem of diagnosing and treating vestibular disorders is one of the most pressing in modern medicine, which is determined by the high incidence rate and insufficient effectiveness of existing treatment methods. Among the reasons for visiting doctors of various specialties, it is 3–4% and 10%, respectively, to otolaryngologists and neurologists [1]. In a survey of more than 20 thousand people aged 18 to 64 years, it was found that over the past month more than 20% have experienced dizziness, of which more than 30% have suffered from dizziness for more than 5 years [2]. The prevalence of dizziness in the population is about 25%, and among the elderly - 80% [3].
Dizziness is divided into vestibular and non-vestibular, otherwise it is interpreted as systemic or non-systemic. It is known that systemic dizziness is associated with irritation of certain areas of the vestibular analyzer and, depending on the level of damage, can be peripheral or central. Peripheral vestibular vertigo (vertigo) occurs when the sensory elements of the ampullary apparatus and vestibule, vestibular ganglion and nerve conductors of the brain stem are damaged. Central vestibular vertigo occurs when there is damage to the connection with the vestibular nuclei in the brain stem, disruption of connections with the cerebellum, medial longitudinal fasciculus, oculomotor nuclei and their own connections, disruption of the vestibulospinal and vestibuloreticular connections (tract), as well as connections with the cerebral cortex [4] .
The most common cases of systemic dizziness can be divided into three groups:
1) dizziness accompanied by hearing loss; 2) dizziness not accompanied by hearing loss; 3) dizziness with central neurological symptoms [5].
In the event of acute rotational vertigo, it is important to exclude life-threatening conditions - cerebral circulatory disorders in the vertebrobasilar arterial system, the symptoms of which vary and depend on which artery is occluded.
In patients with lesions in the inferior cerebellar artery, isolated rotational vertigo with fluctuating hearing loss and/or tinnitus, simulating an attack of Meniere's disease, may be observed 1–10 days before the development of cerebral infarction. Typically, dizziness during a stroke in the vertebrobasilar arterial system is combined with other neurological symptoms. However, a small lesion in the area of the cerebellar nodule or patch, the area of the exit of the VIII nerve root between the pons and the medulla oblongata, and/or the vestibular nuclei can cause isolated vertigo without accompanying manifestations. Less commonly, such symptoms can occur with damage to the dorsal insular cortex of the flocculus, and in the latter case, gaze-induced nystagmus develops [6].
The most common signs of central damage to the vestibular system are: 1) vertical nystagmus; 2) nystagmus, changing direction; 3) atypical nystagmus (especially downward) in the head shaking test; 4) asymmetric oculomotor dysfunction; 5) severe postural instability with falls. Most of these symptoms have high specificity but low sensitivity [7].
One of the tools for the differential diagnosis of central and peripheral vertigo is the Halmagi test (head impulse test) and the head shaking test, identifying vertical squint deviation (skew deviation), not associated with damage to the oculomotor nerves or their nuclei [8].
The combination of a negative Halmagi test, vertical strabismus (skew deviation), changing the direction of nystagmus and a violation of smooth vertical tracking allows us to diagnose cerebrovascular accidents in the brain stem with 100% sensitivity and 90% specificity. The head rotation test is significant for lesions in the posterior cerebellar artery basin, but has limitations and can be positive in case of blockage of the anterior cerebellar artery with the formation of a focus in the cerebellar flocculus, vestibular nuclei or the exit zone of the VIII nerve [9–12].
According to various authors, indications for neuroimaging in patients with isolated rotational vertigo are:
1) old age; 2) the presence of risk factors for vascular diseases in combination with a normal head rotation test; 3) gaze-induced nystagmus, changing direction; 4) severe ataxia with falls; 5) a combination of acute dizziness with a first-time headache, especially of the occipital localization; 6) the presence of risk factors for vascular diseases in combination with acute hearing loss [13, 14].
Clinical example 1. Patient V., 42 years old. She went to the clinic with complaints of attacks of rotational dizziness lasting up to 2–3 hours, with a feeling of objects being displaced from right to left during an attack; occur suddenly, for no apparent reason. Before an attack of dizziness, there is a feeling of “fullness” in the left ear, which disappears soon after the dizziness stops. She reported three such attacks in total.
7 months ago I consulted a neurologist with complaints of moderate noise in the left ear and slight hearing loss, which arose suddenly, against the background of complete health. Pure-tone audiometry was performed - sensorineural hearing loss of the 1st degree. After the treatment (choline alfoscerate, B vitamin complex, deproteinized hemoderivative of calf blood), she noted a complete regression of the noise; audiometry control was not carried out.
On examination there are no neurological symptoms, vestibular function at rest is compensated. Magnetic resonance imaging of the cerebellopontine angles and internal auditory canals without pathological changes. Pure-tone audiometry - increasing hearing thresholds on the left at low frequencies up to 35 dB, with a conductive component.
Diagnosis: Meniere's disease, classic form.
When making a final diagnosis of Meniere's disease, one should adhere to the modern concept of "obvious" Meniere's disease:
1) two or more spontaneous attacks of systemic dizziness lasting from 20 minutes to 12 hours; 2) audiologically confirmed hearing loss (sensorineural) at low and medium frequencies during or after an attack of systemic vertigo; 3) fluctuating auditory symptoms: hearing, subjective noise, feeling of fullness in the ear; 4) absence of other causes of systemic dizziness [16].
Acute vestibular syndrome (vestibular neuronitis and labyrinthitis) is defined by a sudden attack of intense systemic dizziness. Depending on the level of damage, hearing loss and tinnitus may occur. As a rule, the onset of symptoms is preceded by a viral illness. With these diseases, dizziness begins gradually, intensifies over several hours, and then “mild” dizziness persists for the next few days or weeks. Dizziness persists at rest, but may subjectively intensify with changes in body position. Along with dizziness, nausea, vomiting, increased sweating, and pallor are present [17].
A labyrinthine fistula is characterized by an attack of systemic dizziness or oscillopsia that occurs due to a sharp strong sound, the Valsalva maneuver, or changes in pressure in the external auditory canal, but does not depend on changes in head position [18].
Clinical example 2. Patient M., 32 years old, complains of a constant feeling of slight instability, heaviness in the head, dizziness when throwing the head back, and sometimes wakes up at night from a pronounced sensation of rotation. 3 days ago he was discharged from the neurological department, where he was diagnosed with a transient ischemic attack in the vertebrobasilar arterial system. For the first time, an attack of dizziness occurred acutely in the morning when getting out of bed, and was accompanied by palpitations, weakness, vomiting, and cold sweat. He underwent a course of treatment with vascular and neurometabolic drugs with slight improvement.
There are no focal symptoms in the neurological status. The Disc-Hallpike test on the left is a geotropic nystagmus with a rotatory component lasting 40 seconds and a latent period of 5 seconds.
Diagnosis: benign paroxysmal positional vertigo on the left (canalolithiasis of the posterior semicircular canal). After performing the Epley maneuver twice, there was complete regression of symptoms.
Benign paroxysmal positional vertigo (BPPV)
Symptoms: the occurrence of systemic dizziness when changing the position of the head: turning in bed, throwing the head back or bending forward. The duration of the episode, as a rule, is no more than a minute.
The duration of the disease varies from several days to several years, but is more often calculated in days. BPPV occurs approximately twice as often in women. With a long course of the disease, patients report changing their lifestyle and their usual actions, so as not to provoke an attack of dizziness. Many people note an imbalance in the interictal period; a number of patients experience a feeling of heaviness in the head and nausea [16].
To diagnose this condition, special positional tests are performed: Dix–Hallpike for diagnosing BPPV of the posterior semicircular canal and McClure–Pagnini for diagnosing BPPV of the horizontal semicircular canal [18]. The diagnosis of BPPV is made with a positive Dix-Hallpike test. Nystagmus that occurs during the study has a latent period of 5–20 seconds (very rarely - up to 1 minute). Dizziness and nystagmus provoked during the test decrease gradually and stop within 60 seconds. Direction of nystagmus: towards the sore ear.
If the Dix-Hallpike test is negative, it is recommended to perform a test for the lateral (horizontal) semicircular canal of McClure-Pagnini [17].
One of the most common complaints in patients with migraine (9–14%) is dizziness. It can last from a few seconds to several days, and may not be accompanied by a headache [19].
Diagnosis criteria for vestibular migraine:
1) episodic vestibular symptoms; 2) migraine according to IHS (international headaches society) criteria; 3) at least two of the following migraine symptoms occurring during an attack of dizziness: migraine headache, photophobia, sound sensitivity, or visual or other aura; 4) other causes of vestibular vertigo are excluded [19].
In the rapid diagnosis of rotational vertigo, an internist can be helped by the scheme “Acute systemic vertigo (without other neurological symptoms)” (Fig.) [20].
Treatment of acute vestibular syndrome involves the use of antiemetics and vestibular suppressants. The action of the latter is aimed at reducing the asymmetry of vestibular tone and, thus, alleviating dizziness. However, their use is limited to a few days, since the drugs slow down the formation of compensatory mechanisms in acute peripheral damage to the vestibular apparatus. The main groups of drugs used for acute dizziness: anticholinergics, antihistamines, antidopaminergics and benzodiazepines.
From the anticholinergic group, centrally acting drugs are used that act on muscarinic receptors, improving movement tolerance. The most effective is scopolamine (M3 and M5 receptors), but the duration of its use is strictly limited due to the development of dependence. Side effects: dry mouth, mydriasis, accommodation paresis, sedation, decreased reaction speed.
Among the antihistamines, H1-blockers are used, such as diphenhydramine (Diphenhydramine), cyclizine (Valoid), dimenhydrinate (Dramina), meclozine (Bonin) and promethazine (Pipolfen). The mechanism of action is based on inhibition of activation of central cholinergic connections. Additionally, they have an anticholinergic and sedative effect. Compared to anticholinergic drugs, side effects in this group are less pronounced. It should be noted that newer drugs in this group without sedation do not penetrate the central nervous system (CNS), and are therefore useless in the treatment of dizziness.
Betahistine was registered as a drug in Europe in 1970; it is a synthetic drug that has the ability to bind to H1 histamine receptors, which are located in the neuroreceptor cells of the inner ear. It has a local powerful stimulating effect, increasing the release of neurotransmitters (histamine) from the nerve endings of the receptor cells of the inner ear into the synapse. Neurotransmitters act on the precapillary sphincters, causing vasodilation of the vessels of the inner ear, increasing their permeability and thereby normalizing intralabyrinthine pressure. In addition to affecting the receptors of the inner ear, betahistine affects the receptors of the vestibular nuclei located in the medulla oblongata, reducing activity and excitability, which helps to stop dizziness.
Dopamine antagonists are used to treat nausea and vomiting in patients with acute dizziness. The antiemetic effect is due to blocking dopamine receptors in the vomiting center of the brain stem. Some antihistamines (H1-blockers), such as promethazine, have additional dopamine-blocking effects.
The action of benzodiazepines is mediated by GABA, which is a neurotransmitter that inhibits vestibular function. The most commonly used drugs are diazepam, lorazepam, clonazepam and alprazolam [21].
For more than 50 years in world medical practice, doctors of various specialties have been using the complex antihomotoxic drug Vertigoheel for the treatment of dizziness [22].
Vertigohel is a multicomponent preparation containing the pharmacologically active ingredients Anamirta cocculus, Conium maculatum, Ambra grisea and Petroleum rectificatum. Numerous studies of the mechanism of action of the drug Vertigohel suggest multi-target activity in relation to vasodilation of capillaries and thereby microcirculation.
Numerous scientific studies, including randomized clinical trials, non-interventional studies (reproducing the scheme of daily work with patients) and meta-analysis, have confirmed the effectiveness of the clinical use of Vertigoheel.
A reference controlled cohort study on 774 patients was devoted to the effectiveness and tolerability of the drug Vertigohel in comparison with dimenhydrinate for dizziness of various origins. 25 patients were prescribed the drug Vertigohel (2-3 tablets 3 times a day) or dimenhydrinate (50 mg 2-3 times a day) for a course of no more than 8 weeks. Most patients had non-vestibular vertigo (visual/somatosensory or psychosomatic disorders). Presenting symptoms also included unsteadiness in gait and standing, with a tendency to fall. The second large group was represented by patients with vestibular (systemic) vertigo with manifestations of rotational vertigo, Meniere's disease or balance disorders.
The average number of attacks, their intensity and duration decreased significantly in both groups. By the end of the course of treatment, the patients also experienced relief from accompanying symptoms: nausea, vomiting, and increased sweating. The overall result of therapy was rated as “good” or “excellent” in 88% of cases in the Vertigohel group and in 87% of cases in the dimenhydrinate group. Tolerability was rated as “good” to “excellent” in 99% of cases in the Vertigohel group and in 98% of cases in the dimenhydrinate group [23].
In the period from 2009 to 2015, we observed 89 patients aged 18 to 42 years (53 women and 36 men) with peripheral vestibular vertigo, who were recommended to take 10 drops every 15 days when acute vestibular vertigo and nausea occurred. minutes (no more than 2 hours in a row) or dimenhydrinate 50–100 mg (if necessary, every 4 hours, but not more than 400 mg per day).
All patients received both drugs, but at different time intervals. The majority of patients (83 people - 93%) rated the high effectiveness of both drugs (as "good" or "excellent"), however, all patients (89 people - 100%) noted better tolerability of Vertigohel, since the lethargy and drowsiness characteristic of dimenhydrinate did not occur .
Thus, we can recommend the use of Vertigohel to patients to relieve acute vestibular crisis at home, since the drug is highly effective and is well tolerated. Thus, Vertigohel has no known interactions with other drugs, which is especially important for the treatment of elderly patients with concomitant chronic diseases.
Literature
- Oosterveld WJ The efficacy of piracetam in vertigo. A double-blind study in patients with vertigo of central origin // Arzneimittelforschung. 2000. No. 30 (11). P. 1947–1949.
- Yardley L., Britton J., Lear S., Bird., Luxon L. Relationship between balance system function and agoraphobic avoidance // Behav. Res. Ther. 1998. Vol. 33, No. 4. P. 435–439.
- Bobrov LS, Shmyrev VI, Vasil`ev AS, Morozov SP, Rudas MS 2011, No. 1 (39). S. 115–119.
- Sheremet A. S. Dizziness as a sign of damage to the vestibular analyzer // Consilium medicum. Vertigo app. 2001. pp. 3–9.
- Burton Martin J. Dizziness: features of diagnosis and treatment // Attending Physician. 1999. No. 4. pp. 58–60.
- Savitz SI, Caplan LR Vertebrobasilar disease // N Engl J Med. 2005; 352:2618–2626.
- Lee H. Isolated vascular vertigo // Journal of Stroke. 2014; 16 (3): 124–130.
- Brodsky MC Three dimensions of skew deviation // Br J Ophthalmol. 2003, Dec; 87(12):1440–1441.
- Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis // Neurology. 2008; 70:2378–2385
- Cnyrim CD, Newman-Toker D., Karch C., Brandt T., Strupp M. Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis” // J NeurolNeurosurg Psychiatry. 2008; 79:458–460.
- Kirchner H., Kremmyda O., Hufner K., Stephan T., Zingler V., Brandt T. et al. Clinical, electrophysiological, and MRI findings in patients with cerebellar ataxia and a bilaterally pathological head-impulse test // Ann NY AcadSci. 2011; 1233:127–138.
- Park HK, Kim JS, Strupp M., Zee DS Isolated floccular infarction: impaired vestibular responses to horizontal head impulse // J Neurol. 2013; 260:1576–1582.
- Lee H, Sohn SI, Cho YW, Lee SR, Ahn BH, Park BR et al. Cerebellar infarction presenting isolated vertigo: frequency and vascular topographical patterns // Neurology. 2006; 67:1178–1183.
- Kim HA, Lee H. Recent advances in central acute vestibular syndrome of a vascular cause // J Neurol Sci. 2012; 321: 17–22.
- Lopez-Escamez JA, Carey J., Chung W.-H., Goebel JA, Magnusson M., Mandalà M., Newman-Toker DE, Strupp M., Suzuki M., Trabalzini F., Bisdorff A. Diagnostic criteria for Meniere's disease. Consensus document of the Bárány Society, the Japan Society for Equilibrium Research, the European Academy of Otology and Neurotology (EAONO), the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) and the Korean Balance Society // Acta Otorrinolaringol Esp . 2021, Jan-Feb; 67(1), 1–7.
- Halmagyi GM Diagnosis and management of vertigo // Clinical Medicine. 2005; 5: 159–165.
- Bhattacharyya N., Baugh, RF, Orvidas L., Barrs D., Bronston LJ, DC, Cass S., Chalian AA, Desmond AL, Earll JM, Fife TD, Fuller DC, Judge JO, Mann NR, Rosenfeld RM, Schuring LT, Steiner RWP, Whitney SL, Haidar J. Clinical practice guideline: Benign paroxysmal positional vertigo // Otolaryngology–Head and Neck Surgery. 2008, 139, S47-S81.
- Huh Y.-E., Kim J.-S. Bedside Evaluation of Dizzy Patients // J Clin Neurol. 2013; 9:203–213.
- Boldingh MI, Ljøstad U., Mygland A., Monstad P. Comparison of Interictal Vestibular Function in Vestibular Migraine vs Migraine Without Vertigo // Headache: The Journal of Head and Face Pain. Vol. 53, Issue 7, p. 1123–1133.
- Vanni S., Pecci R. STANDING, a four-step bedside algorithm for differential diagnosis of acute vertigo in the Emergency Department // ACTA otorhinolaryngologica ita lica. 2014; 34:419–426.
- Singh RK, Singh M. Otorhinolaryngology Clibics // An International Journal. 2012; 4 (2): 81–85.
- Vertigoheel is the first choice drug for dizziness. Materials from the Heel company // Pharmacist. 2002, No. 20.
- Wolschner U., Strösser W., Weiser M., Klein P. Treating vertigo - combination remedy therapeutically equivalent to dimenhydrinate: results of a reference-controlled cohort study // Biol Med. 2001; 30: 184–190.
O. V. Zaitseva1, Candidate of Medical Sciences K. V. Overchenko, Candidate of Medical Sciences A. F. Khirnetkina
FSBI Scientific Center of Otorhinolaryngology FMBA of Russia, Moscow
1 Contact information
* The drug is not registered in the Russian Federation.
Anti-dizziness medicine for older people
What drug treatment is used for dizziness in older people? Since the diagnosis is so common, there are a number of drugs that make attacks less frequent and have a beneficial effect on the brain. These are so-called nootropics, that is, drugs that accelerate neural processes in the brain. They are excellent for helping with memory loss, complications of mental activity, sclerosis and dementia. In addition, they can be prescribed to improve blood circulation, to combat prolonged fatigue, insomnia and depression.
Nootropics have a wide spectrum of action and are completely safe for the body. They can be given to children and prescribed to absolutely healthy people for whom maximum concentration at work is important. But you should not try to choose a drug for yourself; let a doctor prescribe it. The main nootropics are Glycine, Phenotropil, Piracetam, Cinnarizine, Bilobil.
We recommend
“Boarding home for the elderly: how to place an elderly relative there” More details
Any of these medications improves blood circulation in the vessels of the brain, strengthens the walls of blood vessels, fights hypoxia, and establishes neural connections in the central nervous system. Some drugs have a sedative effect. Medicines in this group improve cellular metabolism and activate energy processes inside cells. This increases the ability to perceive and remember information and learn. Nootropics are used to treat dizziness in older people because they improve mood and sleep, and make a person more active.
Here is a more detailed description of some nootropics:
- Piracetam is on the first step in popularity. Many people experience sleep disturbances when taking the drug, so it is not prescribed for use in the evening, only before lunch.
- Cinnarizine. It is prescribed not only as a nootropic, but also as an anti-allergy remedy. It should be borne in mind that the drug causes drowsiness, dry mouth, and disruption of the gastrointestinal tract.
- Glycine is good because it does not cause adverse reactions. A very popular drug among students, especially during study periods. The main component is gamma-aminobutyric acid, which accelerates brain function and is important for metabolic processes.
- Phenibut. Its main component is the same gamma-aminobutyric acid. This medicine may cause you to feel sleepy, especially when you first start taking it.
How else to treat dizziness in older people? Nootropics based on herbal components are also used:
- Vinpocetine. The basic component is the small periwinkle. It has a beneficial effect on brain function, improves blood circulation in areas of blood vessels susceptible to ischemia (relaxes their walls). Helps lower blood pressure.
- Bilobil. The main herbal component is ginkgo biloba. Supplies the brain with oxygen and glucose, making blood vessels more resilient in case of oxygen deficiency. Improves attentiveness, memory and learning abilities. Has a weakening effect on numbness of the limbs.
All of the above remedies and others like them should be taken for at least three months. Only after a month will the first changes be noticeable. The frequency of administration is usually one to three times a day. The treatment regimen must be prescribed by a doctor.
Noise in the head during a stroke
Stroke is an acute disorder of blood circulation in the brain. It can be hemorrhagic and ischemic.
- In the first case, a brain vessel ruptures and blood flows into the brain tissue. The patient feels as if there was a strong blow to the head, a sharp headache, loses consciousness and falls. Other symptoms depend on which part of the brain is affected.
- The second option, ischemic stroke, is based on blockage of the lumen of a blood vessel by a thrombus. As a result, the brain tissue that this vessel supplies with blood does not receive nutrition and experiences oxygen starvation. The symptoms of this condition are very diverse - from mild speech impairment, dizziness and some tinnitus to severe weakness in the limbs and their paralysis.
A stroke is an acute condition, and the sooner the patient receives quality medical care, the greater the chance that he will quickly recover. However, long-term consequences of this pathology occur in the majority of people who have suffered it. They are:
- headache;
- dizziness;
- noise in one or both ears of varying nature (humming, pulsation, shooting, clicking) and intensity.
One of the leading methods of combating stroke and its consequences is the prevention of these diseases. Reducing the risk of their development is much easier and more effective than treating them later.
Treatment of dizziness in older people with folk remedies
Along with drug treatment, it is permissible to use traditional medicine recipes. It is better to consult a doctor first so that the effect does not turn out to be the opposite. Some simple remedies:
- Sage. Brew 4 tbsp in 0.5 liters of boiling water. l. sage flowers. Leave for half an hour, you can mix with honey. Drink before meals. The decoction is a good tonic.
- Common parsley. Grind the seeds of the plant in a coffee grinder, brew 1 tsp in a glass of boiling water. crushed mass, leave overnight. In the morning, strain and take four times a day in equal parts, before meals. It stops dizziness well in older people.
- A collection of peppermint leaves, lemon balm, linden flowers and mistletoe. The herbs need to be brewed with boiling water and allowed to brew. It helps well with a weakened vestibular apparatus.
- Red clover. Brew 1 tsp in half a glass of boiling water. dried flowers, let it brew. Take 50 ml twice a day 40 minutes before meals. Helps cleanse the walls of blood vessels, activates life processes, and reduces dizziness.
- Elecampane root. Brew a pinch of crushed root in a glass of boiling water, let it brew for half an hour and strain. Take 4 times a day in equal parts. Tones, destroys infections and parasites, has a beneficial effect on the vestibular system and stops dizziness.
- Simple kelp (sea kale). Eat 1 tsp once a day. dried plant with water. Strengthens the immune system, helps cleanse toxins, normalizes the central nervous system, and stops dizziness.
We recommend
“Centers for pensioners: what they are and how to get there” Read more
- Veronica grass. Brew 1 tbsp in 250 ml boiling water. l. dried plant, infuse. Take the infusion warm, 80-100 ml before meals. Acts as a sedative and relieves dizziness.
- Onion. Scroll it through a meat grinder. The dizziness goes away if you breathe over the resulting mush. Mix chopped onion and honey in a glass jar in equal parts and leave in a cool place for 5 days. The remedy stops severe dizziness in older people and gives strength.
Basically, soothing herbal decoctions are used as herbal remedies:
- Chamomile tea with mint. Brew a tablespoon of dried herbs in a glass of boiling water and strain after 15 minutes. If you are not allergic to honey, you can add one teaspoon to your tea.
- Calming drink. Brew chamomile, mint and valerian (one teaspoon each) in 0.5 liters of boiling water and leave in a thermos for 12 hours. The best option is to prepare the decoction overnight, strain it in the morning, add honey and apple cider vinegar (one teaspoon each). Drink before meals.
- Dried ginger root is an excellent folk remedy for treating dizziness in the elderly. The root is taken in powder form three times daily before meals. Dry, powdered garlic is also a good tonic. You can take both remedies at once.
- Hawthorn relieves spasms and has a strengthening effect on the walls of blood vessels. A self-prepared infusion is much more effective than a pharmaceutical alcohol preparation. To prepare, brew one tablespoon of dry herb in 200 ml of boiling water and leave for half an hour.
- Dizziness stops after two weeks of taking plantain infusion.
You can also prepare tinctures:
- From garlic. Pour half a liter of alcohol into 300 g of garlic in a glass container and leave in a cool place for 15 days. Method of administration: add 20 drops of tincture to half a glass of milk. The product cleanses the body of toxins, fights infections, improves the functioning of the heart muscle, and relieves dizziness.
- From chestnut. Crushed chestnut buds are poured with half a liter of Cahors (preheated to 70 degrees) and kept for 15 minutes in a water bath. When it cools down, add two tablespoons of honey and a little vanilla powder. Take 50 ml before meals. Improves general condition and activates the activity of brain vessels.
Juice treatment:
- Carrot. Drink 0.5–1 glass three times a day before meals. Strengthens the immune system, relieves dizziness. An excellent remedy is a mixture of carrot, pomegranate and red beet juices (in a ratio of 3:2:2). Take the same way, 0.5–1 cup three times a day before meals. Improves the overall well-being of older people.
- Pineapple. Pineapple is a very strong antioxidant, rich in minerals and vitamins. Its juice rejuvenates the body and has a strengthening effect on the walls of blood vessels. Relieves dizziness in older people and is good for anemia.
- Juice from salad. Drink 25 ml 4 times a day if dizziness occurs due to heart failure or disorders of the central nervous system.
- Juice of young zucchini (possibly with the addition of carrot). It is taken in cases where dizziness occurs due to cardiac problems or high blood pressure.
Which doctor should I contact if I have a murmur in old age?
In most cases, when people with tinnitus seek medical help, they are diagnosed with neurological or ENT pathology. Therefore, it is advisable to visit these doctors for initial diagnosis and examination. It would be more correct to start with a neurologist.
The specialist will talk with the patient, carefully question him about his complaints, clarify what, where and how long it hurts, the history of this disease and life, and based on the data obtained, he will assume the presence of a certain pathology. To clarify the diagnosis, the patient will be sent for examination, which may include:
- clinical blood test;
- general urine analysis;
- ECG;
- angiography of cerebral vessels;
- MRI of the brain or cervical spine, as well as other research methods.
If the neurologist is convinced that the patient does not suffer from a disease of his profile, he will refer him to other specialists - an otolaryngologist, an endocrinologist, a therapist. If an organic cause of tinnitus has been ruled out, a psychiatrist can help treat it. If the neurological diagnosis is confirmed, the doctor will tell you how to treat it and order the patient to appear for a follow-up examination.
Other treatments for dizziness in older people
Dizziness in older people is best treated by a combination of medications, folk remedies and the following methods:
- Physiotherapy. Properly selected exercises strengthen the spine and stimulate the functioning of blood vessels. Regular exercise can sometimes give more significant results than taking medications.
We recommend
“Gymnastics for the elderly: the best exercises for various diseases” Read more
- Physiotherapy. Modern technologies in this area are multifaceted; water, sound, light, magnetic, and laser treatments are available. Regular implementation of these procedures has a very beneficial effect on the nervous system.
- Reflexology, in particular acupuncture. It normalizes the functioning of the central nervous system, relaxes muscles and activates blood circulation.
- Psychotherapy. The likelihood of dizziness in older people is significantly reduced if measures are taken to relieve nervous tension and anxiety.
Entering into old age will be much easier if you take care of your health in advance. The physical capabilities of the body directly depend on compliance with the daily routine, proper nutrition, intensity of exercise, and abuse of bad habits. Think about what is easier - to prevent the disease or to treat it later? Provide your body with normal functioning, do not neglect examinations if you are already about sixty. Be active, walk more, look at the world positively. Then you definitely won’t have to deal with bouts of dizziness.
Doctor's help
It is impossible to make a diagnosis yourself when it sways from one side to the other. This is done exclusively by specialists. To begin with, doctors monitor the patient’s movements using the following methods:
- observation of movements directed forward with the face and forward with the back;
- doctors watch how the patient moves in a straight line with his right and left sides;
- alternate change of step rhythm;
- comparison of walking with eyes closed and with eyes open;
- watching a person climb stairs;
- movement around an object (for example, a chair);
- making turns while driving;
- It is also suggested to walk on your toes and heels.
Based on the results, the doctor prescribes further examination and treatment:
- undergoing magnetic resonance imaging;
- X-ray;
- CT scan;
- blood donation (general analysis and biochemical);
- A biopsy of muscle tissue is performed.
In addition, the patient should be examined by other doctors:
- ENT;
- ophthalmologist;
- endocrinologist
After going through all the stages, the doctor can diagnose the patient and prescribe the necessary treatment.
You should turn to traditional medicine only after examination and consultation with a doctor.
Any medications are prescribed only by a certified specialist! All drugs are prescribed based on the individual characteristics of each organism. Medicines that help one person can cause irreparable harm to another.
Treatment in Moscow
The best treatment for vestibular disorders is considered to be exercises for dizziness or vestibular rehabilitation. Vestibular rehabilitation is carried out in many special centers, including the rehabilitation center of the Yusupov Hospital. Therapeutic gymnastics is carried out by an instructor, classes are developed individually for each patient. A preliminary examination by a neurologist will help determine the cause of dizziness, and the doctor will prescribe effective drug treatment. A neurologist will tell you what examination to undergo and how to cure vestibular vertigo during your consultation.