IVH has recently become a significant problem in pediatric neurosurgery. This is explained by the improvement in the quality of nursing for premature babies with low birth weight. According to the literature, among children weighing less than 2500 g, IVH occurs in 60% of cases. Neurosurgical assistance is required for children with severe IVH, leading to the development of progressive hydrocephalus. The severity of intraventricular hemorrhages directly depends on the degree of prematurity. The year 2012 was marked by the adoption of WHO live birth standards. Currently, babies weighing 500 grams are considered live births. Nursing children with extremely low body weight is significantly complicated by the high incidence of severe IVH among them. This is a category of patients for whom the timeliness and skill of providing assistance to them largely determines the degree of further disability. Providing assistance to this category of patients begins at the stage of the maternity hospital. The visiting team assesses the condition of the newborn patient and assesses his transportability.
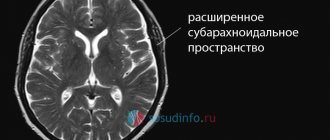
The enlarged lateral ventricles of the brain are clearly visible. The severity of the condition is largely explained by severe intracranial hypertension.
In such cases, we begin treatment with a series of lumbar punctures. Contraindications to lumbar puncture may be the presence of occlusion or a bulging blood clot in the lumen of the ventricles. Sometimes it is possible to compensate for the process with a series of lumbar punctures. To reduce ICP we perform ventricular punctures. Multiple ventricular punctures are not advisable, since it has been proven that frequent ventricular punctures lead to the development of porencephalic cysts. Thus, for long-term unloading of the ventricular system, it is often necessary to resort to various drainage operations. For example, ventriculostomy followed by external drainage. This manipulation is performed under ultrasound control in order to visually control the placement of drainage into the lumen of the lateral ventricle. The image clearly shows the catheter in the lumen of the right lateral ventricle.
This image was taken intraoperatively:
This is necessary because drainage is sometimes left standing for a long time. Against the background of drainage, as a rule, hypertensive symptoms are relieved, hemodynamics are normalized, convulsive syndrome is stopped, and breathing is normalized.
The complexity of the situation is that, against the background of various drainage methods, it is extremely rare to achieve final normalization of liquor outflow. This condition is usually resolved by shunt surgery. But here, too, not everything is simple. It is sometimes possible to achieve cerebrospinal fluid sanitization sufficient to install a shunt only after 1-2 months. This turns this category of patients into a big problem for the department. External drainage requires constant attention and poses a serious risk of infection of the drainage system and the development of ventriculitis. For the last 6 years, we have practically not used external drainage in newborns.
Closed drainage techniques are used, such as the subgaleal reservoir and the installation of Omaya type reservoirs. We use these techniques as the first stage of treatment of hydrocephalus in premature infants with IVH, which allows us to delay shunt implantation until the cerebrospinal fluid is completely sanitized.
Subgaleal reservoir.
The essence of the method is to install a silicone catheter into the lateral ventricle and remove it into a reservoir formed under the aponeurosis. Liquor from the ventricular system rushes into the subaponeurotic reservoir, from where it can be periodically evacuated painlessly.
The reservoir is punctured with a thin intradermal needle 1 to 3 times a week, removing accumulated cerebrospinal fluid and introducing solutions of antiseptics and antibiotics. If possible, I transfer the patient to a day hospital for psychological rehabilitation of the mother. The reservoir acts as a receiver, port and shock absorber and allows for control of ventriculomegaly.
The advantage of this technique compared to external drainage is that it allows sanitization of the liquor system with minimal risk of infection and greatly facilitates patient care. Compared to external drainage, we obtained more encouraging results.
Manifestations of IVH in young children
Up to 90% of all hemorrhages in the ventricular system occur in the first three days of a baby’s life, and the lower his weight, the higher the likelihood of pathology. After the first week of a child’s life, the risk of hemorrhage decreases significantly, which is associated with the adaptation of the vascular system to new conditions and the maturation of the structures of the germinal matrix. If the child was born prematurely, then during the first days he should be under close supervision of neonatologists - on the 2-3rd day the condition may worsen sharply due to the onset of IVH.
Small subependymal hemorrhages and grade 1 IVH may be asymptomatic. If the disease does not progress, the condition of the newborn will remain stable, and neurological symptoms will not even arise. With multiple hemorrhages under the ependyma, signs of brain damage will appear closer to a year with the phenomena of leukomalacia.
A typical intracerebral hemorrhage is manifested by symptoms such as:
- Decreased muscle tone;
- Sluggish tendon reflexes;
- Breathing disorders up to stopping (apnea);
- Convulsions;
- Focal neurological symptoms;
- Coma.
The severity of the pathology and the characteristics of the symptoms are associated with the volume of blood entering the ventricular system and the rate of increase in pressure in the cranial cavity. Minimal IVH, which does not cause obstruction of the cerebrospinal fluid ducts and changes in the volume of the ventricles, will be accompanied by an asymptomatic course, and it can be suspected by a decrease in the hematocrit number in the baby’s blood.
An intermittent course is observed in moderate and submassive IVH, which are characterized by:
- Depression of consciousness;
- Paresis or muscle weakness;
- Oculomotor disorders (histagmus, strabismus);
- Respiratory disorders.
Symptoms with spasmodic flow are expressed over several days, after which they gradually decrease. Both complete restoration of brain activity and minor deviations are possible, but the prognosis is generally favorable.
The catastrophic course of IVH is associated with severe disorders of the brain and vital organs. Characterized by coma, respiratory arrest, generalized convulsions, bluish skin, bradycardia, decreased blood pressure, and thermoregulation disorders. Intracranial hypertension is indicated by the bulging of a large fontanel, clearly visible in newborns.
In addition to clinical signs of impaired nervous activity, there will be changes in laboratory parameters. The occurrence of IVH in newborns may be indicated by a drop in hematocrit level, a decrease in calcium, fluctuations in blood sugar, and often disorders of the blood gas composition (hypoxemia), and electrolyte disturbances (acidosis).
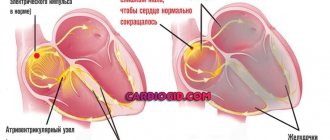
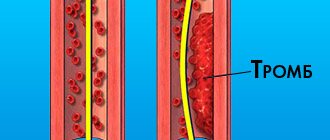
Complications of IVH include blockage of the cerebrospinal fluid pathways by blood clots with the development of acute occlusive hydrocephalus, atrophy of the cerebral cortex and impaired psychomotor development. Impaired circulation of cerebrospinal fluid leads to an increase in the size of the ventricles, an increase in intracranial pressure and compression of the cerebral cortex, which already suffers from hypoxia. The result is convulsive syndrome, depression of consciousness and coma, cardiac and respiratory arrest.
The progression of bleeding leads to the spread of blood from the ventricles into the cisterns of the brain and nervous tissue. Parenchymal intracerebral hematomas are accompanied by severe focal symptoms in the form of paresis and paralysis, sensory disturbances, and generalized convulsive seizures. When IVH is combined with intracerebral hemorrhage, the risk of an unfavorable outcome is extremely high.
Among the long-term consequences of IVH are ischemic-hypoxic damage and residual changes in the brain in the form of cysts, periventricular leukomalacia, white matter gliosis, and cortical atrophy. By about a year, a developmental delay becomes noticeable, motor skills suffer, the child cannot walk or perform correct movements of the limbs in due time, does not speak, and lags behind in mental development.
Diagnosis of IVH in children is based on an assessment of symptoms and examination data. The most informative is CT, neurosonography and ultrasound. CT is accompanied by radiation, so ultrasound is preferable for premature babies and newborns in the first days of life.
IVH on a diagnostic image
US – navigation.
Separately, I would like to dwell on interventions using ultrasound navigation. This type of intervention falls into the category of gentle and minimally invasive. If the surgeon is sufficiently qualified under ultrasound control, manipulations can be performed with high precision. If the child is an infant, then the sensor is installed on the membrane of the large fontanel. In older children, the sensor is placed on the dura mater, for which a trefination hole is applied; often this is not required; it is enough to install the sensor on the temporal bone, which remains “transparent” even in adolescents. Below is an example of the complicated course of hydrocephalus with the so-called. isolation of the fourth ventricle.
In this case, ultrasound navigation made it possible to pass the ventricular catheter through the foramen of Monroe, the third ventricle, recanalize the aqueduct and pass it into the fourth ventricle, thus conducting Panventriculostomy:
On the presented tomograms, a 10-year-old girl has an extensive cyst in the chiasmatic-sellar region, which impedes the outflow of cerebrospinal fluid through the foramina of Monroe and causes occlusive hydrocephalus.
Under ultrasound control, puncture of the cyst was performed through the foramen of Monroe, followed by catheterization and implantation of the Omaya reservoir. Subsequent tomograms confirm the accuracy of catheter placement. Hydrocephalus has decreased significantly.
Subsequently, regular (once a month) punctures of the reservoir were performed, which ensured relief of hydrocephalus. The child attends a regular school. Control MRI after a year. It can be seen that the cyst retains its volume, but the hydrocephalus has been relieved.
A very important problem in pediatric neurosurgery is the problem of purulent diseases. The most common are rhinogenic complications, as in this case contact abscess of the frontal lobe. CM. snapshot:
This example has more academic significance, because... At one time, as in this case, it was customary to remove abscesses openly in the capsule.
Postoperative photo:
It is clearly visible that the brain is straightened. The lateral ventricle is not damaged. Subsequently, after 6 months. The child underwent cranioplasty surgery. Discharged without neurological deficit.
Currently, we practically do not use removal of an abscess in a capsule. Modern techniques are minimally invasive. We carry out catheterization of the abscess under ultrasound navigation and evacuation of pus, which makes it possible to easily cure even small and deeply located abscesses, as in this case in a teenager with Down's disease.
Causes of intraventricular hemorrhages in newborns
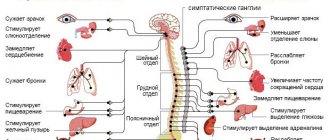
The reasons for the development of IVH in young children are fundamentally different from those that cause hemorrhages in adults. If in the latter vascular factors come to the fore - hypertension, atherosclerosis, which underlie strokes, and the penetration of blood into the ventricles is secondary to intracerebral hematoma, then in newborn babies the situation is somewhat different: hemorrhage immediately occurs inside the ventricles or under their lining , and the reasons are somehow related to pregnancy and childbirth:
- State of prematurity;
- Long waterless period;
- Severe hypoxia during childbirth;
- Injuries during obstetric care (rare);
- Birth weight less than 1000 g;
- Congenital disorders of blood coagulation and vascular structure.
In premature babies, the main cause of intraventricular hemorrhages is considered to be the presence of the so-called germinal matrix, which should gradually disappear as the fetal brain and vascular system mature. If birth occurs prematurely, then the presence of this structure creates the prerequisites for IVH.
The germinal matrix is a region of neural tissue around the lateral ventricles that contains immature cells that move into the brain and, when mature, become neurons or neuroglial cells. In addition to cells, this matrix contains immature capillary-type vessels, the walls of which are single-layered, therefore very fragile and can rupture.
Hemorrhage into the germinal matrix is not yet IVH, but it most often leads to the penetration of blood into the ventricles of the brain. A hematoma in the nervous tissue adjacent to the wall of the ventricle breaks through its lining, and blood rushes into the lumen. From the moment even a minimal volume of blood appears in the ventricle of the brain, we can talk about the onset of an independent disease - intraventricular hemorrhage.
Determining the stages of IVH is necessary to assess the severity of the disease in a particular patient, as well as determine the prognosis in the future, which depend on the amount of blood entering the ventricles and the direction of its spread towards the nervous tissue.
Radiologists base IVH staging on CT scan results. They highlight:
- IVH of the 1st degree - subependymal - blood accumulates under the lining of the ventricles of the brain, without destroying it and without entering the ventricle. In fact, this phenomenon cannot be considered a typical IVH, but at any moment a breakthrough of blood into the ventricles can occur.
- IVH grade 2 is a typical intraventricular hemorrhage without expansion of its cavity, when blood exits the subependymal space. On ultrasound, this stage is characterized as IVH with less than half the volume of the ventricle filled with blood.
- IVH stage 3 - blood continues to flow into the ventricle, filling more than half of its volume and expanding the lumen, which can be observed on CT and ultrasound.
- IVH of the 4th degree is the most severe, accompanied not only by the filling of the brain ventricles with blood, but also by its spread further into the nervous tissue. CT scan reveals signs of IVH of one of the first three degrees along with the formation of foci of parenchymal intracerebral hemorrhage.
Based on structural changes in the brain and its cavities, three stages of IVH are distinguished:
- At the first stage, the ventricles are not completely filled with blood content, they are not expanded, spontaneous cessation of bleeding is possible and normal liquor dynamics are maintained.
- Continued filling of the lateral ventricles with possible expansion, when at least one of the ventricles is filled with blood by more than 50%, and the blood spreads into the 3rd and 4th ventricles of the brain occurs in the second stage.
- The third stage is accompanied by progression of the disease, blood entering the choroid of the cerebellum, medulla oblongata and spinal cord. The likelihood of fatal complications is high.
The severity of IVH and its manifestations will depend on how quickly blood penetrates the brain tissue and its cavities, as well as on its volume. Hemorrhage always spreads along the flow of cerebrospinal fluid. In very premature babies, as well as those who have suffered deep hypoxia, disorders of the blood coagulation system occur, so clots do not appear in the cavities of the brain for a long time, and liquid blood “spreads” unhindered throughout the parts of the brain.
The basis for the disorder of cerebrospinal fluid circulation and the subsequent increase in hydrocephalus is the penetration of blood into the ventricle, where it mixes with the cerebrospinal fluid, but does not immediately coagulate. Some of the liquid blood penetrates into other cavities of the brain, but as it coagulates, clots begin to block the narrow zones through which the cerebrospinal fluid circulates. Blocking any of the openings of the brain entails blockage of the cerebrospinal fluid pathway, dilatation of the ventricles and hydrocephalus with characteristic symptoms.