In recent decades, diagnostics of diseases of the upper digestive tract using flexible fiber optics - fibrogastroduodenoscopy (FGDS) - has been widely used in medical practice. Bleeding from the digestive organs as a result of a violation of the integrity of an arterial or venous vessel can occur with inflammatory, hereditary, tumor diseases of the stomach and duodenum. FGDS is effectively used to determine the location and stage of the pathological process, the intensity of blood loss, and the possibility of relapse of a life-threatening condition. To systematize the data obtained, a Forest classification was created.
Advantages of the method
The advantage of the FGDS method is the ability to carry it out almost anywhere - both in a specialized office and in a department ward.
Based on the results of the examination, having classified the bleeding according to Forest, the specialist can decide on the tactics of further treatment measures - either prescribe conservative methods of treatment, that is, using hemostatic drugs, or immediately refer the patient to the surgical department. The use of endoscopic methods also makes it possible to determine the volume of necessary surgical intervention - suturing a damaged vessel, excision of an ulcerated area of the mucosa, resection of the stomach. Under endoscopic control, it is possible to directly influence the damaged vessel wall - coagulation, clipping, fibrin filling, injecting the damaged area with hemostatic agents.
The procedure for fibrogastroduodenoscopy
Diagnostics
Forest's classification of gastric bleeding is used by doctors specifically when diagnosing such cases. The doctor begins his work with the following:
- The patient's medical history is collected. The doctor analyzes the symptoms of the pathological process.
- First of all, laboratory methods are prescribed to study the patient’s health status - a general analysis of a blood sample, a study of its coagulability.
- The patient is prescribed FGDS - fibrogastroduodenoscopy. If a person is admitted to the hospital with gastric or intestinal bleeding in critical condition, then this diagnostic method will be the only one for him.
Forest's classification for gastrointestinal bleeding will explain the examination results obtained using the FGDS technique. Its recognized effectiveness is confirmed by several factors:
- Helps document an episode of gastrointestinal bleeding.
- Determines the location of the damaged vessel.
- Sets the intensity of bleeding. And this helps specialists understand how much blood a person has lost.
Another plus is the convenience of the procedure. It is performed both at the patient’s bedside and in a specialized treatment room.
Analyzing the endoscopic classification of bleeding according to Forest, I would like to draw the reader’s attention to another useful function of FGDS. The technique allows you to influence the defect of a “leaky” vascular wall:
- clipping;
- coagulation;
- fibrin filling;
- injecting the damaged area with drugs that stop bleeding.
Indications for use
Indications for performing FGDS are the presence of the following diseases in the patient's medical history:
- peptic ulcer of the stomach and/or duodenum;
- malignant forms of cancer, in which the disintegration of neoplasms is observed;
- erosive gastritis;
- Randu-Osler syndrome (hereditary pathology in which defective blood vessels are formed);
- oncological and genetic pathologies of the circulatory system.
Categorical contraindications for endoscopic examination are the acute period of myocardial infarction, stroke, and a state of agony.
Additional Research
In addition to FGDS, the gastroenterologist will need other data about the patient’s well-being. A clear diagnosis will be established after several step-by-step studies. The doctor needs the readings to complement each other and create an overall picture.
A comprehensive study of the whole organism is necessary.
- Study of the patient's blood composition. A biochemical blood test is needed.
- Composition of urine.
- Medical history (anamnesis), as well as information about the presence of other diseases.
- MRI diagnostics of all internal organs.
If lethargy, pallor, and clouding of consciousness are observed - these are clear signs of blood loss, the patient’s blood pressure and hemodynamics of the heart must be monitored. Those diagnosed with any heart disease undergo fibrogastroscopy under the supervision of an experienced cardiologist.
Endoscopic classification of bleeding according to Forrest
- font sizedecrease font sizeincrease font size
The classification is applicable for ulcerative sources of bleeding
The Forrest classification plays an important role in assessing the patient's risk of rebleeding and death. Based on the endoscopic picture, it is possible to determine the volume of endoscopic manipulations to achieve hemostasis or the indications for surgical intervention.
F1A—stream bleeding from an ulcer
F1B—drip bleeding from an ulcer
FIIA—thrombosed vessels at the bottom of the ulcer
FIIB—blood clot closing the ulcer
FIIC—ulcer without signs of bleeding
- Causes of bleeding during early pregnancy: what to do?
FIII sources of bleeding were not detected
Another version of Forrest's classification:
F1 a- jet bleeding
F1b - parenchymal bleeding
F2a - thrombosed vessel at the bottom of the ulcer
F2b - blood clots at the bottom of the ulcer
F2c - inclusions of hydrochloric acid hematin at the bottom of the ulcer.
F3 - ulcer without signs of bleeding
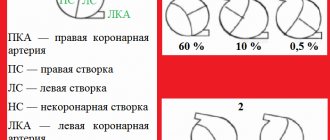
| Forrest classification | Rebleeding rate | Surgery | Deaths |
| Ia Ib | 55-100% | 35% | 11% |
| IIa IIb | 40-50% | 34% | 11% |
| 20-30% | 10% | 7% | |
| III | 5% | 0,5% | 2% |
Gastric resection
If type F1a is established - a pulsating stream, blood quickly fills the gastrointestinal tract. In some cases, self-medication should not be allowed. You need to call an ambulance immediately. Giant ulcers, which are more than 2.5-3 cm in diameter, and peptic ulcers are operated on urgently.
The tactics of surgeons when preparing for surgery consists of three points:
- Forrest group definitions.
- Carrying out early endoscopy, which determines the level of damage to the mucosa and the degree of risk.
- Determining the volume and timing of the operation. It is determined what kind of resection is needed: distal resection, proximal, or gastrectomy.
In cases where the ulcer is dangerous and there is a risk of repeated intense bleeding, a planned distal gastrectomy is prescribed. The operation is not dangerous. During this procedure, 2/3 of the organ, the pylorus, is removed. The remaining stump is connected to the small intestine or duodenum. The operation is possible only after the bleeding has completely stopped.
Total resection or gastrectomy with resection is the removal of more than 90% of the organ tissue. Prescribed after endoscopy when repeated ulcerations were observed, large volumes of blood were lost, and pyloric stenosis was found.
What may indicate the presence of stomach bleeding
Approximately 70% of all hemorrhages of the digestive tract are due to bleeding from ulcerated areas of its upper parts, namely the esophagus, duodenum and stomach. The characteristics of blood loss are determined by the duration of development of the pathological condition that provoked damage to human blood vessels, as well as the general condition of the patient’s body.
- Bleeding in the middle of the cycle: causes
Symptoms that indicate a person may have stomach bleeding include:
- pale skin, cold sweat;
- general weakness, dizziness, flashing of black spots before the eyes;
- pain in the heart area;
- constant feeling of thirst;
- uncontrollable vomiting. In this case, by the nature of the vomit, one can tentatively guess in which part of the digestive tract the source of bleeding is localized. Thus, in case of bleeding from the esophagus, the vomit contains an admixture of scarlet blood, and in case of gastric bleeding, where the blood is exposed to gastric juice, the vomit has the appearance of coffee grounds;
- melena stool (black). Blood is detected in a stool test. Since gastric emptying takes at least 12 hours, this is not an early symptom.
- low blood pressure, pulse becomes frequent and weakly filled;
Cold sweat as a sign of gastric hemorrhage
How is diagnosis carried out?
If a person is suspected of having gastric bleeding, specialists use an integrated approach to diagnose it.
That means:
- Signs of arterial bleeding and first aid
- collecting anamnesis, that is, history, disease;
- identifying early signs of gastric bleeding;
- laboratory testing of blood to determine its clinical indicators (primarily, determining the level of hemoglobin and studying the properties of coagulation);
- conducting instrumental examination using, first of all, endoscopic methods (FGDS).
Carrying out fibrogastroduodenoscopy (FGDS) allows you to establish the presence of gastric bleeding, determine the location of the damaged vessel and the degree of intensity of blood loss.
Further treatment
The diagnostic results allow you to choose the optimal treatment method for a particular patient:
- Conservative. This is drug therapy.
- Operational. This is a surgical intervention of various specifications and scope - from excision and suturing of the ulcer itself to resection of the gastric region.
Today, as progress develops, Forest's classification is used in various modifications and variations. However, the entire system of grading gastrointestinal bleeding is still aimed at determining the activity of the pathological process and selecting the best treatment option for the patient. Classification helps to identify the likelihood of relapse of the pathology, which can be fatal for the patient.
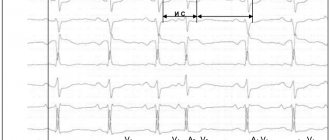
Sequence of assistance
If the patient received anticoagulants before bleeding occurred, they should, in most cases, be discontinued. Assess the severity of the condition and the estimated amount of blood loss based on clinical signs. Vomiting blood, loose stools with blood, melena, changes in hemodynamic parameters - these signs indicate ongoing bleeding. Arterial hypotension in the supine position indicates large blood loss (more than 20% of the blood volume). Orthostatic hypotension (a decrease in systolic blood pressure above 10 mm Hg and an increase in heart rate by more than 20 beats per minute when moving to a vertical position) indicates moderate blood loss (10-20% of blood volume);
In the most severe cases, tracheal intubation and mechanical ventilation may be required before endoscopic intervention. Provide venous access with a peripheral catheter of sufficient diameter (G14-18); in severe cases, install a second peripheral catheter or perform catheterization of the central vein.
Take a sufficient volume of blood (usually at least 20 ml) to determine the group and Rh factor, combine blood and conduct laboratory tests: general blood count, prothrombin and activated partial thromboplastin time, biochemical parameters.