© Author: A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
The frequency of anomalies of the vein of Galen does not exceed one percent among people of all ages, but up to a third of cases of cerebral vascular defects in newborns and young children are due to this pathology. In male children it is detected twice as often as in girls.
According to statistics, up to 90% of cases of congenital malformations of the vein of Galen end in the death of children at an early age, which is associated both with the severity of the pathology and with the insufficient readiness of specialists to treat the disease, and the lack of equipped neurosurgical and vascular operating rooms. The prognosis is significantly worse in patients who were born with signs of heart failure, hydrocephalus and impaired blood flow in the cerebral hemispheres.
In recent years, mortality has been reduced to 70-80%, and the literature even describes isolated cases of successful control of pathology, which is largely due to progress in the field of ultrasound research methods and the improvement of microsurgical and endovascular techniques in neurosurgery. At the same time, unfortunately, doctors still cannot give parents of babies with anomalies of the vein of Galen any reassuring recommendations.
Anatomy and types of pathology of the great cerebral vein
The vein of Galen is called the great vein of the brain, since it is one of the largest venous trunks, carrying blood saturated with carbon dioxide and metabolic products from the internal parts of the brain - the subcortical nuclei, visual thalamus, transparent septum, plexus of the lateral ventricles.
The great cerebral vein belongs to the deep venous system and runs in the subarachnoid space (it is also called the cistern of the vein of the same name in this area), connecting with the inferior sagittal venous sinus to form the straight sinus. The large vein of Galen flows into the straight sinus.
The anatomy of the vein of Galen depends on the shape of the head. Its length is about 12-14 mm, while in people with a dolichocephalic type of skull (with a long and narrow head) it can reach 2 centimeters, and in brachycephalics with a short and wide head - a little more than a centimeter.
The diameter of the vessel is not related to the shape of the skull and averages 5-7 mm, however, it has been noted that brachycephals have a relatively short but wider trunk than dolichocephals with a long and narrower vein.
The normal speed of blood flow in the vein of Galen in children under one year of age is 4-18 cm/sec.
Among the changes that are most often detected in the vessel in question are:
- Aneurysm of the vein of Galen;
- Arteriovenous malformation of the great cerebral vein.
Alena and Artem: were in the smallest percentage!
On that day, the icon of the Mother of God “The Sign” was brought to the Church on the Blood in Yekaterinburg. Alena Babaeva really wanted to kiss. Her pregnancy was going well. 32 weeks already. It’s just that lately I’ve been having trouble sleeping at night.
It was not difficult to get to the icon: with its belly, people willingly gave way to it. But getting away from it is almost impossible. Tears flowed freely from the unsentimental Alena. Why? She couldn't understand it herself. She only remembers that she left the temple with a firm intention: she urgently needs to do an ultrasound!
At home, her “whim” was not supported. “What kind of nonsense? You just did it today! An excellent doctor looked at me, on recommendation. He said: everything is fine." But Alena stood her ground: it needs to be done urgently!
We signed up for the only medical center that had a “window” left. There was no time to choose, just to be accepted today! Late in the evening, the tired ultrasound technician was probably hoping to finish his work day quickly. But could not. A professional eye could not help but pay attention to this baby. There was clearly a mess in his head. “Most likely, hydrocephalus,” he brought the conclusion down on Alena’s head.
In the morning she was already standing on the threshold of the medical genetic center. Four uzists looked at her with pitiful eyes, not daring to pronounce a verdict. Finally, the council decided: “Malformation of the vein of Galen.” 90% of children with this diagnosis die in utero, of those who survive, 90% die on the first day.
Arteriovenous malformation is a pathological connection between veins and arteries, in which there is no capillary network and arterial blood is directly discharged into the venous blood, depriving the corresponding organ of nutrition. The vein of Galen is one of the main venous collectors of the brain (collects blood from its internal structures). Arteriovenous malformation of the vein of Galen is a rare congenital disease of this vein.
But Alena did not agree. She didn't want to be one of those statistics. Three weeks later she had a caesarean section - and Artem was born. Alive. And he continued to survive. “Then we often ended up in the smallest percentage according to statistics. That is, statistically all this was very unlikely.”
On the third day, Artem had his first stroke - hemorrhage. Alena sent his documents to the three most famous neurosurgical clinics in the country, including in Novosibirsk to the National Medical Research Center named after Academician E.N. Meshalkin.
And then it turned out that Dr. Orlov from this center should come to Yekaterinburg. Having learned about Artyom’s case, he immediately said: “We must save him!” This probably really saved him. Because in all the official responses that came a month later, Artem was refused help: “inappropriate.”
After that life-saving operation (it was the first operation in the Sverdlovsk region to correct a malformation of the vein of Galen, which was successful), Artem underwent nine more neurosurgical operations. Each time, giving her son for surgery, Alena realized that she might be kissing him for the last time.
Aneurysm of the vein of Galen can cause complications in the form of cerebral palsy, hydrocephalus, and epilepsy. Artem suffered all the complications that one can imagine. The most severe of them is West syndrome, a complex form of epilepsy. It was this syndrome that provoked 30 respiratory arrests per day. Artyom lay motionless for days on end, his gaze seemed clouded and absent.
“It was as if he was not with us,” says Alena. “But we managed to defeat West syndrome. The son went into long-term remission, he returned to us, his freed brain began to perform a wide variety of tasks - from picking his nose to crawling.”
By the age of two, Artem was assigned level V according to the GMFCS gross motor function classification system. This meant he would never go. Typically, Level V children remain like this for their entire lives. But after two years, when drugs for epilepsy were selected, his body began to actively respond to rehabilitation. Today he can roll over on his own, get on all fours, stand and walk with support. And its capabilities are assessed as corresponding to level III according to the GMFCS system.
“Even with a walker, he’s already walking! It's incredible, but it's possible! And to all the women who come to me when faced with the same diagnosis, I say: “I always repeat the prayer “Lord! Give me the strength to change the things I can change, the courage to accept the things I cannot change, and the wisdom to know the difference.”
Alena, together with other parents whose children were diagnosed with AVM of the vein of Galen, is creating a support base for “newcomers.” Together they created a website where you can get the necessary information and contact experienced mothers who have already achieved good results.
Even if no pathologies were identified during pregnancy, be careful if you notice the following symptoms in your baby: gets tired quickly during feeding; swelling of the soft tissues of the head; an increase in head circumference beyond the norm; pronounced venous pattern on the head; possible: vomiting, strabismus, convulsions. Be sure to consult a neurosurgeon!
Aneurysm of the vein of Galen
Aneurysm of the vein of Galen is one of the most severe and quite difficult forms of vascular pathology of the brain for early diagnosis and treatment. Unfortunately, it is usually discovered no earlier than the third trimester of gestation, which comes as a real shock to expectant parents, because previous screening ultrasounds showed normal results.
At the same time, a defect identified during pregnancy, albeit quite late, makes it possible to decide on the tactics of treating the baby before birth, choose a clinic and specialist, and psychologically prepare for the fight for the well-being of the child.
An aneurysm of the vein of Galen forms in utero. Initially, the brain structures of a growing embryo are nourished by embryonic vessels, which mature into full-fledged arteries and veins during the first two months of gestation. If this process is disrupted, then in the fetal brain the embryonic vessels remain undeveloped, giving rise to aneurysms and other malformations.
Among the reasons that may contribute to abnormalities in the formation of the vascular bed are:
- Exposure to viruses and bacteria (herpes, rubella, respiratory infections, etc.);
- Taking certain medications;
- Effect of ionizing radiation.
It is important to note that the defect begins in the first third of gestation, but becomes noticeable for diagnosis much later.
From an anatomical point of view, an aneurysm can represent a local increase in the lumen of a vein, but much more often it looks like multiple communications between vessels in the form of a tangle consisting of embryonic-type vessels.
Blood from the arteries of the brain (the internal carotid and vertebrobasilar systems) is discharged into an abnormally formed vein, without sufficiently reaching the nervous tissue of the hemispheres and subcortical formations, which is why the latter experience anemia, and the venous section is overloaded.
Embryonic vessels lack a smooth muscle layer, so they can easily rupture with blood spilling into the nervous tissue, and can also be stretched by excess fluid. Stretching and increasing the diameter of the venous part of the bloodstream contributes to compression of the cerebrospinal fluid pathways and the development of hydrocephalus.
An aneurysm of the vein of Galen is found in the anterior part of the skull, behind and above the visual tuberosities in the cistern of the same name. There are several forms of aneurysm:
- Intramural, when the artery flows directly into the vein.
- Choroidal - represented by choroid plexuses in the choroidal fissure.
- Parenchymal - multiple vascular communications are located in the brain parenchyma.
Video: Vein of Galen aneurysms on ultrasound
Malformation of the great cerebral vein
Malformation of the vein of Galen is a change in the vascular system in which a plexus is found in the form of a tangle, consisting of embryonic-type vessels and, necessarily, an enlarged great vein (aneurysm). That is, malformation always includes an aneurysmal change in the vein.
Malformations are characterized by underdevelopment of the elastic and muscle fibers of the middle tunic of the vein, so even a slight increase in pressure is accompanied by an expansion of the lumen of the vessels, which only worsens over time. An aneurysm may have the appearance of a sac or a diffuse increase in the lumen of the vessel.
Arteriovenous malformation of the vein of Galen can be mural, when the brain arteries approach the aneurysmally dilated vein and flow into it directly, and choroidal - pathologically altered tangles of vessels feeding the malformation, flowing into the dilated vein of Galen.
The malformation together with the aneurysmally dilated vein of Galen puts pressure on the surrounding tissues, promoting their atrophic changes, displacement, blockade of liquor and venous outflow, which causes hydrocephalus to increase.
Video: Vein of Galen malformation
Tributaries
Vein of Galen is one of the most important elements of the circulatory system.
It has tributaries:
- medial tributaries located in the occipital region;
- the anterior superior vessel, which passes through the cerebellum;
- pineal gland;
- internal venous plexuses of the brain;
- Rosenthal vessels;
- posterior venous duct of the corpus callosum.
Manifestations of venous vessel anomalies
Symptoms of abnormalities of the venous bed of the brain appear at birth in half of the babies. The main symptom of an aneurysmal change in the vein of Galen is heart failure associated with increased venous pressure in the cerebral and vena cava, creating excess stress on the child’s heart. Since the aneurysm functions during the prenatal period, by the time of birth the baby has a high probability of cardiac decompensation.
child diagnosed with vein of Galen malformation
Clinical signs of an aneurysm are:
- Rapid fatigue of the child during feeding;
- Swelling of soft tissues;
- Shortness of breath with risk of pulmonary edema;
- Delayed physical development from the first months of life.
An unfavorable sign of impaired venous outflow is hydrocephalic syndrome, which indicates compression from outside by dilated vessels of the brain aqueduct carrying cerebrospinal fluid from the lateral ventricles and subarachnoid spaces, or a strong discharge of large amounts of blood into the veins of the skull.
Hydrocephalus is manifested by an increase in the size of the child’s head, expansion of its superficial veins, which is noticeable to the naked eye. Against the background of hydrocephalic-hypertensive syndrome, vomiting, convulsions, bulging eyes, strabismus, and focal neurological disorders are possible.
As a result of blood shunting, the hemispheres do not receive enough arterial nutrition, therefore the development of intelligence is disrupted and mental retardation is formed. In rare cases, hemorrhages into the brain with convulsions, coma, and paralysis are possible.
Malformation of the vein of Galen manifests itself in early childhood and is extremely rare in adults. Most often it occurs with hydrocephalus and intracranial hypertension due to compression of the cerebral aqueduct, as well as intracerebral hematomas, convulsive syndrome, mental and motor development disorders, and focal neurological disorders.
Due to the increased load on the myocardium, as well as due to concomitant malformations of the cardiovascular system, heart failure with shortness of breath, edema, and cyanosis appears quite early.
Depending on the severity of the course, several clinical types of malformation are distinguished:
- Type I - severe course with high mortality, cardiac and respiratory failure, enlarged liver, dropsy of the brain;
- Type II - severe neurological focal disorders, hypoplasia of parts of the brain, signs of arterial blood flow disturbance due to blood shunting;
- Type III - disorders of venous outflow with increased pressure, pathology of liquorodynamics, communicating hydrocephalus.
Arteriovenous malformations of the vein of Galen (AVMvG) are a special type of arteriovenous malformations (AVMs), characteristic mainly of pediatric patients. AVMvH account for approximately 30% of AVMs detected in childhood. The pathology is congenital and is characterized by the formation of an arteriovenous shunt in the area of one of the main venous collectors - the great cerebral vein (vein of Galen) [3-5, 7, 9, 11].
The main clinical manifestations of AVMvH are: 1) hypertensive-hydrocephalic syndrome, which develops as a result of occlusion of the cerebral aqueduct, impaired cerebrospinal fluid resorption; 2) focal neurological symptoms caused by secondary disorders of cerebral circulation of the ischemic type; 3) delayed psychomotor development of a child of a younger age group [5-7, 10, 12].
At the first stages of the development of vascular neurosurgery, treatment of AVMvH was palliative and limited to shunt operations for occlusive hydrocephalus, which did not solve the problem of the underlying disease. In cases of the natural course of the disease, i.e. without medical support, up to 90-96% of children died during the 1st year of life [14].
In connection with the modernization and fundamental changes in approaches to the treatment of AVMvH, the issue of early diagnosis of this pathology is of particular relevance. Currently, the standard for diagnosing AVMvH is ultrasound examination, which makes it possible to establish an accurate diagnosis already in the third trimester of pregnancy [1, 2, 15].
Attempts at open interventions for AVMvH, carried out before the era of endovascular surgery, were associated with high postoperative mortality, reaching 60%. Currently, this option of open interventions is performed only for thrombosed vein of Galen, which has a volumetric effect on the midbrain [8].
The question of the need, timing, and clear indications for performing CSF shunt operations as part of the complex treatment of this pathology remains debatable; This refers to the combination and sequence of endovascular and liquor shunt operations [16].
The small amount of data in the world and domestic literature and the inconsistency in approaches to complex treatment became the reason for conducting this study, the purpose of which is to develop an optimal algorithm for the diagnosis and treatment of patients with AVMvH.
Material and methods
The work is based on an analysis of the results of examination and treatment of 90 patients with AVMvH at the Research Institute of Neurosurgery named after. acad. N.N. Burdenko RAMS for the period from 1987 to 2009. Over the entire analyzed period, there was a gradual annual increase in the number of patients with AVMvH, mainly children of the younger age group, which is associated with improved early diagnosis and expanded opportunities for effective treatment of this pathology. The largest number of observations (38) occurred in the period from 2006 to 2009. Patients examined and operated on during this period constituted a prospective group.
The age of the patients ranged from 3 weeks to 38 years. All patients (27 (30%) female and 63 (70%) male) were divided into four age groups: group 1 (≤1 year) - 35 (39%), group 2 (1- 3 years old) - 15 (17%), 3rd group (3-10 years old) - 19 (21%), 4th group (over 10 years old) - 21 (23%), including 11 aged up to 16 years old, 10 - adults. The average age of patients under 16 years was 3.5 years, for adults - 22.9 years.
The examination of patients included the collection of anamnesis and general clinical data (term and method of diagnosis, the presence of hydrocephalus, delayed psychomotor and speech development, epileptic seizures, a history of hemorrhages, cerebral symptoms), indicators of physical development (weight, height, head circumference), ophthalmological, otoneurological , cardiac examination (echocardiography), CT and MRI of the brain at the pre- and postoperative stages. Angiographic examination (AG) was performed in all 90 patients; in most cases, 75 (83.3%) were performed directly during endovascular surgery. The division of AVMvH into angioarchitectonic types - mural and choroidal - was carried out according to total selective cerebral angiography in accordance with the classification of P. Lasjaunias et al. [10].
Anesthesia for all operations in patients of younger age groups (younger than 10 years) was carried out under endotracheal anesthesia and constant monitoring of ECG, blood pressure, partial pressure of CO2 and respiratory rate. In patients older than 10 years, intravenous sedation or neuroleptanalgesia was most often used.
Of the 90 patients, 78 (86.7%) used various treatment options for AVMvH. In 12 (13.3%) patients, the tactics of dynamic observation were chosen. In this group, 3 patients underwent only cerebrospinal fluid shunt surgery.
Endovascular treatment was performed in 75 (94.9%) patients out of 78 operated on. They performed a total of 131 endovascular operations. In the vast majority of cases - 129 (98.5%) - operations were performed using transarterial access; in a few cases - 3 (2.3%) transvenous access was used. The tactics of endovascular treatment depended on the type of AVM, the caliber of afferents and the age of the patient.
Microsurgical treatment of AVMvH was performed in 4 (5%) patients. The purpose of direct surgical interventions was the excision of the thrombosed ampulla of the vein of Galen after endovascular occlusion or after spontaneous thrombosis of the dilated vein of Galen, which had a local volumetric effect on the adjacent brain structures, in combination with occlusive hydrocephalus.
Radiosurgical treatment was performed in 8 (10.1%) patients.
CSF shunt operations were performed in 24 (26.7%) patients. In 20 patients, ventriculoperitoneostomy was performed, in 4 cases endoscopic perforation of the floor of the third ventricle was performed. In 3 cases, endoscopic ventriculostomy of the third ventricle and ventriculoperitoneostomy were performed sequentially.
The natural history group included 12 (13.3%) patients. In 9 cases there was a functioning AVMvH; in 3 (3.3%) patients, according to hypertension, spontaneous thrombosis of the AVMvH was detected.
The dynamics of the disease picture was assessed on the basis of clinical and radiological examination of patients in the immediate postoperative period, as well as 3 and 6 months after endovascular surgery, depending on the age, dynamics of psycho-speech and motor development of the child in a prospective group of patients. In the retrospective group, the analysis was carried out using records of control examinations of patients in the clinic of the Institute of Neurosurgery.
Clinical picture and angioarchitecture
The primary diagnosis of AVMvH was established on the basis of fetal ultrasound in utero in 22 (22.2%) patients, in newborns - according to neurosonography - in 16 (17.8%), CT - in 23 (25.5%), MRI - in 30 (33.3%), hypertension - in 1 (1.1%).
The leading clinical picture in children of all age groups with AVMvH was hydrocephalic syndrome; in the group of children aged 1 to 3 years, it was detected in 80% of cases. Hydrocephalus was the result of hyporesorption of cerebrospinal fluid due to impaired venous circulation, or was of an occlusive nature due to compression of the cerebral aqueduct by the dilated ampulla of the vein of Galen. An increase in head circumference occurred mainly in patients of the younger age group - up to 3 years (60%). Among patients over 10 years of age (47%) who were diagnosed with hydrocephalus, according to CT data, craniomegaly was found in 4% of patients. In group 1, hydrocephalus was detected in 59% of children under 6 months of age, and in 75% of children aged 6 months to 1 year (Table 1).
Other symptoms were less common: symptomatic epilepsy - in 19 (21.1%), dysfunction of cranial nerves (II, III, VI, VII) - in 19 (21.1%) and intracerebral hemorrhages - in 8.9% . Congenital heart defects were observed in 34.4% of patients, of which 3 underwent surgical treatment for this pathology.
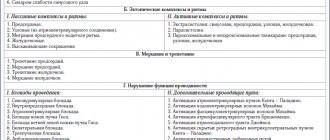
According to angiography, AVMvH of the choroidal type was detected in 67 (74.4%) patients, the mural type of AVM was verified in 20 (22.2%) patients (Fig. 1, a, b).
Figure 1. Angiogram of patients with AVMvH. a — choroidal type; b - mural type.
In 3 (3.3%) patients, spontaneous thrombosis occurred at the time of AG.
The afferents of AVMvH were most often the arteries of the vertebrobasilar system, less often - the arteries of the carotid system. In most cases, adjacent blood supply was detected (Table 2).
Results and its discussion
Results of endovascular treatment
The main goal of endovascular intervention was to stop or reduce the discharge of arterial blood into the cerebral venous system, which was achieved mainly through occlusion of afferent vessels using transarterial access. Only 3 patients had occlusion of the great cerebral vein due to the complete failure of transarterial embolization for the choroidal type of AVM. To occlude the afferents of AVMs of the mural type, microcoils and balloon catheters were used; for the choroidal type, microcoils, adhesive compositions, or a combination thereof were used.
Microspirals were used as occluding materials in 45 (60%) cases, detachable balloon catheters were used in 21 (28%) patients, adhesive compositions were used in 19 (24.9%) cases, including ONYX composition in 2 cases ( MTI, EV3, USA). In some observations - 10 (13.3%) a combination of different occlusive materials was used.
According to control cerebral hypertension, complete cessation of arterial inflow was achieved in the mural type of AVMvH in 61% of cases, while in choroidal type malformations this figure did not exceed 7%.
Complications after endovascular operations were noted in 10 (16%) cases. Of these, clinically significant complications - persistent neurological deficit caused by ischemic cerebral circulatory disorders in the choroidal arteries - occurred in 6 (10.7%). In 3 patients, intraventricular hemorrhage developed, in 1, a retroperitoneal hematoma was detected after endovascular surgery.
Death in the early period after endovascular surgery occurred in 2 (2.7%) cases. In one case, the cause of death was massive intraventricular hemorrhage, in the second - acutely developed occlusion at the level of the Sylvian aqueduct. Despite urgent external drainage of the lateral ventricles, the child died from axial herniation of the brain stem.
When assessing the dynamics of clinical symptoms 3 and 6 months after endovascular treatment, approximately the same results were obtained in all age groups; in the vast majority of observations, a positive result was noted (Fig. 2).
Figure 2. Dynamics of the clinical picture in different age groups 1 year after endovascular treatment.
In the long-term period (follow-up from 1 to 15 years) after endovascular treatment, improvement occurred in all age groups, the best result (82.8%) was observed in the group of patients under 1 year (Fig. 3).
Figure 3. Disease outcome in different age groups after endovascular treatment.
The “recovery” group included patients who had no clinical symptoms of the disease, and neuroimaging data did not reveal signs of functioning AVMvH and hydrocephalus (Fig. 4).
Figure 4. AVMvH of mural type. Endovascular occlusion of afferents by microspirals. Patient M. 4 months of age. a — MRI before surgery; b — initial hypertension of the vertebral artery; c — MRI 1 year after surgery; d — control hypertension of the vertebral artery. A comparative analysis of the outcome of the disease in different age groups found that improvement occurred in all age groups. The rate of recovered patients is significantly higher in groups 1-2 compared to groups 2-3. These trends reflect the degree of influence of endovascular operations on the clinical course of the disease. Thus, even a partial decrease in the degree of arteriovenous discharge creates conditions for improving cerebral hemodynamics, as a result of which the clinical status of patients improves (Fig. 5).
Figure 5. Choroidal type AVMvH. Occlusion of AVMvH afferents with microspirals (2 stages). Patient G. 3 months of life. a — MRI before surgery; b — initial hypertension of the vertebral artery; c — MRI 2 years after the 2nd stage of the operation; d — control hypertension of the vertebral artery. Total switching off of the pathological arteriovenous shunt (more often with mural-type AVMvH or with continued thrombosis after embolization of choroidal-type malformations) creates conditions for complete normalization of cerebral blood flow and leads to recovery of patients. Moreover, the earlier the endovascular operation is performed, the more obvious the overall positive effect. In addition, it is technically easier to perform endovascular interventions at an earlier age, when there is still no pronounced hypertrophy of afferent vessels and the volume of arteriovenous shunting is relatively low.
The probability of an increase in neurological symptoms is greatest in group 2 - 23.1%, and in the group of patients under 1 year of age the negative result was minimal - 3.2%.
The overall mortality rate among all 90 patients with AVMvH was 6.7%. In the early period after endovascular surgery, 2 (2.7%) patients died. In the long-term period, after partial occlusion of the afferents of the malformation, 2 (2.7%) patients died. Among patients who did not receive any treatment for AVMvH, 2 (16.7%) patients died from intraventricular hemorrhage.
Results of microsurgical and radiosurgical treatment
Microsurgical total excision of the thrombosed vein of Galen was performed in 4 patients. 3 of them experienced disability with the development of severe pyramidal symptoms.
Radiosurgical treatment was performed in 8 patients over 5 years of age with choroidal AVMvH. In 7 (87.5%) cases, radiation therapy was preceded by endovascular partial occlusion of accessible AVM afferents. When analyzing the long-term results of radiosurgical treatment, stabilization in the clinical and radiological picture of the disease was revealed in the majority of patients. In 2 patients, an increase in symptoms in the neurological status was noted. In 7 cases, according to control CT and MRI data, performed at different times after irradiation, the x-ray picture remained unchanged. Only in 1 observation during control hypertension was complete thrombosis of the AVM detected. However, this patient, a year after proton irradiation, developed symptoms of damage to subcortical structures, hemiparesis, paresis of the third nerve on the left, and emotional and personal disorders caused by the development of radiation necrosis.
Results in the natural history group
The natural course of the disease group included patients with spontaneous thrombosis of AVMvH, patients who at the time of treatment did not have the technical capabilities to perform endovascular surgery, as well as patients who refused surgical intervention, a total of 12 (13.3%) observations. When assessing the neurological status after 1 year of observation, stabilization of the clinical symptoms of the disease was noted in 8 (66.7%) cases. In 4 (33.3%) there was an improvement in neurological status. It should be noted that in 3 of these 4 patients spontaneous thrombosis of AVMvH was detected according to hypertension.
When analyzing the frequency of cases of stabilization and improvement in the groups of endovascular treatment and the natural course after 1 year, a statistically significant (p < 0.05) increase in positive results was shown in the group of patients who underwent endovascular treatment.
Evaluation of long-term results in the group with the natural course of the disease revealed a high mortality rate - 16.7% (2 observations) - in comparison with the endovascular treatment group (5.3%). Recovery occurred only in 3 patients with spontaneously thrombosed malformation; in the remaining 5 (41.7%) cases, the clinical status remained relatively stable.
Results of treatment of AVMvH against the background of liquor shunt operations
CSF shunt operations were performed in 24 patients. In 9 cases, shunt surgery was performed before endovascular treatment, in 13 patients - after partial occlusion of AVMvH, in 2 cases - with spontaneously thrombosed malformation. In no case was there any intracranial hemorrhage during CSF shunt surgery.
Complications after bypass operations developed in 9 (37.5%) patients. They were not specific in nature and were associated with inflammatory changes, as well as hyperdrainage syndrome and the development of subdural accumulations of cerebrospinal fluid.
Thus, AVMvH has a complex angioarchitecture, which is largely individual for each patient. There is no doubt that it is on the basis of a thorough study of angioarchitecture that adequate planning of all stages of surgical treatment of patients with AVMvH is possible.
Summarizing the results of our work, it should be noted that the most effective method of treating AVMvH is the endovascular method. The high percentage of satisfactory results obtained indicates the correct selection of optimal types of treatment depending on the anatomical type of AVMvH and the age of the patient.
A wait-and-see approach for asymptomatic AVMvH is unjustified, since successful endovascular treatment in the first year of life, before the onset of irreversible neurological disorders, allows one to achieve good clinical results. The natural history of AVMvH is associated with a higher risk of intracranial hemorrhage.
With mural-type AVMvH, endovascular treatment can achieve complete recovery of the patient, while with choroidal-type AVMvH, by occlusion of the largest afferents, stabilization of the clinical manifestations of the disease can be achieved by improving cerebral circulation.
Radiation therapy for AVMvH with large afferents and high shunting rates is ineffective. Indications for radiosurgical treatment can be determined in patients with AVMvH of the choroidal type with numerous small-caliber afferents and a relatively low volume of arteriovenous discharge, as well as after partial embolization upon achieving maximum blood flow reduction.
The assumption existing in some literature sources [1, 13] that CSF shunt operations against the background of a functioning AVMvH are associated with a high risk of hemorrhagic complications was not confirmed in our observations. For progressive occlusive hydrocephalus, the method of choice is endoscopic ventriculostomy, for aresorptive hydrocephalus - ventriculoperitoneal shunting.
conclusions
1. Prenatal diagnosis of AVMvH using ultrasonography and fetal MRI makes it possible to establish a diagnosis already in the third trimester of pregnancy, which allows adequate planning of delivery and further treatment of the child.
2. The endovascular method is a highly effective and low-traumatic method of treating AVMvH with a low level of disability and mortality. Microsurgical excision of AVMvH is associated with a high risk of complications and disability for the patient.
3. The optimal age for treatment is 4-5 months. Heart failure is not an absolute contraindication for endovascular surgery, except for decompensated heart failure requiring surgical treatment.
4. The presence of progressive hydrocephalus with corresponding symptoms is an indication for CSF shunt surgery before endovascular treatment.
Review
Treatment of patients with arteriovenous malformations of the vein of Galen (AVMvG) continues to be one of the important problems of modern neurosurgery. Due to its relatively rare occurrence, there is no uniform standard for the treatment of this pathology.
The article provides convincing data in favor of the endovascular method of treating this pathology, based on retrospective and prospective analysis of a large number of patients, even according to global data. At the same time, the authors prove the low effectiveness of radiation therapy and justify performing CSF shunt operations for progressive occlusive and aresorptive hydrocephalus.
The work shows that endovascular treatment of AVMvH in the first year of life makes it possible to achieve complete recovery in a large number of patients, so wait-and-see tactics for this pathology are unjustified.
Undoubtedly, the presented article contains novelty and certain value in solving the problem of treating AVMvH and will be useful for both scientific and practical neurosurgeons.
V.E. Ryabukhin
(Moscow)
Nuances of diagnosing venous malformations
Diagnosis of pathology of intracranial veins is carried out through:
- X-ray contrast angiography - after the birth of a baby, this is the main research method that plays a decisive role in determining surgical tactics;
- Ultrasound analysis with Doppler measurements - before birth in the third trimester and after the birth of the baby (neurosonography) is the safest and most accessible diagnostic method;
- CT, MRI - in the early neonatal period.
Detection of an aneurysm of the vein of Galen becomes possible no earlier than the third trimester of gestation using ultrasound. The anomaly appears as an anechoic formation in the center of the skull. Ultrasound scanning is complemented by Doppler measurements to determine the nature of blood flow in pathologically altered vessels.
If a woman was not examined before childbirth, then it is extremely difficult to suspect a pathology both because of its rare occurrence and due to the absence in some cases of clinical signs at the time of birth of the child. Pediatricians make the diagnosis by excluding other causes of cerebral edema and heart failure.
In addition to ultrasound diagnostics, computed tomography and MRI are used, which show tangles of abnormally developed intracranial vessels. X-ray contrast angiography makes it possible to clarify the nature of the branching of embryonic vessels, their relationship with normal ones, the presence or absence of thrombosis, based on the results of which a surgical treatment plan is also developed.