Vessels susceptible to atherosclerosis
With atherosclerosis, large main arteries are affected - the aorta and its branches.
Among the sections of the aorta, the abdominal aorta is most susceptible to atherosclerosis. Clinically significant atherosclerosis of the aortic arch and thoracic aorta is much less common. From the peripheral arteries and directly the branches of the aorta, the following should be distinguished:
- coronary (coronary) vessels,
- nourishing the heart,
- brachiocephalic arteries (BCA),
- subclavian arteries,
- common and internal carotid arteries (ICA),
- vertebral arteries,
- arteries of the limbs,
- renal arteries,
- celiac trunk,
- mesenteric arteries.
When several arterial basins are affected, they speak of generalized (widespread) atherosclerosis. Most often, atherosclerosis affects the coronary, brachiocephalic basins, as well as the vessels supplying blood to the lower extremities.
Signs of multiple sclerosis
Some of the first symptoms are loss of vision, paresis, paralysis, weakened sensitivity of the limbs and other parts of the body, and impaired coordination of movements. A person may have the feeling that there is “frozen” on the face, or that the leg or hand is “not his.”
With the development of multiple sclerosis, the following is observed:
- a sharp decrease in performance, mental functions, concentration;
- sudden dizziness for no apparent reason;
- speech problems;
- unilateral decrease in vision up to blindness (impairments appear and disappear);
- problems with coordination of movements;
- impaired motor skills of the hands (the patient finds it difficult to do small work, handwriting noticeably deteriorates, etc.);
- convulsions and non-convulsive epileptic seizures;
- complete or partial paresis of the limbs;
- disturbance of urination, bowel movements, and genital function;
- pain without a clearly defined focus
- anxiety, sudden mood swings, etc.
If several symptoms from the above list appear simultaneously, you should immediately consult a doctor.
The appearance of causeless dizziness may be one of the signs of MS
Why is atherosclerosis dangerous?
Atherosclerotic or, as they are also called, cholesterol plaques, gradually narrow the lumen of the arteries and make them less elastic. This creates an obstacle to normal blood flow and leads to insufficient blood supply to the feeding organ.
The narrowing of the lumen of a vessel by an atherosclerotic plaque is called stenosis, and complete blockage of the lumen is called occlusion. Symptoms of the disease begin to appear at a certain degree of arterial stenosis, in which case we can talk about stenosing vascular atherosclerosis. For example, if the arteries of the heart narrow, the blood flow to the heart muscle (myocardium) decreases. This can cause chest pain and shortness of breath, which can ultimately lead to a heart attack. Particles of atherosclerotic plaque can break off from the walls of the arteries and be transported with the blood to narrower vessels, completely blocking their lumen.
In addition, the danger of atherosclerosis lies in the fact that particles of atherosclerotic plaque can break off from the walls of the arteries and be transported with the blood to narrower vessels, blocking their lumen. Blood clots can form in the area of atherosclerotic plaques, partially or completely blocking the lumen of the artery. In such cases, there is an acute disruption of the blood supply to the feeding organ, which can lead to dangerous, often life-threatening complications. The described mechanisms are often the cause of stroke, myocardial infarction, thrombosis and obliterating atherosclerosis of the vessels of the lower extremities.
4.Treatment
Neuropsychiatric specialists deal with cerebral atherosclerosis. And if the question of complete healing and restoration of already lost functions is not raised today, then it is possible and necessary to significantly slow down the process by improving the somatic and psycho-emotional state of the patient. A special diet is prescribed; all self-destructive habits, of course, are completely excluded. An individual medication regimen is selected: anti-cholesterol, hypotensive, antiplatelet, vitamin-antioxidant, nootropic (all components according to indications), as well as certain types of massage, exercise therapy, herbal medicine. In some cases, vascular and neurosurgical interventions are indicated and successfully performed.
In conclusion, here is a saying from dark medical humor: the connection between atherosclerosis and old age is that both processes are incurable. But if with regard to old age it is indeed better to refrain from commenting, then regarding atherosclerosis we will still risk clarifying: it is irreversible YET, at the present time of the development of our knowledge, ideas and technologies. Let us remember: what kind of diseases were not considered incurable, including quite recently.
Clinical picture or symptoms of atherosclerosis
Symptoms of atherosclerosis depend on the organ that feeds the vessels affected by atherosclerotic plaques. Thus, when the coronary arteries are damaged, the heart muscle (myocardium) suffers, and coronary heart disease (CHD) develops. Signs of angina appear - chest pain and shortness of breath during exercise or at rest.
Among the vessels supplying the brain, the internal carotid and vertebral arteries are most often affected by atherosclerosis. In this case, patients may experience dizziness, impaired memory and vision, episodes of loss of sensitivity or movements in the face and limbs, and speech disorders. With the long-term existence of an atherosclerotic plaque in the lumen of the carotid artery, ulcerations may occur on its surface, as well as blood clots, which can be carried with the bloodstream into the vessels of the brain, causing clinical manifestations such as paresis/paralysis, sudden loss of sensation in the limbs or in the face, as well as temporary blindness.
When the vessels of the legs are damaged, symptoms of intermittent claudication appear - pain in the calf (less often in the gluteal and thigh) muscles that occurs when walking. With the progression of obliterating atherosclerosis of the vessels of the lower extremities, trophic ulcers and gangrene of the extremity ultimately occur. With atherosclerosis of the iliac arteries, potency disorders (erectile dysfunction) may also occur.
Treatment
Therapy involves the use of medication (conservative) and surgical techniques.
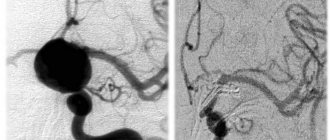
Surgery
If an ultrasound reveals more than 70% reduction in the diameter of a cerebral artery, the question arises about the need for surgical treatment of the damaged vessel. The most commonly used method is carotid endarterectomy. During the procedure, the vessel is dissected at the site of the blood clot, which is removed, and the integrity of the vessel is restored using sutures.
Other methods are endovascular operations, stenting.
Drug treatment
It is prescribed only by a doctor, taking into account contraindications, medical history and based on the results of studies and tests.
Therapy for cerebral atherosclerosis is aimed at:
- harmonization and restoration of lipid metabolism;
- lowering cholesterol levels (find out the norm from the table);
- elimination of metabolic disorders;
- treatment of concomitant diseases.
To solve these problems, several groups of medications are prescribed:
Statins are an active group of drugs that block cholesterol synthesis in the body, reduce its amount and prevent the formation of plaques. These drugs are Lovastatin, Mevacor, Fluvastin, Mekafor, Simvastatin, Pravastatin.
Means for improving microcirculation , dilating blood vessels, relieving spasms and at the same time preventing platelets from aggregating (sticking together) into clots:
- "Actovegin", "Cavinton", "Curantil".
- “Parmidin”, “Anginin”, “Aspirin” restore blood flow in small vessels, reduce the permeability of the walls, suppress the adhesion of platelets into clots, stimulate the resorption of blood clots, and prevent the deposition of fats and cholesterol on the vascular wall.
Vasodilators:
- “Nicotinic acid”, Nikoshpan” - expand small capillaries, strengthen the cells of the arterial wall, and effectively help reduce cholesterol concentrations. From simple standard means - “Papaverine”, “Eufillin”.
- Among the more progressive medications: Isoptin, Lomir, Amlodipine, Diazem. Cinnarizine and Nimodipine are suitable for long-term use.
- Medicines containing the alkaloid of the periwinkle plant - Vinpocetine (Cavinton, Bravinton) allow you to dilate blood vessels and stimulate metabolism.
- Dietary supplements based on the Gingko Biloba plant are good at relieving vasospasm, stimulating the work of brain cells, and reducing blood viscosity. Taking Gingium, Tanakan, Ginkor Fort is not combined with medications containing aspirin (Trombass, Cardio-magnyl) due to the risk of a serious increase in blood flow and bleeding.
Nootropic drugs activate the process of energy exchange in brain cells, improve memory, mental activity, cerebral circulation and cell resistance to oxygen deficiency.
They treat problems of mental disorders, senile dementia: Piracetam, Nootropil, Bemitil, Cerebrolysin, Aminalon, Sermion (nicergoline), Meclofenoxate, Phezam, Biotredin, Vinpocetine.
Medicines that activate energy metabolism and remove lipids - Lipostabil, Omacor, Eikonol, Thioctic acid.
Medicines to prevent the formation of blood clots when blood viscosity increases and the content of prothrombin in it increases - “Trental”, “Aspirin-cardio”, “TrombASS”, “Pentoxifylline”, “Cardiomagnyl”.
Doctor's advice
There are risk factors for developing stroke and heart attack in the next 5 years that have long been studied and taken into account, called the “SCORE Scale”, in which the higher the cholesterol, the greater the risk. Accordingly, cerebral atherosclerosis increases the risk of sudden cardiovascular accidents. In the first place in the treatment regimen are statins - drugs that lower cholesterol and help reduce the volume of plaques.
Victoria Druzhikina Neurologist, Therapist
Additional tools:
Fibrates – suppress the formation of fats and total cholesterol: “Clofibrate”, “Gemfibrozil”, “Fenofibrate”, “Atromid”, “Bezafibrate”, “Atromidine”.
Fibrates currently cause much controversy in the treatment of cerebral atherosclerosis. When used uncontrolled, fibrates are dangerous, so the dosage regimen and therapy regimen are agreed upon with a cardiologist.
“Nicotinic acid” and “Enduracin” are recommended in cases where atherosclerosis is associated with an increased amount of high-density cholesterol. They dilate blood vessels, but cause a rush of blood to the skin, so their use should be carried out under the supervision of a doctor.
Hypocholesterolemic drugs - Neomycin, Guarem, Colestipol, Probucol, Lipostabil, Eikonol, Benzaflavin - reduce cholesterol, stabilize metabolism, and suppress the formation of blood clots.
In addition to the main treatment medications, it is advisable to take:
- Antioxidants that suppress oxidation processes: Mexidol, vitamins A, E, Aevit, P (strengthen the walls and increase the density and elasticity of blood vessels), microelements - potassium, silicon, selenium, vitamin C, which prevents the formation of fat deposits on the walls of arteries , group B improves the functioning of nerve cells. The use of Ascorutin (vitamin C plus rutin) requires monitoring the level of blood viscosity.
- For neurological manifestations and depression, antidepressants are used: Paxil, Azafen, Amitriptyline.
- When phobias, panic attacks, or severe anxiety appear, tranquilizers are prescribed: Alprazolam, Diazepam, Atarax, Phenazepam.
- If sleep is disturbed, sleeping pills and antidepressants (Donormil, Nitrazepam) are prescribed.
- For headaches and myalgia, the use of drugs that relieve pain and spasms is indicated: “Spazgan”, “Spazmalgon”, “Pentalgin”.
Among the more progressive medications: Isoptin, Lomir, Amlodipine, Diazem. Cinnarizine and Nimodipine are suitable for long-term use. Nootropics are prescribed with caution for dementia, as well as in older people - they activate the nervous system, and thus, as a side effect, can cause hyperexcitability, irritability, and aggression.
Physiotherapy for cerebral atherosclerosis
Aimed at activating blood circulation in the brain and processes in nerve cells, increasing arterial tone, and improving adaptive capabilities. This:
- Electrophoresis with medications.
- Hydrotherapy using carbon dioxide, oxygen, iodine-bromine, sodium, radon baths.
- Electrosleep procedures to strengthen and restore the nervous system.
- Special therapeutic exercises to improve and stimulate proper motor skills, motor functions, and relieve muscle spasms.
Diet therapy
The main provisions of the diet for cerebral atherosclerosis:
- Salt per day up to 3 g.
- Meals are frequent, in small portions.
- The amount of fat is no more than 65 g per day, of which 72% is vegetable.
- The amount of protein is not limited. Animal protein prevents fatty liver and cholesterol deposits in blood vessels.
What you can do:
- lean veal, pork, beef, turkey, fish;
- eggs in the amount of 1 pc. per day: in the form of steamed, baked, soft-boiled omelettes; milk, low-fat cottage cheese, kefir, peas, beans, buckwheat, wheat, oatmeal;
- once a week a little caviar and tongue are allowed. 10-20 g per week of butter is allowed;
- sunflower, rapeseed, corn, cottonseed, olive seeds promote intestinal motility and remove excess cholesterol;
- seafood is very healthy (up to 6 times a week): fish, squid, shrimp, mussels, seaweed, kelp;
- vinaigrettes, salads from cucumbers, zucchini, cabbage, tomatoes, potatoes, pumpkin, soybeans, eggplant, pumpkin, dill;
- You can have low-fat sausage, ham, mild cheeses, dry cookies, marmalade, dried fruit candies, muesli.
What not to do:
- animal fats, offal products saturated with cholesterol, including liver, brains, kidneys are excluded;
- limit sweet dishes, fresh white bread, pure sugar, jam, honey, jams, cakes, buttery sweet cookies;
- Rich meat and mushroom soups, cream, ice cream, butter and custard creams, mayonnaise and sauces based on it, dark chocolate, strong coffee, tea, and alcohol are not recommended.
Folk remedies
In complex therapy of atherosclerosis, traditional methods are used with caution and after consultation with a doctor. They must be combined with medications
Among them:
- Collection for spasms of cerebral vessels, nervous tension. A collection is prepared from valerian root, cudweed, and St. John's wort in equal parts. Drink as an infusion.
- Honey and lemon juice are mixed equally with vegetable oil and taken a teaspoon in the morning (dangerous for allergies and gastritis).
- Drink 100 g of freshly squeezed potato juice for frequent headaches (harmful for stomach diseases).
- An alcohol tincture with garlic and lemon along with zest is known (extremely dangerous for gastritis, peptic ulcers, inflammation of the pancreas).
- Dill seeds (teaspoon), brewed in a glass of boiling water. Drink as tea for headaches.
Despite the fact that atherosclerosis occupies only the walls of blood vessels, the consequences for the brain, the entire body, psyche and intellect are devastating. A person gradually loses his personal qualities and turns into a thoughtless organism that requires constant care and regular feeding.
To prevent such an existence, you should pay attention to the very first signs of the disease, do all the necessary examinations and take timely the whole range of measures aimed at recovery.
How to recognize and how to treat cerebral atherosclerosis, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://www.angiolsurgery.org/recommendations/2013/recommendations_brachiocephalic.pdf
Rate how helpful this article was
4.5 11 people voted, average rating 4.5
Did you like the article? Save it to your wall so you don’t lose it!
Causes of atherosclerosis
The causes of atherosclerosis remain not fully understood. It is believed that the initial stages of atherosclerosis occur already at a young age, but it usually reaches its clinical significance in people of the older age group (over 50 years). There are risk factors for atherosclerosis, the impact of which can significantly slow down its progression, reduce the severity of its manifestations and prevent the occurrence of complications.
Risk factors for atherosclerosis
- High blood pressure,
- High levels of cholesterol in the blood - low-density lipoprotein (LDL),
- Diet high in animal fats
- Smoking,
- Obesity,
- burdened heredity,
- Diabetes.
Cholesterol and atherosclerosis
It is important to regularly monitor blood tests for the so-called “bad” cholesterol, which is deposited in the artery wall and causes the appearance and growth of atherosclerotic plaques. If the level of low-density lipoprotein cholesterol is elevated, you should consult a physician, cardiologist or vascular surgeon. In the absence of contraindications, it is recommended to take statins - medications that reduce the level of “bad” cholesterol in the blood.
2. Reasons
To date, the etiopathogenetic mechanism of atherosclerosis continues to be the subject of intensive study and discussion. About ten main hypotheses are considered (viral, hereditary, chlamydia, autoimmune, etc.), each of which has the right to exist and finds well-reasoned confirmation. Perhaps atherosclerosis refers to the so-called. polyetiological, or multi-cause processes, or against the background of these conditions, is triggered by some common, not yet known trigger factor. However, risk factors have been quite reliably established that significantly increase this likelihood:
- - smoking and drinking alcohol;
- — physical inactivity combined with overeating and obesity;
- - arterial hypertension;
- - situations of chronic distress;
- - age-related hormonal changes;
- - diabetes;
- — certain metabolic disorders (metabolism), especially in relation to fats and proteins;
- - “viscosity” of blood (increased coagulability).
Visit our Cardiology page
Prevention of vascular atherosclerosis
The best treatment for atherosclerosis is its prevention. It is necessary in order to prevent the occurrence of the first signs and symptoms of the disease, which will help overcome atherosclerosis already in the initial stages. Prevention consists primarily of diet: do not abuse fatty foods, as well as mandatory smoking cessation. If you have hypertension (hypertension), it is necessary to maintain normal blood pressure values by monitoring it, as well as taking medications, after consulting with a therapist or cardiologist. In the presence of diabetes mellitus, it is recommended to maintain normal blood glucose levels by taking glucose-lowering drugs prescribed by an endocrinologist, daily monitoring of blood glucose levels, and regular monitoring by an endocrinologist.
Causes of hippocampal sclerosis
The central question of the etiology of FH is to clarify what occurs primarily: structural pathology of the hippocampus, which triggers chronic drug-resistant epilepsy, or, conversely, long-term pathological electrical activity leads to sclerosis over time. It is important to note that a significant proportion of patients with risk-related epilepsy associated with HS experience febrile seizures or other acute pathology of the central nervous system (trauma, anoxia, neuroinfection) in early childhood, which is referred to as initial precipitating damage. The acquired nature of HS is supported by those rare observations when this pathology occurs in one of the monozygotic twins, the second twin does not have sclerosis, and, therefore, the genetic factor is not paramount. However, hereditary familial forms of temporal lobe epilepsy (for example, a group of epilepsies associated with mutations in the SCN1a and SCN1b genes encoding sodium) indicate that a genetic factor also plays a role, causing hippocampal sclerosis in some of these patients without a history of febrile seizures . Speaking about the acquired nature of the disease, it should also be taken into account that not every type of seizure is associated with the development of FH: autopsy data indicate that long-term uncontrolled epilepsy with frequent generalized seizures does not lead to neuronal loss in the hippocampus, as does afebrile status epilepticus. On the other hand, febrile status epilepticus is accompanied by MRI evidence of hippocampal edema. The answer to the question of how often the status of febrile seizures in a child is realized in FH and drug-resistant epilepsy may be provided by the prospective study FEBSTAT. It has already been established that out of 226 children after febrile seizure status, 22 had MRI signs of hippocampal edema, most pronounced in the Sommer sector (CA1). Of these 22 patients, repeat MRI at various times was performed in 14; in 10 cases, signs of hippocampal sclerosis were detected. However, out of 226 children, epilepsy was diagnosed in only 16 patients and in most cases it was non-temporal epilepsy. That is, on the one hand, febrile status does not always lead to epilepsy with hippocampal sclerosis, on the other hand, the time interval between precipitating brain injury and the appearance of temporal lobe epilepsy can be more than 10 years, and the study does not yet have a follow-up of such a duration. Genetic studies also indicate that the etiology of FH is heterogeneous. Genome-wide association studies have shown that febrile seizures with hippocampal sclerosis may be a genetic syndrome, as they are associated with the presence of a specific allele of a single nucleotide sequence located near the sodium channel gene SCN1A. This association was not found for cases of epilepsy with FH without febrile seizures. The consensus opinion of epileptologists is that there is a certain initial genetic predisposition, which is realized in hippocampal sclerosis in the presence of a certain damaging factor (double hit hypothesis).
Which doctor treats vascular atherosclerosis?
If atherosclerosis is suspected, an examination by a specialist is necessary:
- Angioneurologist - for atherosclerosis of cerebral vessels;
- Cardiologist - for atherosclerosis of the heart vessels;
- Vascular surgeon - for signs of diseases of the arteries of the arms or legs, neck, chest and abdominal cavity.
It is necessary to see a specialist (vascular surgeon) if you have one or more risk factors for atherosclerosis, and also have complaints characteristic of arterial diseases. It is especially important to seek qualified help during the initial manifestations of the disease, when it is possible to prevent the development of severe complications of atherosclerosis.
Before prescribing instrumental diagnostic methods, the doctor must evaluate the patient’s complaints. Collect information about past illnesses and past treatments. An objective examination provides detailed information about the severity and extent of the disease.
In some cases, the diagnosis of atherosclerosis can be excluded at the stage of the initial examination. If vascular atherosclerosis of one location or another is detected, the doctor may prescribe an additional examination.
Laboratory and instrumental studies that can be used to diagnose atherosclerosis:
- ultrasound duplex scanning of blood vessels,
- X-ray contrast angiography,
- CT scan,
- Magnetic resonance imaging,
- ECG,
- treadmill test,
- lipidogram, etc.
Senile sclerosis
Syphilis
Encephalitis
Stroke
Diabetes
2839 04 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Senile sclerosis: causes, symptoms, diagnosis and treatment methods.
Definition _
Senile sclerosis is called memory impairment in older people. In fact, there is no such disease officially, and “senile sclerosis” means late-life dementia, or senile dementia - acquired dementia, which is characterized by a persistent decline in cognitive activity, complete or partial loss of knowledge and practical skills, the inability to acquire new ones, and the collapse of mental functions .
This condition can manifest itself as disturbances in memory, abstract thinking, judgment, speech, the ability to perform purposeful actions, and recognize objects.
Causes of senile sclerosis
The expression “senile sclerosis” may owe its name to cerebral atherosclerosis (atherosclerosis of the blood vessels of the brain) as the earliest known cause of dementia in the elderly.
The term "sclerosis" means the replacement of normal connective tissue.
In English there is no phrase similar to our “senile sclerosis”, but the expressions Alzheimer's disease (Alzheimer's disease) or senile dementia (senile dementia) are used.
Currently, a large number of possible causes of dementia are known:
- metabolic (endocrinopathies, Wilson's disease);
- traumatic (subdural hematoma, hydrocephalus);
- tumor;
- infectious (brain abscess, tertiary cerebral syphilis, hydrocephalus, meningitis and encephalitis);
- vascular (cerebral infarction, multiple repeated cerebrovascular accidents);
- degenerative (Alzheimer's disease, Pick's disease);
- congenital (Huntington's disease), etc.
All these pathological conditions share common features:
- endogenous nature of the disease;
- slow onset and progressive course - from mild dementia to total dementia;
- presence of neurological disorders;
- familial nature of the disease;
- hallucinations, delusions.
Alzheimer's disease (AD) is a common form of primary degenerative dementia of late age, characterized by a subtle onset, steady progression of memory impairment and mental function until the total collapse of intelligence and mental activity.
Early-onset AD (presenile dementia of the Alzheimer's type) develops mainly before the age of 65 and leads to total dementia with severe speech disorders and impaired ability to perform sequential sets of conscious actions. The leading factor in the occurrence of early-onset asthma is genetic burden (10% of the total number of patients with asthma). Mutations in the genes encoding the proteins presenilin-1, presenilin-2 and amyloid precursor protein are associated with the risk of developing Alzheimer's disease in almost 100% of cases.
In AD with late onset at 65-85 years of age (senile dementia of the Alzheimer's type), the most complex forms of intellectual activity associated with abstract thinking and criticality are affected.
Risk factors for developing asthma:
- modifiable
(low level of education and low intellectual activity, physical inactivity, smoking, uncontrolled arterial hypertension in middle and old age, hyperlipidemia, hyperhomocysteinemia, diabetes mellitus, obesity, depression); - non-modifiable
(elderly and senile age, family history of asthma, carriage of genetic polymorphisms, presence of the APOE4 allele, female gender, history of traumatic brain injury).
In Alzheimer's disease, there are disturbances in the metabolism of amyloid precursor protein.
Normally, this protein is broken down into polypeptides that are not pathogenic (that is, not capable of causing disease). In AD, aggregation (sticking together) of its insoluble fragments occurs into a pathological protein β-amyloid, which has neurotoxic properties. Deposition of this protein in the brain parenchyma and in the walls of blood vessels (with the formation of senile plaques) leads to damage and death of neurons. Senile dementia can be of vascular origin and develops:
- as a result of a single heart attack or hemorrhagic stroke, which is localized in a strategically important area of the brain for cognitive and mental activity;
- as a result of repeated episodes of acute cerebrovascular accident of the ischemic type of cortical-subcortical localization;
- as a result of damage to the terminal small-caliber vessels supplying blood to the subcortical basal ganglia and deep parts of the white matter of the brain;
- as a result of disturbances in systemic hemodynamics with a sharp decrease in cerebral circulation (acute heart failure, a decrease in circulating blood volume, a pronounced and prolonged decrease in blood pressure).
As a result of vascular events in the brain, post-ischemic or post-hemorrhagic cysts, changes in white matter, death of nerve cells, and linear deposits of iron-containing pigment formed during the breakdown of blood occur.
Risk factors for developing dementia of vascular origin may include:
- arterial hypertension, coronary heart disease, heart rhythm disturbances;
- high cholesterol, atherosclerosis;
- diabetes;
- smoking;
- obesity;
- high levels of homocysteine;
- rheumatic diseases, vasculitis;
- blood clotting disorders;
- amyloid angiopathy;
- congenital vascular anomalies, etc.
Classification of the disease
Due to the cause of occurrence, senile dementia can be:
- vascular,
- atrophic (Alzheimer's type syndrome, dementia with Lewy bodies, dementia caused by chorea, Huntington's dementia),
- mixed.
By localization:
- cortical - with predominant damage to the cerebral cortex (Alzheimer's disease, frontotemporal lobar degeneration, alcoholic encephalopathy);
- subcortical - with predominant damage to subcortical structures (progressive supranuclear palsy, Huntington's disease, Parkinson's disease, multi-infarct dementia);
- cortical-subcortical (Lewy body disease, corticobasal degeneration, vascular dementia);
- multifocal - with multiple focal lesions (Creutzfeldt-Jakob disease).
There are mild, moderate and severe degrees of dementia.
Symptoms of senile sclerosis
Mild degree
: professional activity and social activity are possible, but limited, the circle of communication and interests is narrowed; independence in everyday life is maintained, but reminders, assistance in mastering new information and solving financial issues, and psychopathic sharpening of personality traits may be required.
Moderate degree
: decreased ability to use household appliances, problems with hygiene, dressing, cooking, movement, daily activities, difficulties in living independently. However, the patient can still be left alone for some time.
Severe degree
: the patient needs help in almost all activities and outside care.
With subcortical localization of the process, the earliest symptom is memory impairment. Patients demonstrate slowness, rigidity of mental processes, difficulties in switching from one type of activity to another, errors in planning activities and performing sequential actions.
Frontotemporal dementia is characterized by changes in personality and behavior. Within a short period of time, a person completely loses the ability to cope with his affairs and exist independently.
In patients with cortical-subcortical dementia, symptoms of cortical and subcortical lesions predominate.
Multifocal dementias are characterized by the presence of multiple disorders: speech, recognition, memory, spatial perception, purposeful movements and actions. There are also subcortical disorders:
- sustained repetition of any phrase, activity, emotion, sensation (perseveration);
- sudden, short, jerky movements of the muscles of the limbs, face, torso, not accompanied by loss of consciousness (myoclonus);
- pyramidal (paralysis, paresis, pathological reflexes) and extrapyramidal disorders (muscle tone disorders).
These disorders are combined with cerebellar pathology (disturbances in gait and coordination of movements).
There is increasing drowsiness. In Alzheimer's disease, first there is a decrease in memory for current events: insignificant details, new names, and the contents of recently read books are forgotten. Criticism of one's condition is preserved. The average duration of this stage in older people is about 5 years. Subsequently, the disease progresses, difficulties appear in everyday life: memorization of new material is impaired, while the storage of memorized information does not suffer, difficulty in orienting in unfamiliar terrain and time arises, speech disorders appear, and personal characterological characteristics become sharpened.
Personal changes are characterized by suspicion and conflict, delusional ideas directed against the immediate environment. Patients suspect relatives of stealing their things, planning to leave them without help, and putting them in a nursing home. In later stages of the disease, aggressiveness, inappropriate sexual behavior, untidiness, hallucinations, and decreased criticism of one’s condition are noted.
The clinical picture of senile dementia of vascular origin is determined by the volume and localization of changes in the brain.
The course of the disease can begin acutely with partial improvement and gradual deterioration. The following symptoms are observed: confusion, severe apathy, restriction of daily activity up to failure to comply with personal hygiene rules, severe memory impairment for current events, impaired perception of spatial relationships, difficulties with counting, understanding logical and grammatical speech structures. Patients cannot properly organize their activities, often abandon the work they started, get tired quickly, are unable to analyze information, work with several sources of information at once, or quickly move from one task to another. Emotional disorders appear in the form of a decrease in mood, the development of depression or anger.
Movement disorders and gait disturbances may be observed. Slowness and staggering appear, the patient cannot take the first step, marks time, the legs do not leave the floor, but slide along it (“skier’s gait”), balance suffers, the risk of falling increases at the beginning of walking, when turning and when stopping. The advanced stage of the disease is characterized by frequent urination and periodic urinary incontinence. Subsequently, a complete loss of control over the function of the pelvic organs develops.
The basis of the clinical picture of mixed dementia is a combination of focal neurological symptoms and mental disorders: disturbances in walking, speech, swallowing, urination, attention and memory. Patients with mixed dementia have more pronounced visual-spatial impairments, decreased attention, and the sleep-wake cycle is disrupted.
Thus, dementia syndrome is characterized by a deep impoverishment of intelligence, the use of past experience becomes impossible. Criticism towards one's condition and surroundings suffers greatly. The individual's adaptation to society is disrupted.
Diagnosis of senile sclerosis
The diagnosis of senile dementia is established on the basis of:
- complaints and information received from the patient and the patient’s environment (relatives, friends, acquaintances);
- data on the impact of existing disorders on the patient’s daily (basic and instrumental) activities;
- available drug therapy (drugs with anticholinergic properties, antipsychotics, barbiturates, benzodiazepine derivatives, antihistamines, some beta-blockers, HMG-CoA reductase inhibitors (statins) with lipophilic properties, cardiac glycosides and other drugs);
- patient examination data in order to detect concomitant diseases that can lead to the formation or aggravation of the severity of mental and cognitive disorders (hypothyroidism, diabetes mellitus, deficiency of vitamin B12, folic acid, neuroinfection (syphilis, HIV, etc.), cancer, renal, liver failure and etc.);
- certain data from laboratory and instrumental examination methods to clarify the diagnosis:
•
biochemical blood test, including:
- total protein, albumin, protein fractions;
How to treat vascular atherosclerosis: drug treatment of atherosclerosis
Vascular atherosclerosis can be combated conservatively and surgically. Conservative treatment of atherosclerosis is used for mild and non-stenotic forms of atherosclerosis. It includes the fight against risk factors for atherosclerosis, as well as taking medications such as statins (Simvastatin, Atorvastatin, Rosuvastatin, etc.) and antiplatelet agents (acetylsalicylic acid, clopidogrel, etc.), which prevent further growth of atherosclerotic plaques and the formation of blood clots on them. surfaces. Medications are prescribed for permanent or long-term use.
Pathogenesis of hippocampal sclerosis
Hippocamal sclerosis has two fundamental pathological characteristics: the first is a sharp decrease in the number of neurons and the second is hyperexcitability of the remaining nervous tissue. One of the key roles in epileptogenesis in HS is played by the sprouting of mossy fibers: abnormal axons of granular cells, instead of innervating the SA cells of the hippocampus, reinnervate the molecular neurons of the dentate gyrus through excitatory synapses, thus creating local electrical circuits capable of synchronizing and generating an epileptic seizure. An increase in the number of astrocytes, gliosis may also play a role in epileptogenesis, because altered astrocytes cannot sufficiently reuptake glutamate and potassium. Proinflammatory cytokines, such as IL-1β, IL 1, TNFa, can also act through the mechanism of increasing glutamate release and decreasing reuptake, GABA inhibition. In this regard, the role of herpes virus type 6, the DNA of which is found in the brain tissue of patients with temporal lobe epilepsy, is discussed in the pathogenesis of FH.
Can vascular atherosclerosis be reversed?
At the moment, there are no drugs that can get rid of atherosclerosis and cleanse blood vessels from atherosclerotic plaques.
Atherosclerosis is an irreversible disease and cannot be completely cured. For advanced forms of atherosclerosis, surgical treatment is often used. Modern surgical methods make it possible to perform the operation effectively, in a low-traumatic manner and without serious consequences for the body, to restore the lumen of a vessel affected by atherosclerosis and to resume sufficient blood flow to the organ.
MRI anatomy of normal and sclerotic hippocampus
A-T2 coronal section: sclerosis of the right hippocampus, a decrease in its volume is determined, the absence of internal structure compared to the left hippocampus. B – the same section with explanations. The red line outlines the hippocampi (a decrease in the volume of the right hippocampus is visible), and the blue line outlines the subiculum on the left. The yellow line in the center of the hippocampus is drawn along the deep part of the hippocampal sulcus (in Figure A, this sulcus is not identified in the right hippocampus). FG – fusiform gyrus, ITG – inferior temporal gyrus. C – FLAIR coronal section showing decreased volume and hyperintense signal from the right hippocampus.
A fundamental point in understanding the electrophysiology of medial temporal lobe epilepsy is the fact that the scalp EEG itself does not reveal epiactivity in the hippocampus, which has been demonstrated in numerous studies using intracerebral electrodes, i.e. for the appearance of epiactivity on the scalp EEG in the temporal region, its distribution is required from the hippocampus to the adjacent temporal lobe cortex. At the same time, the main clinical manifestations of an attack in medial temporal lobe epilepsy are associated with the spread of epiactivity outside the hippocampus: déjà vu is associated with excitation of the entorhinal cortex, a feeling of fear - with the amygdala, abdominal aura - with the insula, oroalimentary automatisms with the insula and frontal operculum, dystonia in the contralateral arm - with the spread of excitation to the ipsilateral basal ganglia. These anatomical and electrophysiological features may cause the patient to have seizures that are very similar to temporal paroxysms, but actually have an extrahippocampal and extratemporal onset. As experience in the surgical treatment of temporal lobe epilepsy accumulated, it became obvious that removal of the medial structures of the temporal lobe makes it possible to get rid of seizures completely in 50–90% of patients, but in some cases the frequency of seizures does not change at all. Data from studies of electrical activity of the brain using intracerebral electrodes and analysis of unsuccessful surgical outcomes have shown that in some cases the reason for the persistence of seizures after removal of the SG is the presence of a larger epileptogenic zone that extends beyond the hippocampus. Brain regions anatomically and functionally associated with the hippocampus, such as the insula, orbitofrontal cortex, parietal operculum, and the junction of the parietal temporal occipital lobe, can generate seizures similar in clinical and EEG picture to temporal paroxysms. The concept of “temporal lobe epilepsy plus” (preferably temporo-peresylvian (Patrick really doesn’t like plus)) has been proposed to describe situations where hippocampal sclerosis exists along with the extratemporal seizure initiation zone. In this regard, it is important to determine the indications for invasive EEG studies in temporal lobe epilepsy caused by hippocampal sclerosis. Warning symptoms are a taste aura, an aura in the form of vertigo, and noise. Interictal epiactivity is most often localized bilaterally in the temporal regions or in the precentral region. Ictal epiactivity in temporal plus forms is more often observed in the anterior frontal, temporoparietal and precentral areas. Differential diagnosis of temporal lobe epilepsy from temporal lobe epilepsy plus, carried out by a qualified epileptologist, is key in planning surgical intervention and predicting treatment outcome.
What does multiple sclerosis look like on an MRI?
Diagnosis of multiple sclerosis allows us to identify the full picture of pathological changes. The following localization of lesions is considered typical:
- superficial parts of the pons;
- paraventricular substance adjacent to the bodies of the lateral and third and the bottom of the fourth ventricles;
- middle cerebellar peduncles;
- white matter under the cerebral cortex;
- optic nerve;
- region of the cervical spinal cord;
- inferior border of the corpus callosum.
Multiple sclerosis on an MRI of the brain looks like round spots with a diameter of up to 2 centimeters, which can merge as the pathology develops. The shade of the changed areas depends on the stage of the disease and can be light, dark or identical to healthy tissues (without contrast it does not stand out).
“Dawson’s fingers” on MR tomograms in axial (left) and sagittal (right) projections - look like light oblong lesions on T1 VI
The classic sign of multiple sclerosis on MR images of the brain is linear plaques located perpendicular to the lateral ventricles. They are called “Dawson's fingers”.
In the spinal cord, foci of demyelination appear as elongated formations spreading from the center to the periphery, involving the dorsal horns in the pathological process.
The final stage of progression of lesions in multiple sclerosis are “black holes”, indicating the destruction of axons.
On an MRI scan of the brain in T1 VI, you can see long-term lesions of MS (indicated by arrows)