A high pulse with normal blood pressure is not such a rare phenomenon, requiring attention from a general practitioner and cardiologist. If the pulse pressure increases, this fact is rarely noted by the person himself before recording the indicators; usually this condition is manifested by changes in well-being, which is the reason for contacting a specialist. Often, the pulse frequency changes after physical exertion, stress and as a result of fatigue, and this symptom is accompanied by an increase in blood pressure (BP).
But this does not mean that the heart rate cannot increase without an increase in systolic pressure; it can jump even with normal tonometer readings. Today we need to figure out what a high heart rate at the same time as normal blood pressure indicates, what causes the condition, and how to deal with it.
What is "bradycardia"?
A decrease in heart rate (HR) below the established norm (60 beats per minute) is called “bradycardia”.
It can occur both in healthy people and in patients with various pathologies. Compared to tachycardia (increased heart rate more than 90 beats per minute), bradycardia is less common. It is typical for people over 60 years of age, since heart disease is more common at this age. Heart rate usually corresponds to the pulse, since with each release of blood into the aorta under pressure, rhythmic vibrations of the arterial walls occur.
What is the normal heart rate?
In adults, the heart rate should be 60–90 beats per minute (bpm); for children, normal heart rates depend on age. Thus, in babies under one year old, heart rate fluctuates between 100–170 beats/min. As the child grows up, normal heart rate values gradually decrease. By age 12–15, your resting heart rate should approach 70–90 beats per minute.
How to measure pulse?
The pulse can be measured by feeling the arteries that are located shallow to the surface of the skin and where they can be pressed against the bones. Then you can feel the movement of the vessel wall with your fingertips (Fig. 1). It occurs with every heartbeat. The pulse is measured in the following arteries: temporal, carotid, brachial, radial (at the wrist), femoral, popliteal, dorsalis pedis, posterior tibial (at the ankle of the foot).
Figure 1. How to measure pulse Source: MedPortal
Low heart rate in children: causes and consequences
A pulse below normal is detected in approximately 3.5% of children. As a rule, the pathology is caused by congenital heart defects or insufficiency of the sinus node. In children without heart disease, problems may occur due to a bacterial or viral infection. Pathogenic microbes release waste products that cause a response from the immune system and disrupt the functioning of the heart.
Some people have a low heart rate from birth, and this becomes evident at an early age. This phenomenon is called constitutional-familial bradycardia, which is hereditary.
In children and adolescents, the development of various types of arrhythmia can be triggered by excessive psycho-emotional stress and an unfavorable family environment.
Causes of bradycardia
A decrease in heart rate can occur not only with cardiac lesions, but also with non-cardiac pathologies. Common reasons for a decrease in heart rate include:
- coronary heart disease, heart defects, atherosclerotic cardiosclerosis, heart attack, myocarditis, cardiomyopathies, pericarditis;
- jaundice and kidney failure, in which toxins slow the heart's impulses;
- connective tissue diseases (rheumatism, rheumatoid arthritis, scleroderma, lupus erythematosus);
- hypothyroidism - decreased function of the thyroid gland;
- infections (diphtheria, borreliosis, syphilis, toxoplasmosis, viral hepatitis, etc.);
- disturbance of the electrolyte composition of the blood - decreased potassium levels and increased calcium;
- increased intracranial pressure due to brain tumors, stroke, trauma, developmental defects;
- lymphogranulomatosis, multiple myeloma, amyloidosis, sarcoidosis, hemochromatosis are conditions in which myocardial damage is possible.
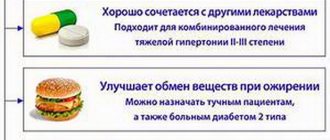
Drug-induced bradycardia often occurs. This occurs when taking or overdosing on beta blockers, cardiac glycosides, calcium channel blockers, and antiarrhythmic drugs.
The heart rate is affected by the work of the nervous system: the parasympathetic system reduces the heart rate, and the sympathetic system increases it. Reflex bradycardia occurs as a result of the influence of the parasympathetic nervous system on the sinus node. The causes of such bradycardia may be:
- diseases of the nervous system;
- gastrointestinal pathology (peptic ulcer of the stomach and duodenum, cholecystitis, cholelithiasis);
- diseases of the esophagus and diaphragm;
- low body temperature, hypothermia;
- blow to the upper abdomen (up to cardiac arrest);
- pressure on the eyeballs or neck in the area of the carotid artery;
- cough, vomiting.
When the heart rate slows, blood pressure (BP) can be normal, high or low.
Bradycardia with high blood pressure is an uncommon occurrence. It is dangerous due to respiratory arrest, loss of consciousness, risk of blood clots, insufficient blood supply to the brain and heart with the development of stroke and heart attack. The combination of hypertension and bradycardia requires special treatment approaches so as not to aggravate the slowing of the rhythm.
For newborns (especially premature ones), bradycardia can occur against the background of apnea - stopping breathing for more than 20 seconds (Fig. 2). This occurs due to the immaturity of the nervous and muscle tissue of the newborn.
Figure 2. Bradycardia and apnea in infants. Source: MedPortal
Low heart rate: what to do?
Bradycardia, that is, a decrease in heart rate, is a symptom that can be caused by both physiological characteristics of the body and dangerous pathologies. What pulse is considered normal and how not to miss the development of complications was told by a cardiologist.
The questions were answered by Nino Revazovna Malania, a cardiologist of the 1st category of the Federal State Budgetary Institution “National Medical Research Center named after. acad. E.N. Meshalkin" of the Ministry of Health of Russia, Member of the ESC (European Society of Cardiology) and RKO (Russian Society of Cardiology).
– Bradycardia – what is this condition?
– The heart is an autonomous and self-sufficient organ that works without our participation. It is forced to contract and push blood through the vessels by the so-called “pacemakers” - the sinus node and the atrioventricular node, which produce electrical impulses, under the influence of which the heart contracts.
The National Institutes of Health (NIH) defines bradycardia as a heart rate <60 beats per minute in adults other than well-trained athletes. However, in population studies, a lower threshold of <50 beats per minute is often used.
In an analysis of four population-based studies from the Netherlands, adults aged 20 to 90 years had the lowest second percentile heart rate ranging from 40 to 55 beats per minute, depending on gender and age.
Sinus pauses of 2 seconds and 3 seconds have been described during 24-hour ambulatory ECG monitoring in healthy elderly patients and distance runners, respectively. Based on the available evidence, guidelines have been developed1 where the presence of a sinus rate <50 beats per minute and/or a sinus pause >3 seconds can be used to diagnose sinus node dysfunction. The only reason to consider any treatment for sinus node dysfunction is the presence of symptoms.
– What symptoms accompany this condition?
– In the clinical picture, there are two main groups of symptoms: cerebral and cardiac. Permanent and long-term bradycardia can be manifested by fatigue, increased fatigue, lethargy, apathy, and decreased mental abilities.
The consequences of cerebral hypoperfusion are most clearly manifested: in acute disorders, sudden dizziness and confusion may occur, and in more severe cases, presyncopal (or presyncope) and syncope (or loss of consciousness) conditions, up to a full-blown picture of Morgania-Adams-Stokes attacks.
Bradycardia can lead to aggravation of coronary heart disease, arterial hypertension and chronic heart failure. Clinically, decreased tolerance to physical activity with the usual manifestations in these cases in the form of rapid fatigue and shortness of breath.
Bradycardia can become a serious problem because the heart does not pump enough oxygen-rich blood into the body. However, in some people, bradycardia does not cause symptoms or complications.
During deep sleep, the heart rate may drop below 60 beats per minute, which is physiological. And in physically active adults (and athletes), resting heart rates are often below 60 beats per minute, which is normal in this case.
– What factors can influence a decrease in heart rate?
– When collecting anamnesis from the patient, it is necessary to clarify the frequency, time, duration, timing of occurrence, factors that provoke and mitigate symptoms, on the basis of which bradycardia can be suspected. It is important to note the relationship of symptoms to medications, food, medical interventions, emotional distress, changes in body position, exercise, or other factors (urination, defecation, coughing, prolonged standing, turning the head) for the differential diagnosis.
The following factors can affect sinus rhythm and cause bradycardia:
- increased tone of the parasympathetic nervous system; increased intracranial pressure (for example, with cerebral edema, tumor, stroke);
- sclerotic changes in the muscular layer of the heart, which affects the sinus node;
- exposure to certain medications for the treatment of cardiovascular diseases (for example, beta blockers, antiarrhythmics - drugs that affect the heart rate, etc.);
- pathology of the thyroid gland (for example, hypothyroidism - decreased function of the thyroid gland);
- some diseases of the cardiovascular system (atherosclerosis of the coronary vessels, ischemic heart disease, cardiosclerosis, heart attack, endocarditis, myocarditis, post-infarction scars, etc.);
- risks of bradyarrhythmia after heart surgery (after coronary artery bypass grafting, open heart valve surgery, transcatheter aortic valve implantation, surgery for congenital heart defects, heart transplantation, after RFA treatment for cardiac arrhythmias);
- disturbance of the metabolism of minerals and electrolytes involved in conducting electrical impulses in the heart (for example, hypokalemia);
— obstructive sleep apnea syndrome (stopping breathing during sleep);
— infectious and inflammatory diseases (rheumatism, systemic lupus erythematosus);
- toxic effects (for example, lead poisoning, nicotine).
– In what cases can bradycardia be a normal variant?
– If nothing bothers a person clinically against the background of bradycardia, then this may be a variant of the norm, and the absence of clinical symptoms may indicate that the brain is adapted to such a rhythm - that is, this is a kind of “norm” for a particular person.
As I already said, during deep sleep, the heart rate can drop below 60 beats per minute, which is physiological. And in physically active adults (and athletes), the resting heart rate is often below 60 beats per minute, which is the norm in this case and is regarded as physiological bradycardia.
– What should be the reason for visiting a doctor?
– If the pulse has become <60 per minute at rest without pathological effects on the pacemaker of the heart (taking medications that affect the heart rhythm, toxic effects, diseases of the cardiovascular system), although before this it was 70-80, or you have clinical complaints (weakness, fatigue, dizziness, lightheadedness, fainting, etc.) - this may indicate serious heart problems and you should first consult a therapist for examination.
What does the general practitioner need to assess? Clinical picture of the patient and anamnesis; 12 channel ECG; Holter monitoring; echocardiography. Other additional research methods at the second stage of the examination will be carried out according to the indications of the arrhythmologist.
– What could be a critical decrease in heart rate that requires emergency care?
– Severe sinus bradycardia is considered to be a heart rate <40 per minute at rest, which can lead to the development of heart failure and is a life-threatening condition (possible development of arrhythmogenic shock, syncope, loss of consciousness). These patients are indicated for emergency implantation of a pacemaker in a cath lab.
The decision to implant a pacemaker is made by an arrhythmologist after a thorough examination of the patient based on clinical and medical data.
- 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society
2. Clinical recommendations “Bradyarrhythmias and conduction disorders” of the Ministry of Health of the Russian Federation 2021
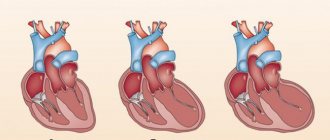
Classification of bradycardia
The work of the heart is impossible without the normal functioning of the conduction system. These are special muscle fibers that form nodes and bundles and provide coordinated contraction of the atria and ventricles of the heart. A normal rhythm is generated with a frequency of 60–90 per minute in the sinus node (SU), which is located in the right atrium. Along the internodal bundles, the electrical impulse is conducted to the atrioventricular node (atrioventricular - AV), located in the interatrial septum. From the AV node, the impulse goes directly to the muscles that provide contraction of the ventricles of the heart.
Depending on the mechanism of occurrence, bradycardia occurs:
- Sinus. Associated with a slowdown in impulse generation in the sinus node itself (Fig. 3).
- Sinoatrial, in which the transmission of impulses from the sinus to the atria is blocked.
- Atrioventricular, when there is a blockade of excitation transmission in the AV node.
Figure 3. Development of sinus bradycardia.
Source: mayoclinic.org Bradycardia can be pathological and physiological - a decrease in heart rate is typical for young athletes and during sleep. Pathological bradycardia occurs:
- acute and chronic;
- with symptoms and without clinical manifestations;
- cardiac and extracardiac (depending on the reasons).
Causes of arrhythmia
The most common causes of arrhythmia or the condition leading to its development are heart disease, high blood pressure, diabetes, smoking, excessive consumption of alcohol and caffeine, drug abuse, and stress. In some cases, the causes of arrhythmias may be an overdose of certain medications, the use of dietary supplements and herbal preparations.
Scars can occur for various reasons. The most common of these is acute myocardial infarction. Such a scar prevents the formation of an electrical impulse and/or interrupts the passage of an impulse through the heart muscle.
In a healthy person with a healthy heart, the development of a stable arrhythmia is impossible without the presence of an external trigger, such as an electric shock. This happens primarily because in a healthy heart there are no pathological substrates for the development of arrhythmias, including scar tissue.
On the other hand, in hearts with signs of arrhythmia, the formation and/or propagation of the electrical impulse may be impaired, facilitating the development of the disease.
Any of the following conditions can lead to the development of arrhythmia:
○ Inadequate blood supply
. If blood flow to the heart is reduced for any reason, this can alter the cells' ability to form and conduct electrical impulses.
○ Damage or death of the heart muscle
. Damage or death of the heart muscle leads to a change in the path of electrical impulses propagating through it.
Among the heart disease causes of arrhythmias, the following are of particular importance:
○
Coronary heart disease (CHD)
. Despite the fact that many types of arrhythmias are recorded with ischemic heart disease, the most strongly associated with it are ventricular arrhythmias and sudden cardiac death. The narrowing of the arteries occurs until, as a result of lack of blood supply, part of the heart muscle dies (acute myocardial infarction). This can affect the process of propagation of an electrical impulse throughout the myocardium: small electrical circles of excitation are formed at the border of scar tissue, which disrupt the normal functioning of the heart, causing pathologically fast heartbeat (ventricular tachycardia) and ventricular flutter or fibrillation - ineffective chaotic contractions of the ventricles.
○ Cardiomyopathy
. It manifests itself as primary stretching and thinning of the walls of the ventricles and atria (dilated cardiomyopathy) or excessive thickening and overcontraction of the walls of the left ventricle (hypertrophic cardiomyopathy). With any variant of cardiomyopathy, the efficiency of cardiac output decreases (the amount of blood ejected by the left ventricle into the aorta to nourish all organs and tissues of the body decreases), and part of the blood remains in the left and right ventricles or is thrown back into the atria and the veins flowing into them.
Heart valve diseases. Damage to the heart valves by infectious agents or due to degenerative degeneration leads to narrowing of the valve openings and/or insufficient closure of the valves, i.e. valve insufficiency. When the chambers of the heart become stretched and weakened due to inadequate valve function, the risk of developing various types of heart rhythm disorders increases.
Why is bradycardia dangerous?
A decrease in heart rate can cause heart failure, chronic attacks of bradycardia, and the formation of blood clots.
Heart failure
It rarely develops when the decrease in heart rate is significant (less than 40 per minute). Bradycardia results in insufficient cardiac output, which means that the heart can no longer supply oxygen to all organs and systems of the body at the proper level. In this case, the brain and the heart itself suffer first. The risk of developing coronary artery disease and myocardial infarction also increases, and fainting and cardiac arrest may occur.
Blood clots
With prolonged or frequently occurring bradycardia with an irregular rhythm, as a result of slowing down the movement of blood flow in the chambers of the heart, blood thickens and the gradual formation of blood clots occurs. When they enter the vessels of the brain or heart, strokes and heart attacks occur.
Chronic attacks of bradycardia
When the cause of bradycardia cannot be identified and eliminated, attacks occur that reduce the quality of life and are difficult to correct. During an attack, the patient experiences weakness, dizziness, and decreased performance. Sometimes fainting is possible.
Rare pulse with normal blood pressure: what to do?
The attending doctor decides how to raise the heart rate with medication. Pharmacotherapy is selected individually for a particular patient, taking into account existing pathologies, the severity and cause of bradycardia.
The most commonly used groups of drugs:
- sympathomimetics (adrenergic agonists);
- M-anticholinergics;
- methylxanthines.
Taking special medications is indicated when the heart rate drops to 40-38 beats per minute or less.
Bradycardia may appear in a person suffering from peptic ulcer, cholelithiasis or urolithiasis, acute glomerulonephritis, or in a patient with a sliding hernia of the esophageal diaphragmatic opening, mass mediastinal tumors, or traumatic brain injuries.
All of these drugs have a short-term effect and are used as emergency medications. There are currently no medications that can consistently increase heart rate without affecting blood pressure and without side effects on other organs and systems. That is why, with a systematic decrease in the frequency of contractions of the heart muscle, it is imperative to look for the cause of the disease. To do this, you need to consult a cardiologist, since the main measure for bradycardia is the diagnosis and treatment of the underlying pathology that causes it, and not taking drugs that temporarily increase the pulse.
However, there are situations where a low pulse with stable blood pressure is an isolated, transient case. In this case, you can increase your heart rate at home without the use of drugs.
In the absence of pathology, you can increase your heart rate by eating a piece of dark chocolate
Most often, the question “what to do if your heart rate is low at home?” Experts advise drinking strong sweet tea or coffee. However, it should be remembered that such a measure can lead to increased blood pressure, which is undesirable for hypertensive patients. This recommendation should also be taken with caution by patients with diabetes.
Several ways to increase your heart rate without medications:
- taking adaptogens, tonic tinctures (ginseng, hawthorn, rose hips, royal jelly, eleutherococcus, etc.);
- dosed physical activity;
- cold and hot shower;
- eating several slices of dark chocolate with a high cocoa content (72-75% or more).
Despite the fact that in most cases the listed methods demonstrate fairly high effectiveness, this does not mean that they are guaranteed to help cope with bradycardia.
Bradycardia is diagnosed when the frequency of contractions of the heart muscle decreases to numbers not exceeding 55–59 beats per minute.
If, against the background of a low pulse (even while maintaining the usual pressure), the patient is worried about a deterioration in health, all measures bring short-term relief or are ineffective, it is necessary to seek medical help.
Symptoms of bradycardia
Manifestations of bradycardia are caused by a lack of blood supply to vital organs: the brain, heart and lungs. Bradycardia can manifest itself (Fig. 4):
- decrease in blood pressure;
- presyncope and loss of consciousness;
- dizziness, headache;
- rapid fatigue;
- chest pain;
- shortness of breath and poor tolerance to any physical activity;
- pale skin.
Figure 4. Symptoms of bradycardia. Source: MedPortal
When to see a doctor?
If you have symptoms of bradycardia and a pulse less than 60 beats per minute, you should consult a physician or cardiologist. The doctor will determine the causes of this condition and prescribe effective treatment.
Not all bradycardia causes symptoms. However, low heart rates cannot be ignored. A repeated decrease in heart rate is the “first bell” that will force the timely diagnosis of heart disease and non-cardiac pathology, and prevent the development of dangerous complications.
Diagnostic measures
A hypertensive patient who often exhibits a small pulse during attacks of arterial hypertension should consult a cardiologist to determine the cause of the disorder. To identify concomitant diseases, you should undergo the following studies:
- electrocardiography;
- phonocardiography;
- clinical blood and urine analysis;
- biochemical analysis for hormones;
- bacteriological research.
Important! To independently monitor their pulse, patients are advised to purchase an electric tonometer that displays blood pressure and heart rate. This allows you to detect a small pulse throughout the day.
Diagnosis of bradycardia
Only a doctor can differentiate physiological or pathological bradycardia. To do this, he uses several diagnostic methods.
Auscultation
A simple diagnostic method is to listen to the heart using a phonendoscope. Auscultation of the heart allows not only to determine a rare rhythm, but also to suspect certain diseases of the cardiovascular system.
Electrocardiography
ECG is a method of instrumental diagnostics of the heart, which records not only heart rate, but also helps to diagnose cardiac causes of bradycardia (myocardial ischemia and infarction, sinus node pathology, AV block). This is important for effective therapy. In some cases, daily ECG monitoring is necessary - a Holter study.
Phonocardiography
Phonocardiography (PCG) is a method of hardware diagnostics of sound phenomena that are created during the work of the heart. The study is carried out in conjunction with an ECG. At the same time, the heart sounds that are created during the operation of the valves, as well as additional noise, are assessed.
To diagnose the causes of bradycardia, the doctor may also prescribe:
- EchoCG - ultrasound examination of the heart;
- blood test for markers of damage to the heart muscle (troponins, creatine kinase);
- study of inflammation indicators (C-reactive protein, rheumatic tests, markers of collagenosis);
- blood test for thyroid function indicators (TSH, T4, T3);
- study of blood electrolytes (potassium, magnesium, calcium, sodium);
- biochemical blood test (glucose, bilirubin, cholesterol, creatinine, etc.).
How to treat
Before starting treatment, it is necessary to undergo a medical examination. Only after identifying the underlying cause can the attending physician prescribe therapy. The main methods include:
- drug therapy – taking medications. In our center, the Federal Scientific and Clinical Center for Medical and Biological Agency, patients are offered outpatient or inpatient treatment. If the patient is old, it is better to assign him to the therapeutic department, where he will be under the constant supervision of doctors and nurses. personnel;
- therapeutic and preventive procedures - moderate physical activity, adherence to a daily routine, taking herbal medicines as prescribed by a doctor for the purpose of prevention;
- surgical intervention - radical measures are resorted to when a concomitant disease affects the decrease in pulse rate. These include implantation of a pacemaker, elimination of certain rhythm disturbances that can lead to bradycardia. Only after all the necessary examinations and tests can the doctor recommend surgery. The cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency has a surgical department. Doctors with many years of experience perform complex open-heart surgeries.
Treatment of bradycardia
Not all bradycardia requires treatment. Only a doctor can determine the need for treatment by excluding physiological causes of a decrease in heart rate.
Conservative treatment
For conservative treatment use:
- anticholinergics - drugs that prevent the influence of the parasympathetic nervous system on the heart;
- adrenaline analogues - drugs that stimulate heart rate;
- antiarrhythmic drugs.
Treatment is carried out with tablets and injections. Their doctor can prescribe them occasionally during attacks and for a long time.
Surgery
In cases where conservative treatment is ineffective or there is damage to the conduction system of the heart, surgical treatment is indicated - installation of an electrical pacemaker (pacemaker). This is an electronic device that is implanted subcutaneously in the left subclavian region and sets the necessary rhythm to the heart through electrodes (Fig. 5). The pacemaker not only stimulates impulses to contract the heart, but also controls its natural electrical activity.
Figure 5. Installation of a pacemaker for bradycardia. Source: MedPortal
Treatment with folk remedies
To treat bradycardia at home, infusions of herbs are mainly used, which reduce the tone of the parasympathetic nervous system, increase myocardial contractions, and maintain blood pressure. These are Chinese lemongrass, tartar, immortelle, yarrow, walnuts, a mixture of lemon, honey and garlic and others.
Important! Treatment with folk remedies should be carried out very carefully and only after consultation with a doctor. It is possible with mild degrees of bradycardia (heart rate of at least 40), in the absence of complications and manifestations such as fainting, shortness of breath, dizziness, chest pain.
Unconventional methods of treatment
Folk remedies based on the use of medicinal herbs and plants will help increase heart rate and stabilize blood pressure.
Natural medicines from yarrow, peppermint, and lily of the valley will help raise the level of pulse contractions
You can achieve an increase in myocardial contractile activity using the following recipes:
- Lemon-garlic mixture. To prepare, you need to squeeze the juice from 5 lemons, then chop half a head of garlic, add 2 tbsp. l. honey, mix thoroughly. Leave for 24 hours, take 1 tsp. 4 times a day before meals.
- Radish juice. Remove the top of the vegetable, take out a small amount of pulp so that a cavity is formed. Add 1 tbsp to the well. l. honey, leave for 2-3 hours. Take the resulting nectar 3 times a day.
- Nut mixture. In a container, mix 1 glass of sesame oil, 500 g. chopped walnuts and 1 tbsp. Sahara. Place the sliced lemon in a separate container and pour boiling water over it. Combine the components, mix together, leave for about 24 hours in a place inaccessible to sunlight. Take 3 times a day.
The ratio of heart rate and pressure is an important diagnostic criterion in assessing the condition of a hypertensive patient, so some disorders may indicate the development of concomitant diseases. In some cases, a minor deviation is a physiological process or the body's reaction to certain medications. The course of the pathology depends on the cause of occurrence and the functional state of the vascular and cardiac systems. Timely diagnosis will help normalize the patient’s condition and slow down the progression of the disease.
Prevention
To prevent complications of bradycardia, you need to consult a specialist as soon as possible if your pulse decreases and heart rate is less than 60, and undergo a full examination to identify the causes of the condition. It is equally important to strictly follow your doctor's recommendations for treating episodic or prolonged bradycardia.
To prevent bradycardia, it is necessary to adhere to a lifestyle that reduces the risk of heart disease:
- stop smoking and drinking alcohol;
- eat well: limit animal fats, salt, caloric content of food should correspond to energy costs;
- reduce excess weight if you are overweight;
- avoid nervous stress;
- normalize blood pressure.