Rheumatic carditis is the most common manifestation of rheumatism. This term refers to autoimmune inflammation in the walls of the chambers of the heart, which occurs in response to an infection caused by a special type of bacteria - group A β-hemolytic streptococcus. The substances that this microorganism produces are similar in structure to those that make up human connective tissue. The immune system becomes confused and begins to attack not only the harmful single-celled invaders, but also the body’s own tissues.
Our expert in this field:
Serebryansky Yuri Evstafievich
Cardiologist, geriatrician, therapist, professor, Honored Doctor of the Russian Federation, Doctor of Medical Sciences
Call the doctor Reviews about the doctor
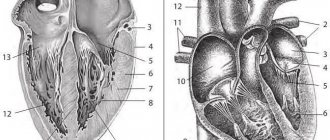
In order to understand what rheumatic carditis is, you first need to understand how the heart wall is structured. It consists of three layers:
- Endocardium is the inner lining. It lines the inside of all the chambers of the heart and covers the valve leaflets.
- Myocardium is the muscle through which the heart contracts and pushes blood through the vessels.
- The epicardium is a thin film of connective tissue that covers the outside of the heart. It protects the organ and produces lubrication, which reduces friction during heart contractions. The endocardium is part of the heart sac - the pericardium.
If rheumatism leads to inflammation in the endocardium and myocardium, this condition is called rheumatic carditis. If the pathological process has spread to the pericardium (which rarely happens), they speak of the addition of pericarditis.
Nature of the disease
Rheumatic carditis is a complication of sore throat, pneumonia, erysipelas, scarlet fever and other infectious diseases caused by group A beta-hemolytic streptococcus. The waste products of this bacterium are similar in structure to the components of connective tissue.
The disease is autoimmune in nature. At some point, the immune system fails and it begins to attack not only the foreign microorganism, but also its own cells. The joints and tissues of the heart are affected.
Prevention Tips
- Prevention of streptococcal infections - administration of the antibiotic Bicillin-5. Bicillin prophylaxis is for those who have already suffered from rheumatism (in this case, prophylaxis is year-round), as well as those who have been in contact with patients. The doctor will select the right dose or replace the drug if you are allergic to penicillin antibiotics.
- Strengthening the immune system - there are no “magic” pills for him, but a clear daily routine, good nutrition, and regular physical activity will help him a lot.
You can go jogging, swimming, or your favorite sport. Up to 20 years of age, strength training and activities that develop flexibility and joint performance (dancing, fitness) are suitable. After 35-40 years, you need to take care of the health of your spine and choose yoga and Pilates. Moderate cardio exercise (walking, running, skating) is also suitable.
- Timely and competent treatment of upper respiratory tract diseases: when the first symptoms appear, you need to consult a doctor (pediatrician, therapist), do not refuse antibiotics if they are prescribed by a specialist, and also do not interrupt the course of treatment at the first improvement. Isolation of patients with streptococcal infection is also necessary: keeping the patient in a separate ventilated room. He must have his own hygiene items and utensils. The patient needs to buy a set of non-woven masks and change them every 3 hours.
After an infection, you need to undergo a comprehensive diagnosis: urine and blood tests, and an ultrasound of the heart. Children need to be observed for 3 months by a pediatrician and rheumatologist.
Clinical picture
The disease manifests itself two to three weeks after a person has had a staphylococcal infection (but this period can increase to one to two months). The joints are the first to be affected (rheumatism itself), and wandering pain appears. There is general malaise, loss of strength, and fever. Further symptoms of pathology from the cardiovascular system are added:
- tachycardia;
- heart rhythm disturbance;
- pain and feeling of heaviness in the heart;
- shortness of breath with minor exertion;
- swelling;
- acrocyanosis – fingers, lips, tip of the nose become bluish and constantly cold;
- moist cough.
In adults, rheumatic carditis occurs asymptomatically or with minor discomfort. In childhood and adolescence, pain in the heart can be very disturbing, especially during physical activity.
How to establish the correct diagnosis?
Usually, a person with heart pain first sees a therapist. It is very important that the doctor conduct a thorough examination and comprehensive examination - this will help to suspect rheumatic carditis and promptly refer the patient to a rheumatologist.
Rheumatism can also affect other organs: joints, skin, nervous system, lungs. But inflammation in them, unlike the heart, does not lead to permanent changes. Usually the symptoms go away without a trace.
To diagnose the disease, they resort to special blood tests, echocardiography (ultrasound of the heart), ECG, chest and joint x-rays.
Why is rheumatic heart disease dangerous?
Previous rheumatic carditis causes heart defects, in particular mitral valve stenosis. In case of a one-time illness, the probability of developing valve disease is 20 percent.
Rheumatic attacks threaten the formation of scars. All this leads to heart failure and heart rhythm disturbances.
In children and adolescents, the inflammatory process can develop into a severe form of heart damage - diffuse myocarditis. Allergic inflammation develops, which leads to an increase in organ volume and serious heart failure. Young patients experience difficulty breathing, weakness, even fainting, swelling of the veins in the neck, and hypotension.
Rheumatism
Angina
Scarlet fever
Arthritis
24869 05 May
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Rheumatism: causes, symptoms, diagnosis and treatment methods.
Definition
From the point of view of modern medicine, rheumatism (rheumatic fever) is a systemic inflammatory process of an infectious-allergic nature that affects the connective tissue of the body. First, inflammation occurs, to which the body responds with an immune response, and then an autoimmune attack begins on the connective tissue of the body’s own. Rheumatism is often associated with joint pain and rheumatoid arthritis, but this is only part of the symptoms of the disease. Rheumatic fever affects the heart muscle tissue, skin, blood vessels, brain and nervous system. Rheumatic lesions of the respiratory system, vision, and gastrointestinal tract are much less common.
The intensity of joint pain is so great that it drowns out most of the symptoms, so a person does not immediately feel other disorders of the body.
It is rheumatic diseases that make the greatest contribution to decreased performance, deterioration of the patient’s general health, and an increase in the number of visits to primary care doctors. Rheumatic diseases occur in people of any age. The first episode of acute rheumatic fever most often develops between 5 and 15 years; it practically does not occur in children under three years of age. The disease affects girls three times more often than boys.
Causes of rheumatism
The main cause of rheumatism is a respiratory streptococcal infection of group A. As a rule, the disease is preceded by tonsillitis, tonsillitis, pharyngitis, scarlet fever, etc., during which the immune system actively produces specific antibodies to fight streptococci. Antibodies detect infectious agents by certain protein molecules, but in some people the same proteins are present in the connective tissue of the heart and blood vessels. As a result, anti-streptococcal antibodies attack their own tissues, causing an inflammatory process in them.
In some cases, we can talk about a genetic predisposition, since the incidence of the disease in children is much higher in those families where one of the parents is diagnosed with rheumatism.
The pathological process is autoimmune in nature, so the disease occurs in waves, exacerbating under the influence of infection or nonspecific factors (hypothermia, physical stress, emotional stress, etc.).
The following factors contribute to the development of rheumatic fever:
- incorrect treatment of streptococcal infection;
- genetic predisposition;
- hypothermia;
- deficiency of vitamins and microelements;
- the presence of autoimmune diseases (systemic lupus erythematosus, scleroderma, etc.).
Classification of the disease According to the nature of the course,
the following are distinguished:
- acute form (up to 3 months);
- subacute form (3-6 months);
- protracted form (more than 6 months);
- latent (hidden) form - occurs without characteristic symptoms, without laboratory changes, is detected after the formation of heart defects;
- recurrent form - has a wave-like course with the rapid development of internal organ failure.
In addition, there are active and inactive phases of the disease.
In the active phase, a specific laboratory picture is observed. According to clinical manifestations:
- rheumatic carditis - inflammation of the heart tissue;
- polyarthritis ー multiple joint damage;
- ring-shaped erythema - a specific rash on the skin;
- chorea - severe neurological symptoms (hand tremors, muscle weakness, involuntary movements);
- subcutaneous nodules in the joint area.
Symptoms of rheumatism
The initial symptoms of rheumatism usually occur 2-3 weeks after a streptococcal infection and are a combination of damage to the joints, heart, skin and central nervous system. Symptoms depend on the nature of the process and which organs are affected by inflammation. A typical clinical picture appears in the second or third week after suffering a streptococcal infection - the patient develops a fever, develops weakness, and experiences increased sweating and headache.
At an early stage, arthralgia is noted - rapidly increasing pain in large joints (knees, elbows, shoulders, ankles, wrists) with limited mobility.
With rheumatism, the joints, as a rule, are not deformed, but they can swell and increase in size.
Changes in the musculoskeletal system manifest themselves in the form of rheumatic arthritis. Migratory polyarthritis is the most common manifestation of acute rheumatic fever, often accompanied by fever. “Migratory” means that the arthritis appears in one or more joints, resolves, but then occurs in others, causing the pain to seem to move from one joint to another. A feature of rheumatic arthritis is its rapid reversal when antirheumatic drugs are prescribed. Sometimes joint damage manifests itself only as polyarthralgia - pain in the joints without the development of arthritis.
Cardiac dysfunction is characterized by murmurs, arrhythmias, tachycardia and decreased blood pressure, leading to heart failure. Patients complain of mild pain or discomfort in the heart area, mild shortness of breath on exertion. As a rule, heart tissue is affected from the inside to the outside, i.e. valves and endocardium, then myocardium and finally pericardium. Rheumatic disease is formed as a result of the course of chronic rheumatic heart disease over decades and is primarily manifested by valve stenosis. The most commonly involved valves are the mitral and aortic valves.
Rheumatic carditis in some young patients and children can be severe - from the very beginning of the disease there is severe shortness of breath on exertion and at rest, constant pain in the heart area, and rapid heartbeat. Symptoms of circulatory failure in the systemic circle may appear in the form of swelling and heaviness in the right hypochondrium (due to an enlarged liver). All these symptoms indicate severe diffuse myocarditis.
Loss of coordination, muscle weakness, and uncontrolled movements may be signs of rheumatic damage to the nervous system. The disease can affect the psyche and the functioning of the speech apparatus.
Lesions of the nervous system and sensory organs are extremely rare, mainly in children.
Skin pathologies associated with rheumatism are expressed by redness and irritation in the form of round spots. Subcutaneous nodules may appear on the arms and legs, but they are not painful and may disappear without treatment.
Features of rheumatism in children:
In children, rheumatic fever is more severe than in adults, and heart defects develop more often and faster. The articular syndrome is mild, and other extracardiac manifestations (ring-shaped erythema, subcutaneous nodules, chorea) are more common with more pronounced manifestations.
However, in children, the disease responds better to drug treatment, which helps avoid relapses.
Diagnosis of rheumatism
Rheumatism is diagnosed based on clinical and laboratory parameters. Main criteria: polyarthritis, carditis, chorea, annular rash, subcutaneous nodules.
Diagnostic measures include:
- general blood analysis;
Treatment of rheumatic carditis and prevention
The only preventive measure is timely treatment of infections. It is necessary to see a doctor and take prescribed antibiotics on time. If after an illness you notice problems with your heart and other symptoms described above, be sure to visit a therapist or cardiologist.
Predisposition to rheumatic carditis is hereditary. If your relatives have this problem, it is necessary to be examined. The disease is diagnosed based on the results of two examinations: electrocardiography and biochemical blood tests.
Additionally, echocardiography, x-rays and other studies may be prescribed. After an accurate diagnosis is established, treatment is prescribed. This is usually drug therapy:
- Antibiotics, such as vancomycin and doxycycline, are aimed at killing streptococcus;
- Immunoregulators are drugs that stop autoimmune processes. Prescribed to patients in difficult cases. These include prednisolone, dexamethasone and other drugs that inhibit immune system cells.
- Non-steroidal anti-inflammatory drugs (aspirin and ibuprofen). They will be quite sufficient if the disease proceeds without complications.
- Diuretics - prescribed to eliminate edema.
- Cardiac glycosides are necessary to support heart function.
- General strengthening drugs and vitamins.
During the treatment period, constant monitoring by a cardiologist is necessary; some patients require hospitalization.
At the first symptoms of rheumatic carditis, seek advice from medical specialists. Here you will undergo the necessary research in a comfortable environment using modern equipment. The appointments are conducted by doctors with extensive experience. Early treatment will help avoid further problems.
Diagnostic measures
The basis for diagnosing rheumatic carditis is observation of the clinical picture. The doctor should carefully collect anamnesis, especially provoking factors such as infectious diseases should be identified. Physical examination is important. Detection of pathological murmurs in the heart may indicate the presence of valvular defects.
Standard laboratory and instrumental studies will help to suspect the disease:
- blood test (leukocytosis, shift of the formula to the left, increased ESR, appearance of C-reactive protein);
- ECG (arrhythmias, myocardial hypertrophy, diffuse cardiomyopathy);
- X-ray of the OGK (allows you to detect an enlarged heart);
- echocardiography (the best method for identifying defects);
The following laboratory tests can confirm the rheumatic nature of heart damage:
- determination of antistrepococcal antibodies;
- determination of autoantibody titer;
- protein spectrum;
- diphenylamine test.
What is rheumatic heart disease
Rheumatic fever is one example of such an inappropriate response and usually occurs several weeks after a certain type of bacterial throat infection. Inflammation is widespread and affects many body systems, including the heart. This is an acute reaction that can last several weeks and usually does not cause permanent damage to any part of the body, except in some cases to the heart valves.
Rheumatic heart disease is an inflammation of the heart that occurs as a result of a post-infectious immunologically mediated reaction known as rheumatic fever . Acute rheumatic fever affects various organs and systems of the body, including the heart, skin, joints and nerves. Although the heart is not the only organ affected by rheumatic fever, the chronic effects, usually affecting its valves, can seriously impair normal cardiac function in the long term.
Carditis in acute rheumatic fever
In rheumatic fever, all three layers of the heart can be inflamed to varying degrees, and this is called pancarditis. This includes the inner endocardium (endocarditis), the middle muscular myocardium (myocarditis), and the outer lining of the pericardium (pericarditis). Much of this inflammation may go away, but the heart valves are at risk of chronic damage. The mitral and aortic valves are most often affected. Nodules typically develop on the leaflets of the mitral valves and irreversibly affect their function.
Features of the course of rheumatism in children
Rheumatic fever is more severe in children than in adults. The leading clinical form is carditis; heart defects form more often and faster in children.
Articular syndrome in children is less pronounced, and other extracardiac manifestations (annular rash, subcutaneous nodules, chorea) are more common with more pronounced manifestations.
But, despite its more severe course, the disease in children responds better to drug treatment, and relapses can be avoided. If symptoms of rheumatism appear, hurry up and show your child to the pediatrician. Do not deny your child medical care, follow all recommendations, all the appointments of the pediatrician, this can be vital.
Statistics of rheumatic diseases
In recent years, rheumatic diseases (and other cardiac disorders) have been diagnosed in both older and younger people.
Chronic heart disease can be detected in adolescent children. Trends towards lowering the age threshold lead to an increase in the mortality rate.
To avoid CRHD, you need to lead an active lifestyle, eat right, and not take medications unnecessarily.
It often happens that a person takes precautions, but the disease still appears. The thing is that cardiac diseases are inherited or occur against the background of other pathologies.
conclusions
In order to reduce the incidence of rheumatism, it is important to carry out primary prevention measures: preventing the spread of streptococcal infection in children's institutions, sanitizing foci of chronic infection (tonsillitis, adenoiditis, sinusitis, carious teeth). If there is a family history in children who have had streptococcal tonsillitis, close attention should be paid to nonspecific symptoms and treatment of rheumatism of the heart should begin immediately. To prevent secondary attacks and progression of the disease, long-acting forms of penicillin are recommended.
The duration of extencillin prophylaxis depends on the severity of the process suffered (from 5 years in uncomplicated cases to lifelong use in patients with mature valve disease). In adulthood and old age, a consequence of rheumatism is the formation of heart defects (mitral, aortic stenosis and insufficiency), requiring surgical intervention.
Symptoms of IHD
A dangerous disease is coronary heart disease (CHD). It manifests itself as follows:
- Pain occurs in the chest; as a rule, they are stabbing in nature. As an attack develops, the person feels as if there is a burning sensation in the chest. The duration of pain is from 2.5 to 16 minutes. If chronic coronary heart disease worsens, this symptom appears with varying frequency.
- A sign of IHD is shortness of breath. It is due to the fact that the body does not have enough oxygen. Shortness of breath appears against the background of a painful attack. The peculiarity of the symptom is that it occurs at rest.
- Heart rhythm disturbances are also characteristic of ischemic heart disease. There is a rapid heartbeat, and the beats are quite strong; in other situations they are weak.
- The malaise is accompanied by dizziness. Some people faint.
- Ischemia is manifested by profuse sweating and vomiting.
- A characteristic symptom of the disease is angina. This is a severe attack, manifested by pain in the chest and abdomen. Sharp pain also radiates to the limbs.
Chronic diseases are more difficult to treat. To reduce symptoms, you need to eliminate the root causes of the pathology. IHD proceeds hidden at the initial stages.
In addition to this disease, there are many others that are asymptomatic. In this regard, it is necessary to use medical monitoring methods and monitor the patient’s condition.
A common disease is heart disease. If it progresses, then permanent damage to the heart valve is observed.
A violation of this nature is a sign of chronic rheumatic carditis. It is worth saying that this disease occurs against the background of rheumatic fever.
There are cases when the cause of rheumatic carditis is tonsillitis and pharyngitis. If a doctor diagnoses rheumatism or any other cardiac pathology, then it is necessary to identify its true origins.
Chronic rheumatic diseases can be caused by sore throat. There are cases when treatment of rheumatic pathology is unsuccessful - then death occurs.