Atherosclerosis of the renal arteries involves thickening of the walls and narrowing of the lumen of the renal arteries as a result of cholesterol deposits inside the vessel. In most cases, it occurs as a chronic disease that impairs the blood supply to the kidneys. The main danger is the risk of renovascular symptomatic hypertension, which entails a threat to the patient’s life. In another case, chronic lack of blood supply can lead to the development of renal failure.
Risk factors include:
- elderly age;
- hereditary predisposition;
- smoking and alcohol;
- sedentary lifestyle;
- diabetes;
- excessive consumption of fatty and fried foods;
- overweight.
Symptoms
During its development, atherosclerosis of the renal arteries goes through several stages:
Latent stage - during this period there are no symptoms of the disease, and the presence of pathology can only be seen using laboratory and instrumental research methods. This stage can last for several years.
Stage 1 of the disease - an increase in ischemic disorders occurs in the kidney tissues, and the only symptom is an increase in blood pressure. In addition, an increase in protein can be seen in a urine test.
Stage 2 of the disease – the process of blood clot formation begins in the renal vessels. This is accompanied by symptoms of general intoxication in the form of vomiting and fever. In addition, there is pain in the lower back with irradiation to the lower abdomen and groin area.
Stage 3 of the disease – the nephrons of the kidneys begin to die, which entails the formation of renal failure and more severe arterial hypertension.
Causes of development of renal artery stenosis
Among the diseases that provoke renal artery stenosis, the most common are atherosclerosis and fibromuscular dysplasia .
Atherosclerotic, that is, accompanied by the formation of plaques in the arteries from pieces of tissue detached from the walls, renal artery stenosis is usually a companion to diabetes mellitus, coronary heart disease or arterial hypertension.
In this case, plaques in most cases are concentrated in the area of the aorta, which is fraught with the most severe consequences for the patient.
Fibromuscular dysplasia as a cause of stenosis is often a hereditary pathology and is much more common in women aged 30-45 years. This disease is a thickening of fibrosis or muscle tissue covering the tissue of artery walls.
In some cases, renal artery stenosis can be provoked by arterial aneurysms, arteriovenous shunts, nonspecific aortoarteritis, thrombosis or embolism of the renal arteries, compression of the renal vessels by a foreign body or tumor, and nephroptosis.
Treatment
Treatment begins with eliminating provoking factors, namely adjusting the diet, increasing physical activity, eliminating bad habits, and so on.
The nephrologist selects an individual treatment regimen for each patient, depending on the stage of the disease and the degree of changes in the renal tissue. Drug treatment is carried out with the help of antiplatelet agents, angioprotectors, antispasmodics, lipid-lowering agents and hypertensive therapy.
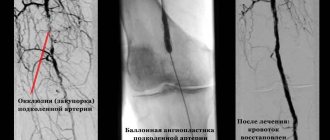
In case of advanced disease and a high risk of blood clots, surgical treatment is used. There are three main methods of surgical interventions:
- stenting;
- bypass;
- prosthetics.
With timely treatment of this condition, there is every opportunity to avoid further complications and make a favorable prognosis for the patient’s life.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Appointment (examination, consultation) with a cardiovascular surgeon, primary, therapeutic and diagnostic, outpatient | 1 750 | — |
| Program “Risk of atherosclerosis and ischemic heart disease, predisposition to dyslipidemia” | 19 000 | — |
* You can read more about the conditions here - Treatment on credit or in installments.
Types and stages of atherosclerosis
The classification is based on the localization of the pathological process and which organ is experiencing insufficient blood circulation.
The following types of atherosclerosis are distinguished:
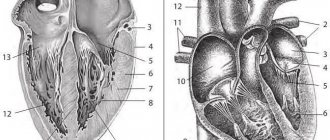
- coronary - blockage of heart vessels;
- cerebral - blocking the lumen of brain vessels;
- aorta - abdominal or thoracic cavity;
- renal arteries;
- arteries of the upper extremities;
- obliterating - blockage of the arteries of the lower extremities;
- penile arteries.
Stages of development (pathogenesis) of atherosclerosis:
- Fat layer stage - small lipid spots (1–2 mm) are present on the walls of blood vessels. These spots grow and merge with each other. Normally, macrophages destroy them and transform them into foam cells, from which fatty stripes subsequently appear. This process does not directly indicate the development of atherosclerosis.
- Stage of fibrous plaques - fatty stripes are transformed into connective tissue, from which fibrous plaques themselves are formed, which pose a great danger to the head vessels, lower extremities and heart. At first, these plaques are soft, but if detected early and competent care is provided to the patient, they are easily dissolved. If this situation is neglected, the plaques harden, as calcium salts are deposited in them.
- Stage of complex disorders - at this stage, the integrity of fibrous plaques is disrupted, they crack and rupture. Platelets attach to them and the vessel is blocked - completely or partially.
Causes of atherosclerosis
The development of atherosclerosis, like all other diseases, has a number of reasons. unhealthy diet - predominance of fatty foods in the diet;
- excess weight;
- diabetes;
- smoking and alcohol abuse significantly increases the risk of developing atherosclerosis;
- heredity;
- sedentary lifestyle;
- high blood pressure;
- the presence of ischemic pathology;
- failure to react to glucose;
- pathologies of the heart and aorta;
- gout.
The exact causes of the development of atherosclerosis are not fully understood; scientists believe that the beginnings of this pathology appear at a young age. However, atherosclerosis reaches its clinical significance in people of the older age group - after 45–50 years. All of the above are risk factors, and if they are managed correctly, you can significantly slow down the progression of the disease, reduce its severity and prevent the development of dangerous complications.
People at risk need to regularly monitor the level of “bad” cholesterol, which is deposited on the walls of blood vessels and causes the formation of atherosclerotic plaques. If the concentration is increased, you should consult a physician, vascular surgeon or cardiologist. If indicated, the doctor will recommend taking statins - drugs that reduce the level of “bad” cholesterol, and, therefore, prevent the development of atherosclerosis.
Who is at risk
Every person, regardless of gender and age, can develop atherosclerosis of the coronary arteries. This is facilitated by many factors, ranging from social reasons to poor ecology. Guidelines for assessing risk factors for the development of cardiovascular diseases, developed on the basis of many years of research in the field of cardiology, highlight the following indicators:
- Men aged 50-55 years;
- Difficult working conditions due to professional activities;
- Hereditary heart pathologies;
- Obesity;
- Smoking, including passive smoking;
- Psychological disorders – stress, depression, depression;
- Thyroid diseases;
- Poor nutrition, the definition includes fried, fatty, sweet and flour foods, fast food.
A systemic risk assessment for the next 10 years can be made independently using the well-known SCORE (Systemic COronary Risk Evaluation) scale proposed by American cardiologists. The modern pace and rules of life put every second person at risk. Therefore, it is difficult to find a better prevention of atherosclerosis of the heart vessels than regular preventive examinations. At the slightest suspicion, it is better to consult a cardiologist and adjust your lifestyle than to undergo long-term treatment, which does not always have a positive outcome.
Basic diagnostic methods:
- Clinical method
- more than half of the information about atherosclerotic lesions comes from a thorough initial examination of the patient, collection of complaints and anamnesis of the disease. - Electrocardiography (ECG)
- shows changes in the heart muscle and heart function caused by atherosclerosis. - Daily monitoring of the electrocardiogram according to Holter
is a widespread method of functional diagnostics, which is used to detect heart rhythm disturbances and ischemic (atherosclerotic) changes in the heart muscle. - Bicycle ergometry
- evaluates the functioning of the respiratory and cardiovascular systems during physical activity, and, in the presence of pathology, is able to identify insufficient function of organs affected by atherosclerosis - Echocardiography
- using ultrasound waves, the work of all parts of the heart is assessed in real time. - Duplex scanning of arteries
is a visual diagnostic method that allows you to “see” the degree of narrowing of the vascular bed, assess the size and structure of the atherosclerotic plaque, its integrity and measure the speed of impaired blood flow in the affected artery. - Magnetic resonance imaging angiography
(MRI angiography) is one of the newest methods for diagnosing vascular diseases. It is possible to obtain images of the vessels of the head and neck without the introduction of any contrast agents. The absence of radiation exposure makes this study absolutely safe for humans. - Multislice computed tomography angiography
allows screening patients for surgical treatment on an outpatient basis due to the non-invasiveness of the method, effectively solving complex diagnostic problems based on the data obtained on the topography of anatomical areas in three-dimensional reconstruction mode, and visualizing any vessels of the human body more than 2 mm in diameter. - Angiography
is the diagnosis of atherosclerotic lesions of almost any arterial system, with visualization of the degree of stenosis, the relationship of the arteries with the surrounding anatomical structures, and possible individual variations in the structure of the arterial bed. The method is considered invasive (requiring surgical intervention), and is prescribed according to strict indications, when the question of possible surgery arises.
Mechanism of development of atherosclerosis
The main role in the pathogenesis of the disease is played by an imbalance between blood lipid fractions. With a decrease in the level of high-density lipoproteins (found in vegetable fats, fish, seafood, cheese) and an increase in high-density lipoproteins (animal fats), the latter are deposited in the wall of blood vessels. This is preceded by local damage to the inner wall of the arteries. Smoking, low levels of antioxidants, and certain viruses and bacteria play a role in this.
Stages of development of atherosclerotic disorders:
- Lipid spot stage
. The plaque does not rise above the level of the vessel wall, does not manifest itself clinically, and is not determined by any research methods during life. - Stage of liposclerosis
. Connective tissue fibers grow into the lipid mass. This makes the plaque more dense, it protrudes into the lumen of the vessel and impedes blood flow in this area. - Stage of atherocalcinosis
. Foci of calcification appear in the plaque and salts are deposited. The plaque completely hardens and is not subject to reverse development. This is where ulceration of the plaque and blood clotting in the vessel begins, which leads to thrombosis.
Atherosclerosis of the arteries of the lower extremities
Damage to the arteries of the lower extremities is called obliterating atherosclerosis. People over 65 years of age, especially men, are susceptible to it. This disease manifests itself in the following symptoms:
- pain in the calves, cramps at rest;
- pain when walking, causing you to limp;
- numbness in the legs, fatigue when walking;
- the appearance of non-healing wounds, and in advanced cases - ulcers.
If you do not consult a doctor in the presence of such symptoms, then there will be a threat of limb amputation as the only treatment measure for extremely advanced cases of obliterating atherosclerosis.
Risk factors for the development of atherosclerosis
All factors that can lead to the development of atherosclerotic lesions can be divided into 3 groups: controllable (we can influence them), uncontrollable and relatively controllable.
Controllable risk factors:
- a diet rich in animal fats, trans fats, insufficient consumption of plant foods;
- smoking;
- sedentary lifestyle.
Uncontrollable risk factors:
- heredity;
- age over 55 years;
- male gender.
Relatively controllable factors
ー chronic diseases that lead to metabolic disorders. They cannot be cured, but can be controlled with diet and medication. These include type 2 diabetes mellitus, hypertension, obesity, and severe infectious diseases (for example, tuberculosis).