Arrhythmia is diagnosed when the regularity of contractions of the heart muscle is disrupted. The most common type of arrhythmia is tachycardia, which can be caused in the ventricles of the heart (ventricular arrhythmia) or in the atria (supraventricular arrhythmia). What are the symptoms of arrhythmia? What is the removal procedure? Arrhythmia is not an isolated disease. This term describes a heart rhythm disorder that can cause the heart to beat too fast, too slow, or irregularly. In other words, the heart rhythm may be disrupted. An abnormal heart rhythm can be a symptom of cardiovascular disease (coronary heart disease, heart valve disease, hypertension) or the effect of disorders such as hormonal or electrolyte imbalances. Therefore, the patient needs to find out the causes of the arrhythmia and, if they require treatment, undergo appropriate therapy.
How does arrhythmia occur?
To understand the mechanism of arrhythmia, it is necessary to recall basic information about the structure and function of the heart in the body. This organ consists of two atria and two ventricles, which contract and relax in a strictly defined rhythm. Thanks to these movements, blood is constantly pumped into every cell of the body, providing it with nutrients and oxygen. But what makes the heart beat so regularly? The heart is equipped with a natural "pacemaker", that is, the sinus node, located in the right atrium. It is thanks to him that the heart “beats” even when it is removed from the chest. The sinus node produces electrical impulses that move the entire muscle. The work of the heart is a series of complex bioelectrical processes that occur in each of its cells. Cardiac arrhythmias occur when abnormalities occur at some point in this complex process. The pulse source may fail or problems may arise at the conduction stage. In both cases, arrhythmia will occur.
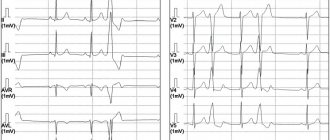
ECG No. 4
This is another ECG demonstrating a variant of supraventricular (also nodal) extrasystole. Only here it’s difficult to find the ‘P’ wave without knowing where to look. It may seem incredible, but it is here and seeing it once, you will be wary in the future.
The ectopic focus is located in the lower parts of the AV node, and possibly in the trunk of the His bundle (before the branching of the legs), since ventricular excitation (QRS) begins much earlier than retrograde excitation of the atria (negative P).
To close the topic, let’s look at the topic “Ventricular extrasytolia” and only then complete the task for self-control.
Types of arrhythmias
There are many types of arrhythmias, as well as divisions in medicine depending on the accepted classifications. The most common forms of cardiac arrhythmia include:
- sinus tachycardia,
- bradycardia,
- atrial fibrillation,
- ventricular fibrillation,
- additional supraventricular and ventricular contractions,
- tachycardia: supraventricular and ventricular.
Each of these disorders is actually a separate disease that has different causes and also requires different treatments.
Symptoms of arrhythmia
The most common symptoms of arrhythmia include:
- fast or irregular heartbeat,
- tachycardia,
- bradycardia,
- strong heartbeat,
- feeling of lumps in the chest,
- dyspnea,
- chest pain,
- heat,
- weakness,
- fainting.
Ventricular arrhythmia
Ventricular arrhythmia is one of the most common. Their classification includes: ventricular tachycardia, flutter and ventricular fibrillation and accelerated ventricular rhythm. The older the patient and the more damaged the heart, the more often they occur.
Ventricular Arrhythmia - Cardiac Factors Factors that cause or exacerbate ventricular arrhythmia can be classified as cardiac or non-cardiac. When this type of arrhythmia occurs, the following cardiac factors are especially likely:
- cardiac ischemia,
- cardiomyopathy,
- congenital long QT syndrome,
- Brugada syndrome,
- mitral valve prolapse.
Ventricular arrhythmia - non-cardiac factors Non-cardiac factors include disorders such as:
- polymyositis,
- sarcoidosis,
- amyloidosis,
- diseases of the nervous system,
- hormonal disorders,
- metabolic disorders,
- electrolyte disturbances.
In addition, the condition is affected by the use of stimulants (coffee, smoking, alcohol).
What are the symptoms of ventricular arrhythmia?
Symptoms of ventricular arrhythmia depend on the type of arrhythmia. In mild forms, patients may not experience arrhythmias. Palpitations may be accompanied by chest discomfort and anxiety. In complex disorders (ventricular tachycardia, ventricular flutter, ventricular fibrillation), shortness of breath, loss of consciousness and sudden cardiac arrest occur.
Medical reference books
Supraventricular rhythm disturbances
Supraventricular arrhythmias account for 4/5 of the total number of tachycardias and occupy an intermediate position between potentially life-threatening and benign cardiac arrhythmias. Supraventricular rhythm disturbances include sinus tachycardia, supraventricular extrasystoles and supraventricular paroxysmal tachycardia; This also includes atrial flutter and fibrillation. Normally, the sinus node generates impulses at a frequency of 60-90 beats per minute. Normal sinus rhythm is correct; as a variant of the norm, sinus arrhythmia can occur.
Sinus tachycardia
Sinus tachycardia is an increase in cardiac activity at rest over 100 beats per minute with the correct rhythm; during maximum physical activity in healthy young people it can reach 190-220 per minute. Mechanism. The development of arrhythmia is carried out due to increased automatism of the cells of the sinus node due to various influences of the autonomic (sympathetic and parasympathetic) nervous system. Increased automaticity function can cause increased tone of the sympathetic nervous system (excessive production of catecholamines or their toxic effect) or decreased tone of the vagus nerve (inhibition of the acetylcholine-cholinergic effect). Hypoxemia, acidosis, elevated body temperature, intoxication, and infections directly affect the cells of the sinus node. With sinus tachycardia, the conduction of excitation impulses through the atria and atrioventricular node occurs normally. The atria and ventricles are excited and contract in a coordinated manner, but shortened diastole creates unfavorable conditions for the functioning of the heart.
Clinic. Complaints are usually absent or minor - palpitations, a feeling of heaviness or pain in the cardiac region. Auscultation - correct rhythm with a heart rate of 100-150 beats per minute, with a gradual beginning and end. ECG diagnosis - all signs of sinus rhythm, P wave - positive in I, II, avF, negative in avR, biphasic in V1, V2.
Treatment. The main principle is the elimination of factors that provoke the development of tachycardia.
Atrial extrasystoles
Atrial extrasystoles (AEC) are premature, time-leading excitations and contractions of the entire heart or its parts, the impulse for which comes from various parts of the atria. They are caused by impulses arising in a focus with pathologically increased excitability, located outside the sinus node and belong to active ectopic rhythms.
Etiology. Approximately 1/3 of supraventricular ES is functional in nature and is observed in healthy people. It may be a manifestation of general neurosis with neurovegetative dystonia, or an expression of changes in corticovisceral regulation. Abuse of strong tea, coffee or alcohol, smoking, etc. have a great influence on their occurrence. In people with neurosis, the frequency of ES ranges from 7 to 14%. In each specific case, when determining the etiology of neurogenic ES, one should look for mental and physical fatigue, irregular sleep, sexual dysfunction, iatrogenics, domestic and professional psychotrauma. Various intrasecretory conditions and disorders (menopause, pregnancy, menstrual period, ovarian dysfunction) may play a role in the occurrence of ES in individuals without heart disease. Neuroreflex: the result of pathological irritation emanating from other internal organs through viscerocardial reflexes. PES of organic origin can cause processes in the lungs and mediastinum, pleural and pleurocardial adhesions, pneumosclerosis and cervical osteochondrosis. The appearance of atrial ES is facilitated by stagnation and stretching of the atria, for example, in patients with left or right ventricular failure or mitral stenosis. They often turn into atrial fibrillation in such situations.
Causes of atrial ES: - acute respiratory failure, chronic obstructive pulmonary diseases, hypoxia, - heart failure, - ischemic heart disease (angina), valvular heart disease, - use of digitalis, quinidine, procainamide (proarrhythmogenic effect is associated with prolongation of the absolute refractory period of the AV node), - excessive consumption of coffee, alcohol, nicotine , - stress, overwork, overeating.
Clinic: arrhythmic pulse, feeling of heartbeat, there may be no interruptions, after myocardial infarction - a reaction to pain. ECG diagnosis: The PES is characterized by a non-widened QRS complex, the P' wave may be biphasic, negative or absent. It can be recorded both before and after the QRS. Depending on the source of the ES, there may be no P' wave at all. With supraventricular ES, in most cases, an incomplete compensatory pause is observed, however, with stem ES, the compensatory pause is always complete.
Treatment – the underlying disease or known causes (exclude coffee, alcohol, smoking). For frequent atrial ES, if they trigger tachycardia, digitalis, verapamil, and beta-blockers (propranolol) are prescribed. Most often, specialized treatment is not required. The main indications for antiarrhythmic therapy are hemodynamic significance and subjective intolerance. In the second case, you should remember about tranquilizers and antidepressants. The selection of drug therapy is carried out individually. If the patient has concomitant ischemic heart disease, the prescription of antiarrhythmic drugs of all classes except the first is indicated.
Supraventricular paroxysmal tachycardias
Supraventricular paroxysmal tachycardias (SPT) are attacks of increased cardiac activity of a regular rhythm, with a heart rate of 140-220 beats per minute, with a sudden onset and end, as a result of activation of a center located outside the sinus node. The ectopic focus that provokes the development of SPT is located in the atria, AV node or common trunk of the His bundle. A special place is occupied by tachycardia against the background of WPW syndrome (presence of additional conduction pathways) - orthodromic and antidromic. Since re-entry includes the atrium, ventricles, AV node, and additional conduction tracts. In cardiological practice the most common are: · sinoatrial; · atrial; · atrioventricular nodal; · atrioventricular reciprocal tachycardia with the participation of additional pathways (WPW and Clerk-Levy-Critesco syndrome).
Mechanisms of development. The origin of paroxysmal tachycardias can be due to several mechanisms: due to impaired impulse formation and impaired impulse conduction. Impulse formation disorders include disorders of automaticity and triggered activity. Disturbances in the function of automaticity arise due to the presence of an ectopic focus in the heart muscle, and are the result of altered cellular metabolism due to local biochemical and electrolyte disorders. In the occurrence of an ectopic focus, a major role is played by the state of the central and autonomic nervous system, the presence of a focus with myocardial damage and local biochemical and electrolyte disturbances. There are two types of disorders - accelerated normal automatism and pathological automatism. The first causes the development of tachycardia in patients with a practically healthy heart. Damage to the myocardium due to inflammation, dystrophy or the development of scar fields leads to the appearance of lesions with pathological automatism. Among electrolyte disturbances, hypo- or hyperkalemia is of greatest importance. The appearance of early post-depolarizations is due to a slowdown in repolarization processes due to a weakening of the outgoing current of potassium ions in relation to the incoming currents of sodium and calcium. It is realized against the background of slowing repolarization and increasing the duration of the action potential. Predisposing factors are bradycardia, hypokalemia and hypomagnesemia. The appearance of late post-depolarizations is associated with cell overload with calcium ions. This is facilitated by the activation of the effect of catecholamines on the heart. Impaired impulse conduction is associated with the formation of a “closed loop” mechanism (re-entry). The development of re-entry is due to the circular movement of the excitation wave in the myocardium and fibers of the conduction system of the heart. There are anatomically determined development of tachycardia against the background of WPW syndrome (presence of additional pathways) and functionally determined - arrhythmias due to longitudinal dissociation of the AV connection, etc.
Etiology. The development of paroxysmal tachycardia can be observed in practically healthy people; it is caused by extracardiac causes. These include neurosis with lability of the autonomic nervous system, sympathicotonia, psycho-emotional effects, excessive consumption and increased sensitivity to substances that stimulate the nervous system (nicotine, coffee, tea, alcohol). The development of SPT can be a manifestation of viscerocardial reflexes and is associated with pathology of adjacent organs - gastric ulcer, acute and chronic pancreatitis, cholelithiasis, nephrolithiasis, colitis, constipation, diseases of the mediastinal organs, spine, organic diseases of the nervous system, etc. Also predisposing factors can be hormonal disorders - pregnancy, puberty, menstruation, menopause, thyrotoxicosis, ovarian dysfunction, pituitary diseases and allergic-anaphylactic reactions. Genetically determined causes are tachycardia against the background of the existence of additional conduction pathways. The cause of the development of tachycardia may be intoxication with digitalis drugs, congenital or long QT syndrome. Of the organic diseases of the heart muscle, SPT develops against the background of rheumatic valve defects, coronary heart disease, and hypertensive heart.
Clinical picture. Subjectively, patients feel a sudden strong palpitation with an initial beat (push) in the heart area with the same sudden ending with a feeling of cardiac arrest. The attack is described as fluttering or “jumping” in the heart area, a feeling of heaviness in the heart area, pulsation and a feeling of tension in the neck and head, general weakness, fear, excitement, tension, dizziness. An attack of paroxysmal tachycardia may be accompanied by increased sweating, increased peristalsis, flatulence, nausea and vomiting. A very important diagnostic sign is frequent and copious urination for several hours; a large amount of light-colored urine with low specific gravity is released. This is the so-called urina spastica, associated with the relaxation of the sphincter of the bladder, which is spasmed during an attack. The end of the attack, often in the form of a jolt and “freezing” in the heart area, is accompanied by a feeling of relief, normalization of cardiac activity and breathing. Clinically, during an attack of paroxysmal tachycardia, patients experience pallor of the skin and visible mucous membranes. The neck veins swell and pulsate synchronously with the arterial pulse. Breathing is rapid. The pulse is rhythmic, sharply increased, difficult to count, and weak in filling. On auscultation, a pendulum-like rhythm is heard, with a heart rate from 150 to 220 per minute. Blood pressure is normal or low. As a rule, attacks occur without a drop in hemodynamics, patients are conscious and adequate, although severe weakness develops. Cardiogenic shock rarely develops with a severe general condition, impaired consciousness, a drop in blood pressure and manifestations of the central and autonomic nervous systems, decompensation and shock.
ECG diagnostics. The rhythm is correct, RR intervals are greatly shortened, but equal to each other, permissible fluctuations are 0.06 s. The constancy of the duration of RR intervals is one of the differential diagnostic features. Depending on the location of the ectopic focus, the P' wave can be positive, biphasic or negative. Each P' wave is followed by a ventricular complex. Often the P' wave merges with the preceding T wave and is not distinguishable on the ECG. The QRS complex is not widened, not deformed, the ST segment and T wave are not changed, and ST segment depression is often observed against the background of high heart rate. Sometimes frequency-dependent bundle branch blocks may occur with all the signs of blocked branches (widening of the QRS complex by more than 0.12 s, discordant changes in the final part of the ventricular complex - the ST segment and the T wave are directed in the direction opposite to the main wave of the QRS complex). Frequent attacks of paroxysmal tachycardia can cause the development of tachycardic cardiomyopathy, with dilation of the heart cavities and subsequent development of heart failure. During an attack of paroxysmal tachycardia with a high heart rate, coronary circulation is significantly disrupted, which can lead to the development of myocardial infarction in patients with coronary heart disease. Sometimes an attack of paroxysmal tachycardia leads to thromboembolic complications. Dynamic cerebrovascular accidents and thromboembolism of peripheral vessels may develop. Often, patients, especially those suffering from severe coronary atherosclerosis, develop post-tachycardia syndrome, which is caused by impaired metabolic processes in the heart muscle and myocardial ischemia. On the electrocardiogram after an attack, ischemic changes in the terminal part of the ventricular complex appear in the sinus complexes in the form of negative T waves, depression of the ST segment, which, the more pronounced the organic changes in the heart muscle, the longer they persist on the ECG.
Treatment. When an attack of paroxysmal tachycardia develops, emergency management of patients includes performing so-called vagal tests, influencing nervous regulation by stimulating the branches of the vagus nerve. These techniques include: the Chermak-Goering test, the Aschner-Danyini test, the Valsalva test. The Chermak-Hering test is performed by applying mechanical pressure to the area of the carotid sinus (carotid sinus), located at the bifurcation of the common carotid artery. The test is carried out with the patient lying on his back. Press on only one side on the inner surface of the upper third of the sternocleidomastoid muscle at the level of the upper edge of the thyroid cartilage. The area of the carotid sinus is gradually pressed with the thumb of the right hand, towards the spinal column. The duration of pressure is no more than 30 seconds, under constant monitoring of the pulse. Typically, pressing on the right carotid node is more effective. As soon as the attack has stopped, pressure on the carotid artery must be stopped immediately due to the risk of prolonged ventricular asystole. This test is contraindicated in elderly people with severe cerebral atherosclerosis, as well as in the late stages of hypertension. To relieve an attack of paroxysmal tachycardia, the Aschner-Danyini test is used. Apply moderate and even pressure on both eyeballs. This test is also performed only in a horizontal position of the patient. The tips of the thumbs apply pressure for no more than 30 seconds on the patient’s closed eyes, directly above the upper supraorbital arches. For eye diseases and severe myopia, this test is contraindicated. The next test used to relieve an attack of paroxysmal tachycardia is the Valsalva maneuver. This is a mechanical technique - straining while taking a deep breath and pinching the nose, artificially inducing vomiting, coughing, strong pressure on the upper abdomen, bending and pressing the legs to the stomach, cold rubbing of the skin, etc. In terms of effectiveness, the Valsalva maneuver is the most effective. The effectiveness of stopping tachycardia is 70-80%. The most effective drug for relieving SPT is adenosine. Adenosine is administered intravenously in a stream over 1-3 s. at an initial dose of 6 mg; if there is no effect, it is advisable to administer a second dose - 12 mg, if necessary, after 1-2 minutes - another 12 mg. Transient side effects include facial flushing, chest discomfort, difficulty breathing, and AV block. If there is no effect, verapamil is administered at an initial dose of 2.5-5 mg IV, then this drug can be used orally at a daily dose of 240 mg/day. The use of adenosine should be avoided in patients with bronchial asthma, vasospastic form of angina, in combination with beta-blockers. Verapamil or diltiazem should be used instead. Digoxin and propranolol, esmolol, and sedatives can also be used in the treatment of SPT, but it should be remembered that verapamil and digoxin cannot be used in the treatment of tachycardia of unknown etiology with wide QRS complexes.
In WPW syndrome, the following are distinguished: · paroxysmal reciprocal AV-orthodromic tachycardia (anterograde impulse is conducted through the AV node, retrograde – through the AP node), · paroxysmal reciprocal AV-antidromic tachycardia (anterograde – through the AP node, retrograde – through the AV node).
ECG criteria for orthodromic paroxysmal tachycardia in WPW syndrome: heart rate - 170-220 beats per minute, rhythm - correct, RR intervals - the same. Negative P waves are often not visualized because they overlap the QRS complex. The QRS complexes are not widened or deformed, their duration does not exceed 0.12 s. (impulses enter the ventricles through the AV connection).
ECG criteria for antidromic paroxysmal tachycardia in WPW syndrome: heart rate - 170-220 beats per minute, rhythm - correct, RR intervals - the same. P waves are not visualized because they overlap the QRS complex; sometimes a negative P wave is located behind the QRS complex. The QRS complexes are widened, lasting more than 0.1 s, and not deformed (a reflection of the maximum pre-excitation of the ventricles, when they are excited non-simultaneously).
Treatment of orthodromic SPT with narrow QRS complexes: vagal tests, if ineffective - ATP 10-30 mg or adenosine 6-12 mg IV bolus over 1-3 s. Verapamil or diltiazem can be used in optimal doses. If possible, insert a probe electrode into the esophagus to the level of the right atrium and perform ultra-frequent stimulation with a current of 10-30 mA, with the maximum possible duration of the stimulus. If ineffective - electrical cardioversion sequentially 150-200-270 kJ.
Treatment of antidromic SPT with wide QRS complexes: ATP, adenosine and verapamil is dangerous to administer, as it can provoke the development of ventricular fibrillation. First-line drugs are procainamide 0.5-1.0 g IV in a bolus, disopyramide 150 mg IV in a bolus, or sotalol 40 mg IV in a bolus or amiodarone 300-450 mg IV in a bolus. If ineffective, use electrical cardioversion. Planned treatment of reciprocal tachycardias is radiofrequency catheter ablation (modification) of the corresponding conductive structures of the heart. It is a first-line treatment and is offered to all patients with supraventricular reentrant tachycardia, which is associated with its safety, favorable cost-effectiveness ratio and the ability to eliminate the background mechanism of arrhythmia with minimal risk of complications. In case of AV nodal tachycardia, exposure in the area of the AV junction is preferable (less risk of AV block) - ablation of slow pathways. With WPW – ablation of additional pathways. Preventive antiarrhythmic therapy for reciprocal tachycardia is carried out only if there are contraindications or the patient refuses radiofrequency ablation.
What tests should be taken for ventricular arrhythmia?
To correctly identify ventricular arrhythmia and accurately differentiate the type of ventricular arrhythmia, it is necessary to perform an ECG. If arrhythmia occurs intermittently, perform a Holter test (24-hour ECG recording). You can also monitor your heart rate for longer, such as three days or even 2-3 weeks. In this case, it is necessary to wear an Event-Holter device, which the patient activates only when symptoms appear, such as:
- cardiopalmus,
- deterioration of health,
- dizziness.
An invasive electrophysiological study is performed when the site of ventricular arrhythmia is identified and an attempt is made to destroy the arrhythmogenic focus. The following methods are used in the treatment of ventricular arrhythmias:
- antiarrhythmic drugs,
- percutaneous high-frequency ablation,
- implantation of a cardioverter-defibrillator.
The doctor decides what treatment to take when he determines what type of ventricular arrhythmia the patient has.
Diagnostics
If you suspect a pathology, you should immediately consult a doctor. He can make an accurate diagnosis.
Diagnostics is carried out comprehensively and includes:
- History taking and examination.
- Studies of urine and blood parameters.
- Carrying out immunological and rheumatological tests.
- ECG, ultrasound of the heart, Holter monitoring.
- Coronary angiographic study.
Supraventricular arrhythmia
Atrial fibrillation and atrial flutter is one of the types of supraventricular arrhythmia. The most common symptoms include rapid heartbeat, shortness of breath, and even fainting. The best results are achieved by combining pharmacological treatment with diagnostic procedures. Supraventricular cardiac rhythm disturbances are caused by electrical impulses originating in the sinus node or atrioventricular focus.
Supraventricular arrhythmia - types
Supraventricular arrhythmias include:
- additional, single stimulation,
- supraventricular tachycardia,
- pre-excitation syndromes,
- atrial tachycardia,
- atrial fibrillation,
- atrial flutter,
- sinus tachyarrhythmias.
Supraventricular arrhythmia - symptoms
Each of the arrhythmias listed above has different causes and symptoms. Each of them is treated differently. First of all, it is necessary to determine what diseases cause supraventricular arrhythmia, what symptoms accompany it, what is the patient's prognosis and how to treat it. Symptoms that are typical of supraventricular arrhythmia include:
- cardiopalmus,
- fatigue,
- dyspnea,
- fainting,
- dizziness,
- chest discomfort.
There are often no symptoms with supraventricular accessory beats.
Treatment of supraventricular arrhythmias
First of all, it is important to have a detailed history of not only heart disease, but also general, rheumatological, metabolic and endocrine diseases. This usually starts with non-invasive tests such as: morphology, ECG, cardiac ECHO and Holter study. If necessary, invasive and complex tests such as electrophysiological studies are performed. Supraventricular arrhythmias are usually treated with medications. When this doesn't work, you can introduce ablation, for example. These two treatments can also effectively complement each other.
The article is for informational purposes only, self-medication is not acceptable. Be sure to consult with your healthcare provider.
Causes of the disease
Extrasystolic arrhythmia develops for a number of reasons.
Among them:
- IHD;
- heart failure;
- acquired or congenital heart defects;
- myocarditis;
- cardiomyopathy.
The following factors can provoke the development of pathology:
- Taking certain medications (glycosides, diuretics and sympathomimetics). Thus, diuretics help remove potassium from the body, which is necessary for the proper functioning of the heart muscle. Glycosides can provoke tachycardia and atrial fibrillation. Sympathomimetics not only increase blood pressure, but also lead to stimulation of the central nervous system.
- Diabetes.
- Abuse of nicotine and alcohol.
- Pathologies of the adrenal glands.
- Hyperfunction of the thyroid gland.
- Overvoltage and stress.
Often the disease actively manifests itself in pregnant women. This is due to the fact that there is a double load on the heart and circulatory system. At the same time, hormonal changes occur. Arrhythmia does not pose a danger to mother and child. After childbirth it is easily eliminated.