Issues discussed in the material:
- What is the reason for the development of congestive pneumonia in older people?
- What are the features of the course and diagnosis of congestive pneumonia in older people?
- What is the treatment for congestive pneumonia in the elderly?
- What measures prevent the development of congestive pneumonia in older people
Hypostatic (congestive) pneumonia in older people proceeds completely differently than in young people. The main reasons are the age of the patient and the weakness of the immune system. It is important to diagnose and properly treat this disease in time to avoid negative consequences. But it is quite difficult to identify congestive pneumonia in older people, therefore, even minor deterioration in health cannot be ignored.
Causes of congestive pneumonia in older people
Older people are more likely to be exposed to factors that worsen their health and suffer from chronic diseases. And, as a rule, such patients are conscious about their well-being, try to constantly visit doctors and treat their ailments.
But congestive complications appear unexpectedly, so it is impossible to diagnose their development in advance. He who is forewarned is forearmed. Therefore, knowing the nature of the origin of hypostatic pneumonia in older people, you can prevent its occurrence.
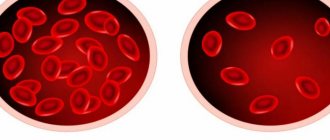
Over the years, age-related changes are inevitable; they affect all life support systems. In the respiratory system, this is expressed in weakening of the diaphragm muscles, uneven breathing, and a decrease in the elasticity of lung tissue.
However, it is not only advanced years that affect the risk of inflammatory processes. There are a number of other interdependent factors. If several negative causes are simultaneously observed, then it will not be easy to cure pneumonia, and the course of the disease itself will be severe. Consider these factors:
- Recumbent state. An acute form of pneumonia, namely hypostatic, occurs in patients who have suffered a serious illness (heart attack, stroke) or surgery, that is, they are forced to remain motionless for a long time. In such a situation, microbes spread faster, and even a harmless acute respiratory infection becomes a source of inflammation.
- Treatment of other diseases with a large number of drugs, which reduces the body's ability to resist infections.
- Diseases of the heart, blood vessels, genitourinary system, diabetes mellitus, malignant tumors.
- Chronic forms of diseases of the respiratory system.
If an elderly patient has at least two factors, then there is a high risk of congestive pneumonia.
We recommend
“Swelling in the elderly: causes, treatment, medications” Read more
Consequences of congestive pneumonia in the elderly
Early diagnosis of inflammation and proper therapy reduce the likelihood of serious problems, such as the development of purulent processes. Poor health depends not only on the number of years lived and the duration of development of complications, but also on concomitant diseases. For example, if a patient has diabetes or suffers from alcohol addiction, then the likelihood of negative events occurring increases.
Complications of hypostatic pneumonia can cause breathing problems, which will also affect the cardiovascular system. With an unfavorable course and untimely treatment, negative consequences are possible - the death of the patient.
Congestive pneumonia causes inflammation of the outer lining of the heart (pericarditis) or accumulation of fluid in the pleural cavity (exudative pleurisy). The disease can damage both the lower parts of the right lung and both organs.
In most cases, the phenomenon of congestive pneumonia is observed precisely in patients forced to lead a recumbent lifestyle.
We recommend
“Senile dementia: causes, symptoms, patient care” Read more
Treatment
It is fundamentally important to determine the patient’s management tactics - whether he should be hospitalized or whether treatment can be carried out on an outpatient basis. For these purposes, you can use the CURB-65/CRB-65 scale, which involves assessing a number of indicators (presence - 1 point, absence - 0):
C —impaired consciousness
U - blood urea nitrogen more than 7 mmol/l (not taken into account in CRB-65)
R — respiratory rate ≥ 30 per minute.
B - systolic blood pressure < 90 mm Hg or diastolic blood pressure < 60 mm Hg. Art.
65 - age 65 years and older
Explanation:
0 points - the patient belongs to group I (mortality 1.2%) and is treated on an outpatient basis.
1–2 points correspond to group II (mortality 8.15%), patients in this group are subject to hospitalization with observation and dynamic assessment of the condition.
3 points and above - patients are subject to emergency hospitalization; mortality in this group can reach 31%.
Diagnosis of congestive pneumonia in the elderly
Determining the presence of congestive inflammation in older patients is quite difficult. It happens that doctors do not take into account the manifestations of the disease, but often, playing it safe, they make an unjustified verdict.
To accurately detect pulmonary inflammation you should:
- Undergo an X-ray examination. If there is an inflammatory process, then the image will show an accumulation of fluid.
- Do an ultrasound examination of the space around the lungs. Ultrasound allows you to identify fluid stagnation and where it accumulates in the lungs.
- Listen to the chest with a phonendoscope or stethoscope. Signs of inflammation will be indicated by hoarseness when inhaling and exhaling, as well as gurgling sounds.
Based on the studies performed, the doctor may prescribe additional ones, for example, a blood test, bacterial cultures, etc.
We recommend
“Why blood pressure drops in older people: causes and treatment” Read more
2. Symptoms of the disease
The most common symptoms of pulmonary embolism are:
- Sudden shortness of breath;
- Chest pain that gets worse with coughing and deep breathing;
- Cough with pink and foamy mucus.
Pulmonary embolism can also cause more general and non-specific symptoms. For example, you may feel anxious, dizzy, have a fast heartbeat, sweat heavily, or lose consciousness.
The appearance of such symptoms is a reason to immediately seek emergency medical help, especially if these signs of embolism appear suddenly and are severe. Causes of pulmonary embolism.
In most cases, a pulmonary embolism is caused by a blood clot in the leg that breaks off and travels to the lungs through the bloodstream. A blood clot in a vein close to the skin cannot cause a pulmonary embolism. But a blood clot in the deep veins (this disease is called deep vein thrombosis) poses a considerable danger.
Blocked arteries can also occur due to other things, such as tumors, air bubbles, amniotic fluid or fat that enters the blood vessels when a bone is broken. But this happens very rarely.
Visit our Pulmonology page
How is congestive pneumonia treated in the elderly?
A mild form of inflammation can be quickly cured with drug therapy. Hypostatic pneumonia is characterized by the accumulation of fluid in the lungs and bronchi, and is therefore treated with other drugs.
Treatment includes the simultaneous administration of bacteriostatic drugs (macrolides) and antibiotics from the class of aminopenicillins or cephalosporins. These medications are prescribed immediately upon detection of the disease, regardless of the results of the bacterial test, since the test readiness period is at least five days. When the exact class of microorganisms is identified, antibacterial therapy is changed if it did not work at the initial stage.
Treatment of congestive pneumonia in older people takes place strictly in a medical institution under the supervision of specialists.
Together with therapy aimed at eliminating the localization of inflammation, treatment is prescribed for the proper functioning of the respiratory system. For this they prescribe:
- drugs that reduce the accumulation of fluid in the lung tissues (diuretics);
- immunomodulatory drugs and antioxidants;
- medicines that facilitate the discharge of sputum.
For the cardiovascular system, glycosides and medications aimed at restoring metabolism are prescribed. Sputum can accumulate not only in the lungs, but also in the bronchi and trachea. To determine it, a special study is performed - bronchoscopy. Based on the examination results, if fluid is present, diuretics are prescribed and punctures are taken.
Along with drug therapy, physical procedures are used: inhalations, massages, oxygen masks, breathing exercises (using the methods of Buteyko and Strelnikova). Elderly patients are also advised to practice deep breathing, which is performed using the diaphragm.
When acute signs of inflammation are relieved and patients feel well, they are allowed to go home, where they are advised to continue treatment with prescribed medications and traditional methods. These include drinking plenty of water: berry teas and decoctions of medicinal herbs (thyme, rose hips).
It happens that a congestive inflammatory process is very difficult: the patient constantly lies down, it is difficult for him to breathe. In such cases, doctors prescribe a puncture of the chest to remove large amounts of sputum.
We recommend
“Vitamins for elderly people over 70: which ones are needed first” Read more
Management of patients with CAP in a hospital setting
It is advisable to begin therapy for pneumonia in hospitalized patients with parenteral antibiotics. After 3–4 days, provided the temperature normalizes, intoxication and other symptoms decrease, it is possible to switch to oral forms of antibiotics until the course of treatment is completed (step-down therapy). Antibacterial drugs can be used both as part of combination therapy and as monotherapy. More detailed treatment regimens for CAP are presented in Table No. 2.
Table 2.
Treatment regimens for CAP depending on the course
| Group | Most common pathogens | Recommended treatment regimens | |
| Drugs of choice | Alternative drugs | ||
| EP of non-severe course | S. pneumoniae H. influenzae C. pneumoniae S. aureus Enterobacteriaceae | Benzylpenicillin IV, IM ± macrolide (clarithromycin, azithromycin) orally, or Ampicillin IV, IM ± macrolide orally, or Amoxicillin + clavulanic acid IV ± macrolide orally, or Cefuroxime IV, IV m ± macrolide orally, or Cefotaxime IV, IM ± macrolide orally, or Ceftriaxone IV, IM ± macrolide orally | Respiratory fluoroquinolones (levofloxacin, moxifloxacin) IV Azithromycin IV |
| Severe EP | S. pneumoniae Legionella spp. S. aureus Enterobacteriaceae | Amoxicillin + clavulanic acid IV + macrolide IV, or Cefotaxime IV + macrolide IV, or Ceftriaxone IV + macrolide IV | Respiratory fluoroquinolones (levofloxacin, moxifloxacin) IV + III generation cephalosporins IV |
Note:
- If the presence of “atypical” pneumonia is suspected, the use of macrolides is indicated.
- If there is a risk of infection with P. aeruginosa (bronchiectasis, use of corticosteroids, therapy with broad-spectrum antibiotics for more than 7 days during the last month, exhaustion), the drugs of choice are ceftazidime, cefepime, cefoperazone + sulbactam, meropenem, imipenem, piperacillin/tazobactam, ciprofloxacin, in monotherapy or in combination with aminoglycosides of the II–III generation.
- If aspiration is suspected, the following treatment options are indicated: cefoperazone + sulbactam, ticarcillin + clavulanic acid, carbapenems, piperacillin/tazobactam.
An initial assessment of the effectiveness of antibacterial therapy should be carried out 24–48 hours after the start of treatment. If signs of pneumonia persist in adults or children, treatment tactics should be reconsidered.
For mild CAP, the course of antibiotic therapy is about 7–10 days. For severe CAP of unspecified etiology, a 10-day course of antibiotic therapy is recommended. If there is evidence of mycoplasma or chlamydial etiology, therapy should last 14 days; in the case of CAP caused by staphylococci, gram-negative enterobacteria, legionella, the duration of therapy is 14–21 days.
In addition to antibiotics, the following are used in the treatment of CAP:
- Antiviral therapy: neuraminidase inhibitors (oseltamivir, zanamivir), active against influenza A and B viruses. Duration of use is 5–10 days.
- Mucolytics and expectorants - tablet or inhalation forms.
- Glucocorticosteroids: used for developed septic shock (hydrocortisone 200–300 mg/day for no more than 7 days).
- Oxygen therapy for PaO2 < 55 mm Hg. Art. or SpO2 < 88% (breathing air). It is optimal to maintain SpO2 within 88–95% or PaO2 within 55–80 mm Hg. Art.
- Infusion therapy - to correct hypovolemia.
- Low molecular weight heparins for the prevention of thromboembolism in severe patients.
- Physiotherapy and exercise therapy to reduce inflammation and improve sputum discharge.
Prevention of the development of congestive pneumonia in older people
Hypostatic inflammation in older people develops against the background of other diseases, therefore, to prevent the occurrence of pneumonia, certain preventive measures should be followed:
- Maintain a comfortable temperature in the room: do not overheat and do not overcool.
- Be outdoors often, regardless of the weather. You just need to dress according to the weather conditions.
- Rest more and don't worry.
- Get rid of bad habits: alcohol, smoking.
- Take the right foods that contain essential minerals and vitamins. First of all, this applies to red fish, meat and legumes - these products are rich in zinc.
- During periods of exacerbation of seasonal epidemics, it is necessary to get vaccinated on time.
- For bedridden patients, the following preventive methods are indicated: - do percussion massage for better sputum discharge, avoiding the area near the heart;
- use jars and mustard plasters;- do not lie in bed in one state, constantly change your body position;
- do some physical and breathing exercises. For example, move your arms and legs, inflate balloons;
— keep the room clean (wet cleaning, ventilation).
Congestive complications of pneumonia in older people can be successfully treated without serious health consequences. The main thing in this matter is timely diagnosis and competent therapy.