Pulmonary edema is a severe pathological condition associated with massive release of transudate of a non-inflammatory nature from the capillaries into the interstitium of the lungs, then into the alveoli. The process leads to a decrease in the functions of the alveoli and disruption of gas exchange, and hypoxia develops. The gas composition of the blood changes significantly, and the concentration of carbon dioxide increases. Along with hypoxia, severe depression of central nervous system functions occurs. Exceeding the normal (physiological) level of interstitial fluid leads to edema.
The interstitium contains: lymphatic vessels, connective tissue elements, intercellular fluid, blood vessels. The entire system is covered by the visceral pleura. The branched hollow tubes and tubes are the complex that makes up the lungs. The entire complex is immersed in the interstitium. The interstitium is formed by plasma leaving the blood vessels. The plasma is then absorbed back into the lymphatic vessels that drain into the vena cava. Through this mechanism, the intercellular fluid delivers oxygen and necessary nutrients to the cells and removes metabolic products.
Violation of the amount and outflow of intercellular fluid leads to pulmonary edema:
- when an increase in hydrostatic pressure in the blood vessels of the lungs causes an increase in intercellular fluid, hydrostatic edema occurs;
- the increase occurred due to excessive filtration of plasma (for example: with the activity of inflammatory mediators), membrane edema occurs.
Condition assessment
Depending on the rate of transition from the interstitial stage of edema to the alveolar stage, the patient’s condition is assessed. In the case of chronic diseases, edema develops more gradually, more often at night. This swelling can be easily controlled with medications. Edema associated with mitral valve defects, myocardial infarction, and damage to the pulmonary parenchyma increases rapidly. The condition is rapidly deteriorating. Acute swelling leaves very little time to respond.
Disease prognosis
The prognosis for pulmonary edema is unfavorable. Depends on the reasons that actually caused the swelling. If the edema is non-cardiogenic, it responds well to treatment. Cardiogenic edema is difficult to treat. After long-term treatment after cardiogenic edema, the 1-year survival rate is 50%. In the lightning-fast form, it is often impossible to save a person.
With toxic edema, the prognosis is very serious. Favorable prognosis when taking large doses of diuretics. Depends on the individual reaction of the body.
Diagnostics
The picture of any type of pulmonary edema is bright. Therefore, diagnosis is simple. For adequate therapy, it is necessary to determine the reasons that caused the swelling. Symptoms depend on the form of edema. The fulminant form is characterized by rapidly increasing suffocation and respiratory arrest. The acute form has more pronounced symptoms, in contrast to the subacute and protracted form.
Symptoms of pulmonary edema
The main symptoms of pulmonary edema include:
- frequent coughing;
- increasing hoarseness;
- cyanosis (the face and mucous membranes become bluish);
- increasing suffocation;
- tightness in the chest, pressing pain;
- increased breathing;
- dizziness, weakness;
- bubbling wheezing is heard;
- with increasing cough - foamy pink sputum;
- as the condition worsens, sputum is released from the nose;
- the person is scared, consciousness may be confused;
- sweating, cold and sticky sweat;
- fear of death;
- increased heart rate up to 200 beats per minute. Can easily develop into life-threatening bradycardia;
- drop or surge in blood pressure.
Pulmonary edema itself is a disease that does not occur on its own. Many pathologies can lead to edema, sometimes completely unrelated to diseases of the bronchopulmonary and other systems.
Classification of the disease
Pulmonary edema, depending on the cause of its occurrence, is divided into two types:
- Hydrostatic, which is characterized by the formation of the disease based on an increase in intravascular hydrostatic pressure. With hydrostatic edema, fluid is removed from the vessel into the alveolus. Hydrostatic pulmonary edema often occurs due to cardiovascular insufficiency.
- Membranous, manifests itself due to the influence of toxins, resulting in destruction of the walls of capillaries and alveoli. This gives impetus to the entry of fluid into the intravascular space.
Pulmonary edema also has two forms of complications, which have corresponding symptoms and signs of the disease. These forms of complications are called:
- Alveolar.
- Interstitial.
Of these two forms, it is worth highlighting the first (alveolar), since it is the most dangerous and leads to dire consequences, in particular, to human death. Interstitial, in turn, is a more gentle form that is subject to treatment and successful recovery. If you do not take appropriate therapeutic measures, then this form worsens and becomes alveolar.
Pulmonary edema has another type of classification: according to the severity of manifestations. There are four degrees, which are characterized by the following signs of manifestations:
- The first degree is called pre-edema and is characterized by the appearance of mild signs of shortness of breath and disturbances in the frequency and rhythm of breathing.
- The second degree is medium, which is characterized by the appearance of wheezing. Shortness of breath increases.
- Third degree - the disease becomes severe and is characterized by increased shortness of breath and wheezing, which can be heard even at a distance.
- Fourth degree - immediate symptoms of the disease occur: weakness, sweating, wheezing, etc. More details about the symptoms in the disease symptoms section.
Causes of pulmonary edema
Causes of pulmonary edema include:
- Sepsis. Usually is the penetration into the bloodstream of exogenous or endogenous toxins;
- Pneumonia;
- Overdose of certain (NSAIDs, cytostatics) drugs;
- Radiation damage to the lungs;
- Drug overdose;
- Myocardial infarction, heart disease, ischemia, hypertension, any heart disease in the decompensation stage;
- Congestion in the right circulation that occurs with bronchial asthma, emphysema and other pulmonary diseases;
- A sharp or chronic decrease in protein in the blood. Hypoalbuminemia occurs with liver cirrhosis, nephrotic syndrome and other kidney pathologies;
- Infusions in large volumes without forced diuresis;
- Poisoning by toxic gases;
- Poisons;
- Gastric aspiration;
- Shock due to serious injuries;
- Enteropathies;
- Being at high altitude;
- Acute hemorrhagic pancreatitis.
Diagnostic measures
To identify the syndrome, two types of diagnostics are carried out: simple and differential.
Simple diagnostic methods:
- Collection of information and study of the clinical picture. If the patient is conscious, and pulmonary edema does not occur in an acute form, then the doctor is obliged to collect an anamnesis, measure the patient’s pulse, his pressure, and use chest percussion to confirm the diagnosis.
- BAC tests. They help identify the primary cause of the disease (for example, a heart attack).
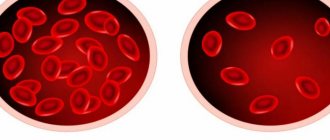
- Analysis of gas concentrations in the bloodstream.
- Chest X-ray. This usually helps confirm or deny the presence of fluid in the lung tissue.
- ECG. Helps identify abnormalities of the heart muscle.
- Pulmonary artery catheterization.
The attending physician can make a final diagnosis only after a detailed study of the patient’s clinical picture, carrying out all types of tests and examinations.
Types of pulmonary edema
There are two types of pulmonary edema: cardiogenic and non-cardiogenic. There is also a 3rd group of pulmonary edema (non-cardiogenic) - toxic edema.
Cardiogenic edema (cardiac edema)
Cardiogenic edema is always caused by acute left ventricular failure and obligatory stagnation of blood in the lungs. Myocardial infarction, heart defects, angina pectoris, arterial hypertension, left ventricular failure are the main causes of cardiogenic edema. To relate pulmonary edema to chronic or acute heart failure, pulmonary capillary pressure is measured. In the case of cardiogenic type of edema, the pressure rises above 30 mmHg. Art. Cardiogenic edema provokes transudation of fluid into the interstitial space, then into the alveoli. Attacks of interstitial edema are observed at night (paroxysmal dyspnea). The patient does not have enough air. Auscultation detects harsh breathing. Breathing is increased during exhalation. Choking is the main symptom of alveolar edema.
The following symptoms are characteristic of cardiogenic edema:
- suffocation;
- increasing cough;
- inspiratory dyspnea. The patient is characterized by a sitting position; in the lying position, shortness of breath increases;
- tissue hyperhydration (swelling);
- dry whistling, turning into wet gurgling wheezing;
- separation of pink frothy sputum;
- acrocyanosis;
- unstable blood pressure. It is difficult to reduce it to normal. A decrease below normal can lead to bradycardia and death;
- tachycardia;
- severe pain behind the sternum or in the chest area;
- fear of death;
- The electrocardiogram shows hypertrophy of the left atrium and ventricle, sometimes blockade of the left bundle branch.
Hemodynamic conditions of cardiogenic edema
- violation of left ventricular systole;
- diastolic dysfunction;
- systolic dysfunction.
The leading cause of cardiogenic edema is left ventricular dysfunction.
Cardiogenic edema must be differentiated from non-cardiogenic edema. With non-cardiogenic edema, changes in the cardiogram are less pronounced. Cardiogenic edema occurs more quickly. There is less time for emergency care than for other types of edema. Death is most often caused by cardiogenic edema.
Toxic pulmonary edema
Toxic edema has certain specific features that contribute to differentiation. There is a period here when there is no swelling itself, there are only reflex reactions of the body to irritation. A burn of lung tissue or a burn of the respiratory tract causes a reflex spasm. This is a combination of symptoms of damage to the respiratory organs and the resorptive effects of toxic substances (poisons). Toxic edema can develop regardless of the dose of the drug that caused it.
Medicines that can cause pulmonary edema:
- narcotic analgesics;
- many cytostatics;
- diuretics;
- X-ray contrast agents;
- non-steroidal anti-inflammatory drugs.
Risk factors for the occurrence of toxic edema are old age and long-term smoking.
It has 2 forms, developed and abortive. There is a so-called “silent” edema. It can be detected by X-ray examination of the lungs. There is practically no definite clinical picture for such edema.
Characterized by periodicity. Has 4 periods:
- Reflex disorders. Characterized by symptoms of irritation of the mucous membranes: lacrimation, cough, shortness of breath. The period is dangerous due to respiratory and cardiac arrest;
- Hidden period of subsidence of irritation. May last 4-24 hours. Characterized by clinical well-being. A thorough examination may show signs of impending edema: bradycardia, pulmonary emphysema;
- Direct pulmonary edema. The course is sometimes slow, reaching 24 hours. Most often, symptoms increase within 4-6 hours. During this period, the temperature rises, the blood count shows neutrophilic leukocytosis, and there is a danger of collapse. The developed form of toxic edema has a fourth period of completed edema. The completed period has “blue hypoxemia”. Cyanosis of the skin and mucous membranes. The completed period increases the breathing rate to 50-60 times per minute. Bubbling breathing can be heard from a distance, sputum mixed with blood. Blood clotting increases. Gas acidosis develops. “Gray” hypoxemia is characterized by a more severe course. Vascular complications are added. The skin takes on a pale grayish tint. The limbs are cold. Thread-like pulse and drop in blood pressure to critical values. This condition is promoted by physical activity or improper transportation of the patient;
- Complications. When leaving the period of immediate pulmonary edema, there is a risk of developing secondary edema. This is due to left ventricular failure. Pneumonia, pneumosclerosis, emphysema are common complications caused by drugs and toxic edema. At the end of the 3rd week, “secondary” edema may occur due to acute heart failure. Rarely does an exacerbation of latent tuberculosis and other chronic diseases occur. Depression, drowsiness, asthenia.
With quick and effective therapy, a period of reverse development of edema begins. It does not belong to the main periods of toxic edema. Here everything depends only on the quality of the assistance provided. Cough and shortness of breath decrease, cyanosis decreases, wheezing in the lungs disappears. The X-ray shows the disappearance of large, then small lesions. The peripheral blood picture is normalizing. The recovery period from toxic edema can be several weeks.
In rare cases, toxic edema can be caused by taking tocolytics. The catalyst for edema can be: large volumes of intravenously administered fluid, recent treatment with glucocorticoids, multiple pregnancy, anemia, unstable hemodynamics in a woman.
Clinical manifestations of the disease:
- The key symptom is respiratory failure;
- Severe shortness of breath;
- Cough;
- Severe chest pain;
- Cyanosis of the skin and mucous membranes;
- Arterial hypotension in combination with tachycardia.
Toxic edema differs from cardiogenic edema by its protracted course and the content of a small amount of protein in the fluid. The size of the heart does not change (it rarely changes). Venous pressure is often within normal limits.
Diagnosis of toxic edema is not difficult. An exception is bronchorrhea due to FOS poisoning.
Non-cardiogenic pulmonary edema
Occurs due to increased vascular permeability and high filtration of fluid through the wall of the pulmonary capillaries. With a large amount of fluid, the functioning of blood vessels worsens. Liquid begins to fill the alveoli and gas exchange is disrupted.
Causes of non-cardiogenic edema:
- renal artery stenosis;
- pheochromocytoma;
- massive renal failure, hyperalbuminemia;
- exudative enteropathy;
- pneumothorax can cause unilateral non-cardiogenic pulmonary edema;
- severe attack of bronchial asthma;
- inflammatory lung diseases;
- pneumosclerosis;
- sepsis;
- aspiration of gastric contents;
- cancerous lymphangitis;
- shock, especially with sepsis, aspiration and pancreatic necrosis;
- cirrhosis of the liver;
- radiation;
- inhalation of toxic substances;
- lungs' cancer;
- large transfusions of drug solutions;
- in elderly patients taking acetylsalicylic acid for a long time;
- drug addict.
To clearly differentiate edema, the following measures should be taken:
- study the patient's history;
- apply methods of direct measurement of central hemodynamics;
- radiography;
- assess the affected area during myocardial ischemia (enzyme tests, ECG).
To differentiate non-cardiogenic edema, the main indicator will be the measurement of wedge pressure. Normal cardiac output and positive wedge pressure results indicate a non-cardiogenic nature of the edema.
Stages of pathology development
The main stages of the development of the disease:
- The pressure in the capillaries will increase. During this process, the permeability of the capillary walls involved in the pulmonary circulation begins to sharply decrease, causing tissue to be excreted into the pulmonary interstitial tissue. Over time, the pulmonary alveoli will absorb a large amount of foreign fluid and lose the ability to participate in gas exchange. This is the reason why, when pulmonary edema occurs, elderly patients experience attacks of suffocation and their skin turns blue.
- Gradually, oncotic blood pressure will decrease.
- The alveolo-capillary membrane will lose its integrity.
Any suspicious symptoms indicating an exacerbation of the pathology should be accompanied by a visit to a doctor. At the first sign you need to call an ambulance.
Consequences of pulmonary edema
When the swelling is stopped, it is too early to end the treatment. After an extremely severe condition of pulmonary edema, serious complications often arise:
- addition of a secondary infection. Pneumonia most often develops. Against the background of reduced immunity, even bronchitis can lead to adverse complications. Pneumonia associated with pulmonary edema is difficult to treat;
- hypoxia, characteristic of pulmonary edema, affects vital organs. The most serious consequences can affect the brain and cardiovascular system - the effects of swelling may be irreversible. Cerebral circulation disorders, cardiosclerosis, heart failure without powerful pharmacological support lead to death;
- ischemic damage to many organs and systems of the body;
- pneumofibrosis, segmental atelectasis.
Emergency care for pulmonary edema
Required for every patient with signs of pulmonary edema. Emergency care highlights:
- the patient must be placed in a semi-sitting position;
- aspiration (removal) of foam from the upper respiratory tract. Aspiration is performed by inhaling oxygen through 33% ethanol;
- urgent oxygen inhalation (oxygen therapy);
- elimination of acute pain syndrome with the help of antipsychotics;
- restoration of heart rhythm;
- correction of electrolyte balance;
- normalization of acid-base balance;
- normalization of hydrostatic pressure in the pulmonary circulation. Narcotic analgesics “Omnopon” and “Promedol” are used. They depress the respiratory center, relieve tachycardia, reduce venous blood flow, lower blood pressure, reduce anxiety and fear of death;
- vasodilators (Nitromint aerosol). The drugs reduce vascular tone and intrathoracic blood volume. Nitroglycerin preparations facilitate the outflow of blood from the lungs, acting on peripheral vascular resistance;
- application of venous tourniquets to the lower extremities. The procedure is necessary to reduce CTC - an old effective method. Currently, 40 mg of Lasix intravenously is used to dehydrate the lung parenchyma. The action of furosemide (Lasix) develops within a few minutes and lasts up to 3 hours. The drug is capable of removing 2 liters of urine in a short period of time. A reduced plasma volume with increased colloid osmotic pressure contributes to the transition of edematous fluid into the bloodstream. Filtration pressure decreases. For low blood pressure, diuretics can be used only after it has normalized;
- prescription of diuretics for lung dehydration (Lasix 80 mg intravenously);
- administration of cardiac glycosides to increase myocardial contractility;
- immediate hospitalization.
Prevention
For bedridden patients, daily breathing exercises are recommended to prevent congestion in the lung tissue and further swelling. It also helps to increase the depth of breathing, oxygenate the blood with oxygen and reduce the likelihood of developing pneumonia. To avoid pulmonary edema in bedridden patients, you should monitor the person’s condition, pay attention to any changes in well-being and do not delay contacting a specialist. If relatives take responsibility for caring for a person, they should know the signs of pulmonary edema in bedridden patients, as well as other complications, in order to provide emergency assistance on time.
Periodic changes in body position have a positive effect not only on the condition of a person’s skin, but also prevent fluids from accumulating in the tissues, causing swelling. Fluid balance must be in an adequate rhythm. If a person has a decreased amount of daily urine, this is the first indicator of poor kidney function, which can subsequently lead to pulmonary edema.
Main complications after emergency care
Such complications include:
- development of a fulminant form of edema;
- intensive foam production can cause airway obstruction;
- depression (depression) of breathing;
- tachyarrhythmia, asystole;
- angiotic pain. Such pain is characterized by an unbearable pain syndrome; the patient may experience pain shock, worsening the prognosis;
- impossibility of stabilizing blood pressure. Pulmonary edema often occurs against a background of low and high blood pressure, which can alternate within a large amplitude. The vessels will not be able to withstand such a load for long and the patient’s condition worsens;
- increase in pulmonary edema against the background of high blood pressure.
Symptoms
As we have already noted, the difference between acute and chronic edema depends on the rate of accumulation of liquid mass.
Symptomatic expressions also vary.
Acute edema:
- Air deficiency;
- Difficulty breathing when inhaling;
- Anxiety;
- Moist cough;
- Pain syndrome;
- Tachycardia or arrhythmia.
Edema is chronic. Here we explain that its symptoms are very similar to the symptoms of pleurisy:
- Increased fatigue;
- Shortness of breath that increases;
- Headache;
- Productive cough;
- Manifestation of attacks of fever;
- Sweating at night;
- Waking up from suffocation.
Treatment of pulmonary edema
It comes down to one thing - the swelling should be removed as soon as possible. Then, after intensive treatment of the pulmonary edema itself, medications are prescribed to treat the disease that caused the edema.
So, means for relieving swelling and subsequent therapy:
- Morphine hydrochloride. A vital drug for the treatment of cardiogenic type and other edema in case of hyperventilation. The administration of morphine hydrochloride requires readiness to transfer the patient to controlled breathing;
- Nitrate preparations in infusion form (glycerol trinitrate, isosorbitol dinitrate) are used for any edema, excluding edema with hypovolemia due to pulmonary embolism;
- The introduction of loop diuretics (“Furosemide”, “Torasemide”) in the first minutes of edema saves the lives of many patients;
- In the case of cardiogenic pulmonary edema as a result of myocardial infarction, administration of tissue plasminogen activator is mandatory;
- With atrial fibrillation. Only if the effectiveness of electropulse therapy is low. Often, against the background of even a slight decrease in rhythm, the patient’s condition can significantly worsen. When amiodarone is prescribed, dobutamine infusion is sometimes required to increase the rate;
- Corticosteroids are used only for non-cardiogenic edema. The most commonly used is dexamethasone. It is actively absorbed into the systemic bloodstream and negatively affects the immune system. Modern medicine now recommends the use of methylprednisolone. Its elimination period is much shorter, side effects are less pronounced, and its activity is higher than that of dexamethasone;
- For inotropic rhythm support in case of overdose of beta-blockers, dopamine is used;
- Cardiac glycosides (digoxin) are necessary for constant atrial fibrillation, sodium thiopental is necessary for short-term anesthesia, to relieve pain;
- "Diazepam" with ketamine is used for premedication;
- For heroin-induced pulmonary edema or iatrogenic complications, muscle relaxants (naloxone) are prescribed;
- In conditions of high-altitude pulmonary edema, Nifedipine is needed; it quickly lowers blood pressure;
- At the inpatient stage of treatment, loading doses of antibiotics are prescribed to prevent infection. In first place are drugs from the group of fluoroquinolones: Tavanik, Tsifran, levofloxacin;
- To facilitate the removal of accumulated fluid, large doses of ambroxol are prescribed;
- Prescribing a surfactant is mandatory. It reduces tension in the alveolus and has a protective effect. Surfactant improves oxygen absorption by the lungs, reduces hypoxia;
- Sedatives for pulmonary edema. In the treatment of patients who have suffered pulmonary edema, the leading role is played by the normalization of the emotional background. Often, severe stress itself can trigger swelling. The stress trigger often causes pancreatic necrosis and myocardial infarction. Sedatives can, in combination with other drugs, normalize the content of catecholamines. Due to this, spasm of peripheral vessels is reduced, blood flow is significantly reduced, and the load on the heart is removed. Normal heart function improves the outflow of blood from the pulmonary circle. The calming effect of sedatives can relieve vegetative-vascular manifestations of edema. With the help of sedatives, it is possible to reduce the filtration of tissue fluid through the alveolar-capillary membrane. Means that can influence the emotional background can reduce blood pressure, tachycardia, reduce shortness of breath, vegetative-vascular manifestations, and reduce the intensity of metabolic processes - this facilitates the course of hypoxia. Not counting the morphine solution - the first, most effective aid for pulmonary edema, 4 ml of a solution of droperidol 0.25% or Relanium 0.5% - 2 ml is prescribed. Unlike morphine, these drugs are used for all types of pulmonary edema;
- Ganglion blockers: Arfonad, pentamin, benzohexonium. They allow you to quickly relieve pulmonary edema with high blood pressure (from 180 mm Hg). Improvement comes quickly. 20 minutes after the first administration of the drugs, shortness of breath and wheezing decrease, and breathing becomes calmer. With the help of these drugs, pulmonary edema can be stopped completely.