A pathological condition in which a person’s heartbeat rhythm is disturbed is called arrhythmia. Arrhythmia is divided into two types - tachycardia (increased rhythm) and bradycardia (slowed rhythm). It is often difficult for a non-specialist to understand from his own feelings how tachycardia and bradycardia differ.
Tachycardia
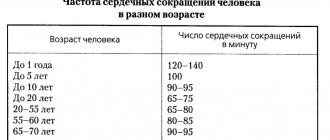
During attacks of tachycardia, the heart begins to beat faster than 90 beats per minute. If such a condition occurs as a result of physical activity or stress, then it is not considered a pathology and does not require treatment. But if there are signs of tachycardia that appear at rest, you should consult a cardiologist.
Types of tachycardia: sinus (rhythm disturbance of the sinus node in the right atrium), paroxysmal (rhythm disturbance outside the sinus node) and ectopic (differs from paroxysmal in that it develops very slowly).
Pathological tachycardia is caused by the following factors:
- myocardial damage;
- myocarditis,
- cardiac ischemia;
- birth defects;
- cardiomyopathy;
- complications after drug therapy.
Ventricular tachycardia cardioversion. Cardiac arrythmia
Arrhythmias requiring emergency treatment
Drugs and electrotherapeutic measures are used to treat arrhythmias. Antiarrhythmic drugs are used to treat hemodynamically stable arrhythmias, and electrotherapy for hemodynamically unstable arrhythmias. Electrotherapy includes:
- defibrillation or cardioversion
- stimulation for tachycardias (for example, treatment of ventricular tachycardias or atrial flutter)
— stimulation for bradycardia in the form of temporary transvenous or transcutaneous pacemakers (=pacemakers).
Defibrillation. During defibrillation, simultaneous depolarization of myocardial cells occurs, which creates a short-term asystole, during which the physiological pacemaker can again assume its function. The condition for this is a sufficient content of energy phosphates in myocytes.
Semi-automatic defibrillators (AED - automatic external defibrillator) are often used, installed in airports, shops, etc.
Cardioversion (or synchronized defibrillation) - electric shocks are given at a certain point in the cardiac cycle (synchronized with R-waves). The defibrillator recognizes the R wave and gives an impulse a few milliseconds after its maximum part and acts on the myocardium during the period of its repolarization. This prevents the development of possible ventricular fibrillation.
Therefore, cardioversion can only be used if there are R-waves on the ECG. Indications: atrial fibrillation, supraventricular and ventricular tachycardia. Defibrillation is used in unconscious and pulseless patients. The discharge during cardioversion is less than during defibrillation and ranges from 50 (atrial fibrillation) to 200 J (polymorphic ventricular tachycardia).
Bradycardia occurs when the heart rate is less than 60 bpm. For emergency situations, bradycardia with a heart rate less than 40 per minute is important. If the cause is known—electrolyte disturbances, increased vagal tone, cardiac tamponade, myocardial ischemia—then it is necessary to eliminate them.
For severe but hemodynamically stable bradycardia, atropine is first prescribed. However, it is necessary to exclude AV block below the His bundle (trifascicular block in the bundle branches), while the heart rate is about 30, the QRS complexes are deformed, dilated, the atria and ventricles contract independently of each other. Secondarily, catecholamines . If bradycardia persists, then a temporary pacemaker .
Atropine can be administered at a dose of 0.5-1 mg every 2-5 minutes up to a maximum dose of 0.04 mg/kg (70 kg person - approximately 3 mg). If IV access is not available, insertion into the endotracheal tube is acceptable. In this case, the dose is increased by 2-3 times and atropine is diluted in 10-20 ml of physiological solution. With blockade below the His bundle (2nd degree AV block, Mobitz II, III degree), atropine can lead to a paradoxical further decrease in frequency and worsening of the condition. In such cases, catecholamines are first used, or even better - stimulation right away.
Catecholamines (orciprenaline and adrenaline). They are used if the heart rate does not increase after atropine and immediately upon the onset of asystole along with resuscitation measures.
In such cases (when catecholamines are used for bradycardia), implantation of a pacemaker is necessary.
Catecholamines are administered as a bolus - orciprenaline 0.25-0.5 mg and/or adrenaline 0.02-0.1 mg (endotracheal administration 2-3 times the dose increased by 10-20 ml of saline solution).
Indications for a temporary pacemaker (artificial pacemaker):
— in case of myocardial infarction with the development of AV block of the second degree Mobitz II with a frequency of 2:1 and higher, AV block of the third degree, progressive block of both fibers
- for symptomatic bradycardia before implantation of a permanent pacemaker
- in case of intoxication with bradycardia
- in other emergency conditions with asystole or symptomatic bradycardia refractory to atropine.
Table 1. Tactics for bradycardia.
With tachycardia, the heart rate is more than 100 beats per minute. For emergency situations, tachycardia with a heart rate of more than 150 beats per minute is important. For the treatment tactics of tachycardia, hemodynamically stable and hemodynamically unstable tachycardias are distinguished.
For hemodynamically unstable tachycardias . which are accompanied by shock symptoms, loss of consciousness, pulmonary edema, antiarrhythmic drugs, defibrillation or cardioversion are urgently used. Treatment of hemodynamically stable patients depends on the type of tachycardia.
The strength of the shock during defibrillation depends on the type of tachycardia. For example, tachycardias with narrow QRS complexes, against the background of atrial fibrillation, respond well to a discharge of 50-100 J. Polymorphic ventricular tachycardias and ventricular fibrillation are defibrillated with a discharge of 200-300 J; if ineffective, the charge increases to 360 J. With persistent ventricular fibrillation Along with resuscitation measures, amiodarone (150-300 mg IV) is administered.
If the patient requires defibrillation or cardioversion and is conscious, sedatives (eg, midazolam) or analgesics (eg, morphine) are used before the procedure. The choice of analgesic should be based on the hemodynamic and respiratory status of the patient. If consciousness is maintained before cardioversion, amiodarone can be administered intravenously.
Rice. 1. Ventricular fibrillation.
Hemodynamically stable tachycardias are treated with medication. A 12-lead ECG is performed. According to ECG, tachycardia is divided into 2 groups, which require different treatment. To differentiate supraventricular and ventricular tachycardias, the decisive criterion is the width of the QRS complex. When the width of the QRS complex is less than 120 ms, arrhythmias originate above the His bundle - supraventricular. The exception is supraventricular tachycardias with bundle branch block and the presence of an additional bundle in Wolff-Parkinson-White syndrome (the QRS complex will be wider than 120 ms, but the tachycardias are supraventricular). When the QRS complex is more than 120 ms - ventricular tachycardia.
Table 2. Tactics for tachycardia.
Atrial fibrillation, atrial flutter. The QRS complex is less than 120 ms, the RR intervals are not the same. Treatment - either slow down conduction in the AV node (verapamil, β-blockers, glycosides), or cardioversion. Cardioversion can be performed only when atrial fibrillation has been present (documented) for less than 48 hours or thrombi in the atria of the heart have been excluded using intraesophageal ultrasound. In all other cases, normalize the rate and plan, if indicated, elective cardioversion.
Rice. 2. Atrial fibrillation and normal sinus rhythm.
Regular tachycardias with narrow QRS complexes. These are supraventricular tachycardias. First, vagal tests are used (carotid sinus massage, Valsalva maneuver). If ineffective, a bolus of adenosine is administered intravenously (6-12-18 mg in increasing order). In 95% of cases, such tachycardias disappear after adenosine. As an alternative or if adenosine is ineffective, calcium antagonists (verapamil 2.5-5 mg IV) and β-blockers are used. If even after these measures the tachycardia does not go away, then flecainide and propafenone are used.
Rice. 3. Supraventricular tachycardia.
Rice. 4. Supraventricular tachycardia and the effect of adenosine.
Tachycardia with wide QRS complexes. Typically of ventricular origin (80%). In some cases, however, it is supraventricular, when there is an additional abnormal path of impulse conduction from the atria to the ventricles (for example, in Wolff-Parkinson-White syndrome).
Rice. 5. Delta wave in Wolff-Parkinson-White syndrome.
When treating hemodynamically stable tachycardias with wide QRS complexes, many mistakes are made, because tachycardias of ventricular origin are incorrectly interpreted as supraventricular with bundle branch block. It is incorrectly believed that all tachycardias with normal hemodynamics and wide QRS complexes are necessarily supraventricular with bundle branch block. Therefore, any tachycardia with wide QRS complexes should be considered ventricular until proven otherwise. In some cases, however, when a supraventricular origin of wide QRS tachycardia is suspected, a bolus of adenosine can be administered for diagnostic purposes.
Rice. 6. Monomorphic ventricular tachycardia.
For such tachycardias, hemodynamically stable with wide monomorphic regular QRS complexes, amiodarone or, as an alternative, ajmaline is recommended. The use of ajmaline is practiced in Germany. One of its advantages is that it also has a beneficial effect on supraventricular tachycardias. It can also be used for atrial fibrillation with Wolff-Parkinson-White syndrome, while adenosine, verapamil and cardiac glycosides are contraindicated. One of the reasons is that conduction through the anomalous additional bundle is accelerated due to the shortening of the refractory period of the cells of this bundle and the simultaneous slowdown of conduction in the AV node.
Also, for such tachycardias in cases where there is a heart attack or ischemic damage, lidocaine is sometimes used. Other antiarrhythmics, such as propafenone, flecainide, play a secondary role as reserve drugs.
When treating polymorphic ventricular tachycardias, it is of great importance to identify “torsades de pointes” arrhythmias against the background of congenital or acquired syndrome of prolongation of the QT interval. The ECG shows a typical sinusoidal waveform on the ECG. Pathogenesis - there are multiple areas of discharged myocardium, so drugs that slow down repolarization, such as sotalol and ajmaline, cannot be used. Magnesium is prescribed in high doses (1-2 g IV) or b-blockers, catecholamines, lidocaine, electrical stimulation.
Rice. 7. Tachycardia of the “pirouette” type.
For polymorphic ventricular tachycardias, which are not a consequence of delayed repolarization, but, for example, arose as a result of ischemic changes or dilated cardiomyopathy, amiodarone is used intravenously (150-300 mg). At the same time, correction of electrolyte disturbances and treatment of ischemic changes should be carried out. It is also possible to use β-blockers and lidocaine.
Rice. 8. Polymorphic ventricular tachycardia.
Tests on the topic arrhythmia.
1). What medications are used to treat life-threatening bradycardia?
a) sodium channel blockers, such as lidocaine, which affect the spontaneous depolarization of pacemaker cells to increase heart rate
b) only adrenaline, because with bradycardia it is very important to increase blood pressure
c) intravenous or endotracheal administration of atropine or catecholamines
d) statins and ACE inhibitors are used together with β-blockers to have a long-term effect on risk factors for cardiovascular diseases
e) There are no medications to treat life-threatening bradycardia.
2). What is the best thing to do for hemodynamically unstable bradycardia that is resistant to medications?
a) mouth-to-nose artificial respiration
b) external cardiac massage through the chest
c) percutaneous or transvenous endocardial stimulation, before this, if necessary, external cardiac massage
d) continuation of alternate administration of atropine and adrenaline
e) defibrillation to activate the pacemaker
3). What parameter should be used when choosing a method of therapy (defibrillation or drug treatment) for tachycardia?
a) according to heart rate on the ECG
b) the width of the QRS complex is decisive
c) due to underlying heart disease
d) by hemodynamic stability or instability during tachycardia
e) according to the patient’s subjective sensations of pain
4). What should be done in case of hemodynamically unstable tachycardia with progressive loss of consciousness?
a) administration of adenosine in increasing doses
b) immediate IV administration of amiodarone is better than all other measures, especially the administration of other drugs
c) rapid cardioversion or defibrillation
d) intubation and intravenous administration of catecholamines to stabilize blood circulation
e) endocardial stimulation to stop tachycardia
5). What is the optimal treatment for hemodynamically stable atrial fibrillation of unknown duration?
a) oral anticoagulants to reduce the risk of stroke
b) cardioversion to restore rhythm and prevent electrical remodulation of the myocardium
c) drug frequency control, cardioversion after excluding thrombi in the atria of the heart
d) class IC antiarrhythmics for painless cardioversion without prior exclusion of thrombi
e) potassium, magnesium and amiodarone
6). What treatment is recommended for symptomatic atrial flutter?
a) rapid cardioversion due to the danger of the impulse passing through the AV node with a frequency of 1:1
b) with an accurate diagnosis, administration of adenosine
c) the same as with atrial fibrillation
d) emergency catheter ablation of the cavo-tricuspid isthmus
e) anticoagulants for several weeks, because the risk of thromboembolic complications is as high as with atrial fibrillation
7). What treatment is used for hemodynamically stable rhythmic tachycardia with narrow QRS complexes?
a) adenosine after vagal tests, alternatively if verapamil or class IC antiarrhythmics are ineffective
b) cardioversion with energy 50-100 J
c) amiodarone (300 mg/30 min) followed by administration for 7-10 days at a rate of 50 mg/h
d) electrical stimulation via transvenous electrodes
e) cardiac glycosides, potassium and magnesium
8). Regular tachycardias with wide QRS complexes:
a) are supraventricular tachycardias with bundle branch block
b) supraventricular tachycardia with bundle branch block in cases where they do not lead to hemodynamic instability
c) tachycardias of ventricular origin and until evidence to the contrary should be treated as ventricular tachycardias
d) tachycardia with additional conduction bundle during atrial flutter
e) tachycardia due to prolongation of the QT interval
9). What is used for polymorphic ventricular tachycardia in connection with prolongation of the QT interval?
a) ajmaline to stop tachycardia and shorten the QT interval
b) IV magnesium and lidocaine, as well as stimulation and catecholamines to increase heart rate
c) IV amiodarone for effect on the QT interval
d) sedation, for example, diazmepam
e) class Ic antiarrhythmics (flecainide, propafenone), with signs of heart failure additionally cardiac glycosides
Bradycardia
Bradycardia is a condition in which the heart rate slows to 50–30 beats per minute. A slow pulse is considered normal in athletes and young healthy people (if the person does not experience discomfort, dizziness or fainting).
With a reduced heart rate, a person feels dizzy and weak, and cold sweat appears. Due to slow blood flow, organs do not receive enough oxygen. In some cases, fainting may occur.
Bradycardia occurs sinus and with heart block. It develops against the background of the following diseases:
- sclerotic changes in the myocardium;
- meningitis;
- brain tumor;
- hypothyroidism;
- liver damage;
- typhoid fever.
Bradycardia also develops with nicotine, lead poisoning or as a result of drug treatment with glycosides.
Arrhythmias
07.08.2018
The optimal heart rate for the body at regular intervals is considered to be 60-80 beats per minute. Any difference from normal sinus rhythm in the heart is called an arrhythmia. heart diseases, the proportion of arrhythmias is quite high, and in comparison between men and women, men lead in the number of this condition. In men, the development of arrhythmia is 1.5 times more common. According to statistics, arrhythmia accounts for more than 15% of all heart diseases, and in the absence of the necessary treatment, this leads to serious consequences for the body.
There are a huge number of reasons that disrupt heart rhythm, for example: various cardiac diseases, a number of endocrine pathologies, drug intoxication, age-related changes in the myocardium, nicotine and alcohol poisoning, etc.
According to the nature of their development, arrhythmias can be permanent or transient, acute or chronic. Clinical forms of arrhythmias are considered to be tachycardia , bradycardia, extrasystole, disturbance of intraventricular and atrioventicular conduction, and sinus node dysfunction.
What is tachycardia?
An increase in heart rate is called tachycardia and can be either a natural or pathological phenomenon. Physiologically, the number of heartbeats increases as a result of physical activity or stress. Rapid heartbeat does not allow the ventricles of the heart to fill completely and, accordingly, reduces the filling of the arteries , which leads to a decrease in blood pressure and limits the flow of blood to the organs, and the deterioration of blood supply limits the amount of oxygen entering the heart and provokes ischemia.
What is bradycardia?
A decrease in the automaticity of the sinus node, leading to a decrease in heart rate, is called bradycardia. The reasons leading to bradycardia are varied. These may include sclerotic changes in the myocardium and increased intracranial pressure, nicotine poisoning and thyroid , as well as the consequences of taking certain medications. Small changes do not cause any negative sensations, but with a significant decrease in the rhythm dizziness , weakness, cold sweat and fainting appear. Fainting conditions become especially dangerous; there is a high risk of sudden cardiac .
What is heart block?
A disorder that occurs independently or develops against the background of other diseases, characterized by a slowdown or absence of impulse transmission through the heart muscle, is called heart . Classification and treatment of the disease is based on the part of the heart it (the disease) occurs. Atrioventricular or atrioventricular blockades develop due to disturbances in the conduction of impulses from the atria to the ventricles. Impairment of impulse conduction in the His bundle is called ventricular block .
An electrocardiogram can successfully diagnose the disease, and Holter monitoring or echocardiography can help determine periodically occurring blockages.
If you suspect any heart , contact a cardiologist !
Published in Cardiology Premium Clinic
Diagnosis of tachycardia and bradycardia
When visiting a therapist, the doctor will prescribe a number of tests. The main type of diagnosis of arrhythmia is an ECG. There are many ECG signs to identify one or another type of arrhythmia. After the doctor determines what type of arrhythmia is developing in the patient, he will prescribe the optimal treatment.
The Medicenter clinic network employs qualified cardiologists and has modern equipment installed. With us you can undergo a comprehensive examination, establish or confirm your diagnosis and receive treatment recommendations.