- ECG principle
- ECG registration in 3 standard leads
- Registration of ECG in 12 leads
- What does an ECG show?
- Normal ECG
- Pathologies in ECG
- Arrhythmia
- Atrial hypertrophy
- Blockade
- Ischemic disease
- Pericarditis
- Myocarditis
- Thromboembolism
- Hypokalemia
- Tachycardia
- Myocardial infarction
- How is ECG diagnosed?
- ECG methods
- ECG interpretation
- When to do an ECG
- Cost of ECG in our clinic
Electrocardiography is a method of recording and studying the electric fields that appear during the heart's work. These electrical fields give an accurate picture of how the cardiovascular system functions. ECG is an inexpensive and effective diagnostic method in cardiology.
ECG principle
The operation of the ECG device is that sensors placed on the patient’s body record the vector and strength of the electrical charge that the heart creates during operation. Changes in the electric charge vector are recorded on paper tape in the form of a graph. Analysis of this graph allows us to draw a conclusion about the correct functioning of the heart and possible diseases.
Electrocardiogram registration is carried out in:
- three standard leads;
- in 12 leads.
ECG registration in 3 standard leads
Registration of an electrocardiogram in 3 standard leads is called a single-channel ECG. It allows you to get a general picture of the condition of the heart and is used during a cardiac examination of the patient in the absence of specific complaints.
The potential difference is determined between:
- left hand and right hand - this is an indicator of the work of the anterior wall of the heart;
- between the left leg and right arm - this is the total reflection of leads 1 and 3;
- between the left leg and left arm - this is an indicator of the work of the posterior wall of the heart.
These leads form an equilateral Einthoven triangle, the vertices of which are located on the electrodes placed on the limbs. In the middle of the triangle is the electrical center of the heart. The electrode on the right is not used for leads, but is intended for grounding.
The line connecting two electrodes of the same lead is called the lead axis. When the vector of the electrical charge of the heart is in the negative part of the lead axis, then a negative deviation is recorded - Q, S waves; if the vector is in the positive part of the lead axis, then a positive deviation is recorded - P, R, T waves.
Registration of ECG in 12 leads
Registration of a 12-lead electrocardiogram is used for specific patient complaints to obtain additional information about the functioning of the cardiovascular system, minor changes, identify the focus of ischemia or necrosis, and the causes of conduction and rhythm disturbances.
In addition to the 3 standard leads, the potential difference is determined between:
- between the left leg and joint hands (aVF) - this is an indicator of the work of the posterior-inferior heart wall;
- between the left arm and the combined left leg and right arm (aVL) - this is an indicator of the work of the left anterolateral wall;
- between the right arm and the combined left leg and left arm (aVR) is a measure of right lateral wall function.
In addition, six unipolar chest leads are used, when 6 electrodes are installed directly on the chest:
- V1 and V2 are an indicator of the work of the right ventricle;
- VЗ is an indicator of the functioning of the interventricular septum;
- V4 is an indicator of the performance of the apex;
- V5 is an indicator of the work of the left ventricle and the anterolateral wall;
- V6 is an indicator of the work of the lateral wall of the left ventricle.
Registration of data from unipolar chest leads allows one to judge the position of the heart in the chest, the size of the ventricles, determine hypertrophy of the right sections, assess the condition of the atria and identify various pathologies.
Registration of an ECG in 12 leads allows you to determine even small changes in the work of the heart that ECG registration in 3 standard leads will not show.
Indications for ECG
ECG is performed:
- for any diseases of the cardiovascular system;
- if you suspect such diseases, for example, chest pain, shortness of breath, swelling of the legs;
- people who are at risk of developing heart disease (those with a hereditary predisposition, those suffering from obesity, atherosclerosis, bad habits - smoking, alcoholism) to determine the condition of the heart;
- in case of risk of complications from the heart, in particular with hypertension, after infectious diseases (for example, tonsillitis), after a stroke;
- when planning and managing pregnancy;
- to assess the effect of medications on the body (in particular, to confirm the absence of side effects when taking them);
- to check the operation of pacemakers.
What does an ECG show?
Electrocardiography shows:
- heart rate;
- heart rate;
- position of the electrical axis of the heart;
- size and location of the heart;
- heart condition.
If pathologies are present, electrocardiography can reveal:
- arrhythmia;
- blockade;
- myocardial infarction;
- ischemic changes;
- dystrophic processes;
- electrolyte disturbances;
- Wolff–Parkinson–White syndrome;
- ventricular hypertrophy;
- other pathological processes in the heart.
Electrocardiogram of a healthy person
Diseases of the cardiovascular system in developed countries rank first in mortality. It is worth noting that heart disease has become much younger in recent years. At a cardiologist's appointment you can meet both middle-aged and elderly people, as well as the younger generation. A number of heart diseases are practically asymptomatic. However, even when the first symptoms appear, we do not run to the doctor with our problem, but begin to self-medicate.
Important! You should not self-diagnose and take medications, experimenting with your health. The use of modern screening diagnostic methods for the state of the patient’s cardiovascular system helps the cardiologist make a diagnosis. Electrocardiography is one of the simplest, fastest and most effective methods for assessing the state of the human cardiovascular system.
Before taking an electrocardiogram (ECG), the readiness of the device for operation is checked (calibration is carried out). The electrodes are applied in a certain way to the patient’s limbs; for convenience, they are marked in different colors. The signal from the electrodes is converted into an electrocardiogram and displayed on the monitor screen.
Rules for conducting an ECG
Once every 3-6 months, it is recommended to undergo an ECG procedure for healthy people who do not have heart problems. People with various pathologies, in particular cardiovascular diseases, should have an ECG taken at least once a month, since the ECG result is valid only during this period of time. It is worth noting that the procedure for taking an ECG is absolutely safe and painless for human health.
The first electrocardiograph was invented by the talented Dutch physiologist Willem Einthoven. The scientist worked on creating the device for seven whole years and on November 14, 1903, presented it to humanity. The device could record and measure electrical impulses that appeared during the contraction of the heart muscle. The weight of the device reached 270 kg; to take an electrocardiogram, the help of five people was required, and the patient had to immerse his arm and leg in a container with liquid. Despite this, this invention made a revolutionary breakthrough in medicine.
Today, the ECG machine is a compact and portable device. This device has become widespread and is used in almost every medical institution: ambulances and intensive care units, clinics and 24-hour hospitals. To carry out the ECG procedure, it is recommended to follow the following rules:
- DO NOT eat large amounts of food
- No smoking,
- DO NOT use medications.
The patient needs to undress to the waist and take a horizontal position. Before applying the electrodes, it is necessary to treat them with a special conductive gel for best contact with the skin.
Important! To correctly interpret the ECG, you must make an appointment with a cardiologist.
Decoding indicators
The heart, like a precise clockwork mechanism, works according to certain principles. It is characterized by:
- automaticity (the impulse contracts voluntarily (spontaneously), exciting the heart);
- excitability (an exciting impulse activates the heart);
- conductivity (the organ conducts impulses from the place of their origin to the myocardium);
- tonicity (the ability to maintain the shape of the heart during diastole);
- contractility (the ability to contract under the influence of impulses);
- aberration (pathological impulse conduction);
- refractoriness (lack of excitation of myocardial cells when additional impulses appear).
Based on the results of the ECG, you can understand the overall picture of the patient’s heart condition. At rest, the heart muscle is electrically neutral. Under the influence of an exciting impulse, a biopotential (potential difference) is formed. In electrocardiography, the potential differences we measure are called leads.
How to correctly read the encrypted message from our heart? A typical human ECG consists of five positive and negative oscillations - waves corresponding to the cycle of cardiac activity. These teeth are formed by changing the amplitude and height of the signal. Knowing the correct interpretation of these indicators, we can draw a conclusion about the functioning of the cardiovascular system.
ECG waves
ECG waves are usually designated by Latin letters - P, Q, R, S, T. The shape and size of these teeth differ in different electrocardiographic leads. On any ECG, several waves, segments and intervals are distinguished, reflecting the complex process of propagation of an excitation wave throughout the heart. The figure below shows an example of a normal human ECG:
Figure 1. Diagram of a normal human ECG
The values of the main teeth presented on the cardiogram:
- P wave . The atrial complex reflects the process of depolarization of the right and left atria. The amplitude of P is 0.5–2.5 mm, the duration does not exceed 0.1 seconds.
- Q wave . Reflects excitation of the interventricular septum (not necessarily with a negative amplitude). The Q amplitude is normally no more than 2 mm (or 25% R), the Q duration does not exceed 0.03 seconds.
- R wave . Caused by ventricular depolarization.
- S wave . Reflects excitation in the basal layer of the ventricles of the heart. Optional negative prong. The amplitude S varies widely, but not more than 20 mm.
- T wave . Reflects the process of ventricular repolarization. The duration is not 0.1–0.25 seconds.
Thus, monitoring the electrocardiogram allows us to characterize the work of the heart. If there are various abnormalities in the functioning of the heart, they are displayed on the electrocardiogram by the absence of waves or their presence not characteristic of a given lead, changes in the duration of intervals, the polarity and amplitude of the waves.
Assessment of heart condition using an electrocardiogram
Only a qualified specialist can correctly interpret the result of an electrocardiogram. Having carefully studied the ECG and calculated the intervals between the waves, the doctor is able to give an objective assessment of the functioning of the cardiovascular system. An electrocardiogram with sinus rhythm is normal for a healthy person.
The following key aspects should be taken into account when decoding the cardiogram:
- Heart rate (normally does not exceed 70 beats per minute), general heart rhythm.
- Calculation of intervals between teeth. The interval values make it possible to identify: myocardial rheumatism, coronary heart disease, atherosclerosis, myocarditis. It is worth noting that with severe pathology, altered intervals are immediately visible.
- Electrical axis of the heart (EOS) is a projection of the resulting vector of excitation of the ventricles in the frontal plane. It is measured in degrees, calculated from isolines based on the amplitude of the tooth.
- The QRS complex reflects the process of ventricular depolarization and is measured in the second standard lead from the beginning of Q to the end of R (Figure 1). The normal duration is 0.05 - 0.1 second.
- The ST segment corresponds to the period when both ventricles are completely covered by excitation, measured from the end of S to the beginning of T. The duration of ST depends on the pulse rate. Normally, the ST segment is located on an isoline, ST depression is allowed up to 0.5 mm, elevation in standard leads should not exceed 1 mm. The doctor draws conclusions about the chaotic depolarization and repolarization of the heart.
- Age, gender and emotional state of the patient. Elderly people experience a slow heartbeat, and pregnant women experience a rapid heartbeat.
Modern ECG devices have an expanded range of functions with the ability to automatically decipher the cardiogram, accurately recording changes in the potential difference. In addition, they can display the main indicators and even make a diagnosis. However, you should not completely trust such devices, and it is better to entrust the final diagnosis to a doctor - a cardiologist.
An electrocardiogram is an objective graphical display of the condition of the heart. A simple, fast and non-invasive diagnostic method has no contraindications. The ECG procedure will not take you much time, but will allow you to identify diseases of the cardiovascular system.
Normal ECG
A normal electrocardiogram consistently displays:
- zero line;
- small P wave - normally lasting 0.7 - 0.12 seconds and amplitude 0.5 - 2.5 mm;
- small flat segment PQ;
- negative Q wave (may be absent) - normally lasting 0.03 seconds and amplitude 0.3 - 0.5 mm;
- a high positive R wave, normally with an amplitude of 10-19 mm, and a negative S wave, with a normal amplitude of 0.2-0.5 mm;
- flat ST segment;
- rounded positive T wave - normally lasting 0.12-0.28 seconds and with an amplitude of no more than a quarter of the R wave;
- very low rounded positive U wave.
The norm of intervals is:
- PQ - duration 0.2 - 0.8 seconds;
- PR - duration 0.18 - 0.2 seconds;
- QRST - duration 0.38 - 0.55 seconds;
- QRS - duration 0.06 - 0.1 seconds;
- ST - duration 0.35 - 0.44 seconds.
Heart rate
calculated as:
Heart rate = 60/(distance between teeth R * K). K is a coefficient depending on the speed at which the electrocardiogram is taken: at a speed of 25 mm/s the coefficient is 0.04, and at 50 mm/s the coefficient is 0.08.
The norm is 50-90 beats per minute.
For example, if the distance R was 20 mm, and the cardiogram was taken at a speed of 25 mm/s:
Heart rate = 60/(20*0.04) = 75 beats per minute (normal).
Heartbeat
assessed by the degree of rhythm of the cardiogram. Normally, it should be repeatable with possible deviations of up to 10%. To evaluate deviations, the distance between the RR teeth is compared.
In this case, the heart rhythm normally has a sinus nature, as indicated by the P wave, which is positive in leads 1 and 2 and negative in lead aVR.
Basically, such indicators indicate that the heart is healthy. But it is worth remembering that the ECG decoding must be done by a doctor; only he can make the correct diagnosis, so you should not decipher the electrocardiogram yourself.
Further study of the ECG
Once you have mastered the basics of the ECG and have learned to confidently look at the electrocardiogram, knowing what you should analyze on it and how to interpret the main changes you find, you need 2 things - first of all, practice, as well as in-depth study of individual ECG topics.
ECG practice
The main thing you need to understand about ECG practice is that it must be regular. ECG analysis and interpretation is a skill that needs to be practiced. It may be difficult at first and there will be many small questions about various details. This is normal, the main thing is to try to sort out unclear questions and look into books and reference books on ECG more often.
After some time of viewing ECGs, you will feel something like a “point of no return”, when you will be able to look at the ECG comprehensively, confidently excluding or confirming the main pathologies. However, there will still be complex, controversial cases that will force you to read more in-depth books and articles on ECG and ask your colleagues for advice.
Where can I find an ECG for regular practice?
There are various sources: atlases, public pages, websites, videos, programs for smartphones.
Subscribe to VKontakte public pages:
- MEDIC: ECG. In this group, every day in the morning an ECG is posted with possible answers in the form of a test, and in the evening an answer is given with an analysis of the main changes in the ECG. You can also find various sources and articles on ECG here. Link: https://vk.com/medic_ecg
- ECG tests. Another great public page with ECG tests every day. Its admin also translated many different books on ECG from English, created several reference programs on ECG for computers and phones, all of this can be found in the group. Link: https://vk.com/club122935445
Websites:
1. https://lifeinthefastlane.com/ecg-library/ - This site has many different ECG examples. It is also one of the best sites that can be used as a reference when you don't understand something, and even to some extent as a study guide.
2. Wikipedia on ECG: https://en.ecgpedia.org/index.php?title=Main_Page
3. https://www.ecg-quiz.com/
4. https://www.skillstat.com/tools/ecg-simulator - online ECG simulator (see picture) Try your hand at determining the rhythm on the monitor at speed! You can also download the ECG simulator to your computer: https://cloud.mail.ru/public/6aLN/9xaABKDea
Even more useful public pages and websites on ECG can be found in this article on “MEDIC: ECG” - https://vk.com/@medic_ecg-ssylki-na-resursy-po-ekg
Pathologies in ECG
An electrocardiogram different from normal may indicate various diseases and disorders of the heart.
Diseases may include:
- arrhythmia;
- atrial hypertrophy;
- blockade;
- ischemic disease;
- pericarditis;
- myocarditis;
- thromboembolism;
- hypokalemia;
- tachycardia;
- heart rhythm disturbances;
- myocardial infarction.
Arrhythmia
Arrhythmia is characterized by the fact that among the normal contractions of the heart there are also contractions with deviations from the norm, the heart beats less often or more often than necessary, the size of the cardiogram teeth is not the same in each heartbeat.
Such ECG features may indicate arrhythmia.
Arrhythmia can be dangerous and lead to thromboembolism, heart failure and even cardiac arrest in the absence of timely treatment and assistance.
Atrial hypertrophy
With left atrial hypertrophy on the ECG, the P wave in leads 1 and 2 is double-humped, and in V1 it is negative and long.
Atrial myocardial hypertrophy is an increase in the thickness of the myocardial wall of the heart, in conditions of chronic overload of the heart with volume and pressure. Hypertrophy can lead to cardiac arrhythmia.
Blockade
With bundle branch block, the ECG shows a widening of the QRS interval, and with complete blockade, the ST segment and T wave become negative.
Blockade is a slowdown in the conduction of an electrical signal through the conduction system of the heart. Causes heart rate to slow to less than 50 beats per minute.
Ischemic disease
With coronary heart disease on the ECG, the ST segment is slightly lowered, and the T wave has a shallow negative value.
Coronary artery disease is stenosis of the coronary arteries resulting from atherosclerosis. As a result of arterial blockage, myocardial infarction may develop.
Pericarditis
With pericarditis, the ECG shows a slight rise in the ST segment from the ascending knee of the S wave, concave downward, and the T wave is positive. In chronic pericarditis, the ST segment is not elevated, and the T wave is negative and sharp.
Pericarditis is an inflammatory lesion of the serous membrane of the heart, manifested in the appearance of fluid in the area of the pericardium and fibrosis, which leads to difficulty in the functioning of the heart.
With timely diagnosis and treatment, the patient makes a full recovery.
Myocarditis
With myocarditis, the ECG often shows depression of the ST segment and a negative T wave. But not always, there are other ECG features that indicate myocarditis, such as a change in the duration of the PQ interval, signs indicating blockade of the left or right leg of the PG and heart rhythm disturbances .
Myocarditis is damage to the muscular lining of the heart as a result of inflammatory processes. Leads to heart failure, shortness of breath, cardiac arrhythmias, discomfort, pain in the heart area and other symptoms.
If myocarditis is detected, hospitalization and treatment are required.
Thromboembolism
With thromboembolism of the pulmonary arteries on the ECG, the RS-T segment is shifted upward and a negative T wave is observed in leads V1-V4.
Thromboembolism is a blockage of a vessel by a blood clot and disruption of blood flow.
If thromboembolism is detected, urgent hospitalization and treatment are necessary.
Hypokalemia
With hypokalemia, the ECG shows a large U wave in the initial form of the disease, and in severe forms, ST segment depression and a deep negative T wave.
Hypokalemia is a reduced concentration of potassium ions in the blood. May cause fatigue, weakness, breathing problems, intestinal obstruction and other disorders.
Treatment is aimed at replenishing potassium levels in the body.
Tachycardia
Tachycardia is characterized by an increase in heart rate above 90 beats per minute at rest. With tachycardia, an increased QRS segment may be observed on the ECG.
Tachycardia is a symptom that indicates the presence of a number of diseases, most often the endocrine and nervous systems.
When tachycardia is detected, further diagnostics are required to identify the cause and eliminate it.
Myocardial infarction
With myocardial infarction, the ECG in one case may show both the absence of ST segment elevation and the Q wave, as well as ST segment elevation and deformation, a large Q wave and a pointed negative T wave.
Myocardial infarction is an acute, life-threatening disease that requires rapid hospitalization and surgical treatment.
Myocardial infarction occurs due to thrombosis of the coronary artery, resulting in blockage of the artery, partial or complete cessation of blood supply and the beginning of the process of tissue death.
Information content and diagnostic capabilities of ECG
An ECG can reveal:
- heart rhythm disturbances (diagnosis of various types of tachycardia, as well as atrial fibrillation, parasystole and other types of heart rhythm disturbances);
- cardiac conduction disorders. This leads to a shift in the generation of impulses from the sinus node, as well as to its blockade in any part of the heart;
- decrease in coronary circulation in one or another part of the heart (coronary heart disease);
- focal changes in the heart (scar tissue formed after inflammatory diseases, myocardial infarction and other diseases);
- myocardial hypertrophy (thickening of the myocardial walls).
How is ECG diagnosed?
The electrocardiography procedure is painless and quick:
- A patient enters the ECG diagnostic room.
- He takes off his clothes to the waist and rolls up his pants, exposing the shins of his legs.
- The doctor lubricates the sensors with gel and attaches them to the patient’s body, fixing them.
- The doctor asks the patient to take the desired body position on the couch, standing or on a bicycle ergometer.
- The diagnostician turns on the ECG machine and begins recording a diagram.
- The doctor removes the sensors from the patient’s body, asks to wipe the body with gel wipes and gets dressed.
- The doctor analyzes the electrocardiogram, makes a diagnosis, gives recommendations and further instructions.
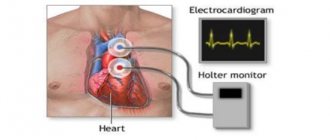
With 24-hour Holter monitoring, the doctor places sensors on the patient's body that are connected to a small portable device that collects electrocardiographic data continuously throughout the day. The sensors and ECG device are hidden under clothing and the patient wears them for 24 hours. Then he returns to the doctor, removes the device and sensors. The doctor analyzes the ECG, draws conclusions and makes a diagnosis for the patient.
Stages of the ECG procedure
Electrocardiography is a research method in which the electrical fields of the heart are recorded, provoked by contractions of the heart muscle. As a result, the specialist receives a cardiogram - an image of curve graphs. They can be displayed on a monitor or recorded on a special paper tape. To carry out this type of diagnosis, you need professional medical equipment - a cardiograph. This device consists of three required elements.
- An input device including electrodes, lead cables and their switches.
- Signal amplifier - allows you to amplify them to the value necessary for analysis.
- Recording unit for direct recording of a cardiogram.
When conducting an ECG, a specialist works sequentially with all these blocks, following a clear algorithm. It, in turn, is divided into several stages:
- preparing the room, equipment and patient for ECG;
- application of electrodes and connection of leads according to a specific scheme;
- adjusting the gain to correctly display the signal on the cardiogram;
- direct recording of the electrocardiogram.
For informative and reliable research results, it is necessary to avoid errors at each of these stages. Therefore, let’s take a closer look at their algorithms and features.
ECG methods
- Classic method
. Registration of an electrocardiogram in 3 standard and 12 leads. The electrodes are attached to the body of the patient, who lies on the couch. The cardiogram is taken at rest. - Vectorcardiography
. The electrical vector of the heart's work is recorded and displayed as a projection of a three-dimensional figure on the lead plane. - Load tests
. Registration of an ECG when the patient is on a bicycle ergometer with increasing stepwise physical activity. Most often used to diagnose coronary heart disease. - Holter monitoring
. Record electrocardiography continuously throughout the day using a special portable device. - Precordial mapping
. Electrodes with a 6x6 matrix are fixed on the patient’s chest, the signals from which are processed by a computer. Used to determine myocardial damage in acute myocardial infarction. - Intraesophageal electrocardiography
. The ECG is recorded using an electrode inserted into the patient's esophagus. Used to diagnose blockades and determine the condition of the atria and atrioventricular connection. - Gastrocardiomonitoring
. Simultaneous recording of gastrogram and electrocardiogram during the day. Used to diagnose gastro- and cardiac diseases. - High resolution electrocardiography
. Registration of low-amplitude and high-frequency potentials, with an amplitude of the order of 1-10 µV and using multi-bit ADCs (16-24 bits).
General rules for applying electrodes
When recording an electrocardiogram, electrodes are installed on several areas of the body. This ensures the conduction of electrical impulses through the heart, and the results are more accurate. The correct location of the terminals is the key to reliable recording of heart function.
General rules for installing electrodes:
- The skin at the site where the electrode is applied is degreased with alcohol;
- Pronounced hair when using reusable electrodes is treated with a soap solution (otherwise the hair is shaved off);
- The electrodes are coated with a special gel that improves electrical conductivity (it can be replaced with an isotonic solution, but this is not recommended, as the contact will worsen);
- The use of gauze pads instead of a special gel is also not an alternative to the gel, since they dry out quickly (such pads are absolutely prohibited for long-term studies, for example, Holter monitoring);
- It is important to follow safety rules when working with electrical devices, in particular grounding (not required when recording ECGs using portable battery-powered electrocardiographs).
All electrodes are divided into reusable and disposable. Each type has advantages and disadvantages and, as a rule, the option for recording is selected by medical personnel.
Features of disposable electrodes
You can purchase disposable electrodes in the Avicena-med online store, where only high-quality elements made in Italy are sold. They are suitable for daily monitoring or stress tests, which involve the patient’s physical activity.
Advantages of disposable electrodes:
- No risk of transmission of infectious diseases;
- Easy to install (doctors consider them more practical);
- High degree of adhesion (does not fall off after prolonged use);
- Good conductivity and high-quality contact;
- Suitable for patients with excessive sweating.
Unlike disposable electrodes, reusable designs are often used in government agencies, as they are more economical and durable.
ECG interpretation
The doctor deciphers the electrocardiogram; only he can identify diseases, make the correct diagnosis and give further directions. A person without medical education should not deal with ECG interpretation.
When deciphering an electrocardiogram, the diagnostician pays attention to the duration, amplitude, shape, frequency, repeatability and other parameters of the following elements of the cardiogram:
- P wave;
- PQ segment;
- Q wave;
- R wave;
- S wave;
- ST segment;
- T wave
Basic rules for electrode placement
To record an ECG, you need to install electrodes on special points on the body. This is the only way to correctly record the electrical impulses produced by the heart. It is the correct location of the terminal that ensures a clear recording of the cardiogram. Be sure to lubricate the ECG electrode with alcohol.
If the patient has a lot of body hair, then you need to treat the skin with a soap solution or shave the hair. For better electrical conductivity, you need to lubricate each electrode with gel. If you don’t have the gel at hand, you can take an isotonic solution or gauze pads. But if the study is long, then gauze pads cannot be used.
If stationary ECG devices are used, they must be grounded.
Electrodes are either single-use or reusable. The choice of electrodes depends on the preferences of the healthcare professional performing the ECG.
ecg how to do it correctly
When to do an ECG
Electrocardiography should be done in the following cases:
- Referrals from a general practitioner or other physician;
- For preventive purposes, once a year after 40 years;
- Pain in the chest or under the shoulder blade;
- Labored breathing;
- Swelling of the limbs and face;
- Shortness of breath at rest;
- High blood pressure;
- Chronic diseases of the musculoskeletal system.
When and who needs to undergo heart diagnostics?
The doctor prescribes this diagnostic test in the following cases:
- high blood pressure;
- chest pain, shortness of breath;
- dizziness or fainting;
- heart murmurs;
- heart rhythm is disturbed;
- rheumatism;
- diabetes.
An electrocardiogram is also prescribed in case of overdose of certain medications. An ECG is part of the examination during medical examination, prof. examination, pregnancy, preparation for operations.
This is not an exhaustive list of cases when an ECG is necessary. In addition, it is performed without a doctor’s referral.
Cost of ECG in our clinic
We provide the following services in the field of cardiology and ECG diagnostics:
- Primary appointment with a cardiologist - 1500 rubles;
- Repeated appointment with a cardiologist - 1400 rubles;
- ECG with interpretation - 500 rubles;
- ECG without interpretation - 250 rubles;
- Interpretation of an ECG done in another clinic - 300 rubles;
- Daily Holter ECG monitoring - 2200 rubles;
- Comprehensive daily monitoring of blood pressure + ECG according to Holter - 3500 rubles;
- Bicycle ergometry (stress tests) - 1800 rubles;
- “Healthy Heart” program - 6,500 rubles;
- Daily blood pressure monitoring - 1700 rubles;
- Tropanin test - 400 rubles.
You can make an appointment for an ECG with a doctor through the online form on the website or by phone 8
and
+7 (4872) 49-57-57
.
All articles "
Fixation of electrodes in chest leads
If a single-channel study is carried out, then only one electrode is used. But in modern ECGs, for more accurate diagnosis, in most cases, 6 are used. They are designated by the Latin letter V and are superimposed at the following points:
- V1 - at the right edge of the sternum in the 4th intercostal space, the red wire is connected;
- V2 - also in the 4th intercostal space, but on the left edge of the sternum, wire color - yellow;
- V3 - in the middle between the 4th and 5th intercostal spaces along the left line, connect the green cable;
- V4 - along the midclavicular line in the 5th intercostal space, wire color - brown;
- V5 - along the anterior axillary line in the 5th intercostal space, connected to a black cable;
- V6 - in the middle of the axillary line at the same level with V450m, the wire color is blue (possibly purple).
How to prepare for the procedure, how it is carried out, who does the decoding
Electrocardiography does not require special preparation. The patient can undergo examination at any time. Before visiting the functional diagnostics office, you need to take care of your appearance, since you will have to expose your chest, forearms and shins, to which the electrodes are attached.
Important! Before the examination, it is not recommended to overeat, smoke, worry, go to the gym or run, drink alcohol, coffee, or energy drinks.
Taking an ECG looks like this: the patient removes the necessary areas of the body from clothing and lies down on the couch. The doctor or nurse degreases the skin with a special product (or water) so that the “suction cups” have better contact with the body, applies electrodes, turns on the device and makes a recording. With the results obtained and a preliminary transcript, the patient is sent to the attending physician.