Infectious mononucleosis in children is a viral disease that mainly affects children from 2–3 years of age to adolescence. The disease also occurs in adults. In young children - under two years of age - it is registered very rarely, and, which is atypical, it occurs more easily than in older children.
The disease is transmitted through household contact and airborne droplets; the incidence is sporadic - there are no epidemics. The incubation period can vary from several days to two months. The disease affects lymphoid tissue - lymph nodes, tonsils of the nasopharynx, spleen, and liver damage may also occur. Among the common symptoms, catarrhal phenomena are sometimes encountered, but more often - weakness, dizziness, nasal congestion, swelling of the tonsils and enlargement of adenoid tissue in the nasopharynx - the child snores in his sleep, which is unusual for children.
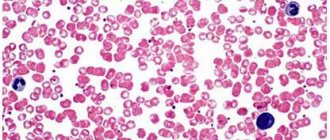
Mononucleosis in children causes enlargement of the lymph nodes, most often the cervical ones, but others may also enlarge. The most characteristic feature of mononucleosis, according to which the final diagnosis is made, is an unusual blood picture in which special large cells appear - these leukocytes affected by the virus are called atypical mononuclear cells, and an experienced laboratory doctor will not confuse them with anything. In controversial cases, you need to consult a hematologist.
The disease lasts 2-3 weeks and usually ends with recovery; sometimes bacterial complications can occur - otitis, sore throat, pneumonia, which are treated standardly - with antibiotics and symptomatic remedies.
Mononucleosis itself in children, like all viral diseases, has no specific treatment; vitamins, plenty of fluids, bed rest are used, and for headaches and fever - antipyretics.
Quarantine for cases of mononucleosis in a children's group is not declared. Due to the fact that the disease affects the components of “white blood” - leukocytes - it would be useful to be observed for some time by a pediatric hematologist, especially in cases where the blood picture does not return to normal for a long time.
After the cessation of a clinically significant disease, we must remember that the immune system was affected, and it does not recover overnight. Children are exempted from preventive vaccinations for a year and physical activity is limited. Such children do not tolerate exposure to the sun very well; sunbathing in the coming summer must be done very carefully. Otherwise, the disease is benign and can be completely cured.
Detailed description of the study
Mononuclear cells are large mononuclear cells of the lymphoid series, similar to normal blood cells - monocytes. They belong to the group of phagocytes and are responsible for the body’s defenses - they capture and destroy viruses and pathogenic bacteria, as a result of which they become large. Normally, the level of mononuclear cells in the blood does not exceed 1%.
An increase in the level of atypical mononuclear cells to 10% signals an acute viral infection. An increase in the rate of over 10% is the main diagnostic sign of infectious mononucleosis.
Infectious mononucleosis ((EBV, human herpes virus type 4, HHV-4) and EBV infection) is an acute disease caused by the Epstein-Barr virus. The infection is transmitted by airborne droplets.
The disease is manifested by an increase in body temperature and enlargement of the lymph nodes (the cervical nodes are most often affected, especially their posterior group). They become noticeable to the eye, dense when palpated, but not fused to each other and the surrounding tissues. The skin over them swells, but does not change color. The spleen and liver are often involved in the infectious process. They increase in size, the patient may complain of heaviness and discomfort in the right hypochondrium. Another very important symptom is fever, sore throat, as well as severe pharyngitis and tonsillitis. Symptoms of infectious mononucleosis appear in 35-50% of infected people. During the prodromal period, the infection is manifested by muscle pain, fatigue, and general malaise.
Determining the percentage of mononuclear cells in the blood helps confirm the diagnosis.
Almost always, mononuclear cells in a blood test are of a secondary nature, therefore, against the background of the above symptoms, signs characteristic of the provoking disease will develop.
Epstein-Barr viral infection in children: modern approaches to diagnosis and treatment
Epstein-Barr virus infection (EBVI) is one of the most common human infectious diseases. Antibodies (Abs) to the Epstein-Barr virus (EBV) are detected in 60% of children in the first two years of life and in 80–100% of adults [3, 13]. The incidence of acute form of EBVI (EBVI) in different regions of the world ranges from 40 to 80 cases per 100 thousand population [2]. The chronic form of EBVI (CEBVI) develops in 15–25% of individuals after EBVI [1, 5, 15]. The role of EBV in the development of malignant neoplasms, autoimmune diseases and chronic fatigue syndrome has been established [3, 5, 14, 15]. All this indicates the relevance of the problem of EBVI.
EBV, discovered in 1964 by M. Epstein and Y. Barr, belongs to the γ-herpes viruses [3]. EBV has 3 antigens: capsid (VCA), early (EA) and nuclear (EBNA). The uniqueness of the pathological process in EBVI is determined by the ability of EBV to transform B-lymphocytes, lifelong persistence in the human body, induction of a secondary immunodeficiency state (IDS), autoimmune reactions, and malignant tumors [1, 3, 5, 12].
The source of EBV infection is patients with manifest and asymptomatic forms. 70–90% of people who have had EEBVI shed the virus in the next 1–18 months. Routes of transmission of EBV: airborne, household contact, parenteral, sexual, vertical. OEBVI is characterized by epidemic rises once every 6–7 years, and is more often registered at the age of 1 to 5 years, in organized groups [4, 7, 9].
The entrance gate for EBV is the mucous membrane of the upper respiratory tract: the virus penetrates the lymphoid tissue, infects B-lymphocytes, polyclonal activation of B-lymphocytes develops, dissemination of the pathogen within B-lymphocytes, the synthesis of antibodies (Ab) in response to antigenic stimulation is reduced. EBV primarily affects lymphoid organs (tonsils, liver, spleen).
The next stage is the formation of a clone of sensitized cytotoxic CD8 cells, the sequential synthesis of Abs to the VCA, EA and EBNA antigens of the virus. Due to disruption of the immune response and functional activity of innate resistance factors (neutrophils, macrophages, NK cells, interferon system), secondary IDS is formed [2–4, 12].
The immune status of 109 patients with OEBVI aged 5 to 14 years in our work revealed signs of activation of the T-cell component of the immune system - an increase in the number of T-lymphocytes (CD3), cytotoxic T-lymphocytes (CD8), cells with markers of late activation (HLA- DR); polyclonal activation of B lymphocytes - an increase in the number of CD20 cells, immunoglobulins (Ig) IgA, IgM, IgG, circulating immune complexes (CIC). Signs of suppression of the immune system were found: normal levels of T-helper cells (CD4), a decrease in the immunoregulatory index CD4/CD8, the number of natural killer NK cells (CD16), and an increase in the readiness of immunocompetent cells for apoptosis (CD95). Activation of oxygen-dependent metabolism of neutrophils and a reduction in its adaptive capabilities were observed.
In a third of the examined children (33.9%), EEBVI occurred in the form of a mixed infection with cytomegalovirus (CMV), herpes simplex viruses types 1 and 2 (HSV-1, HSV-2). During bacteriological examination of oropharyngeal smears, Streptococcus (S.) viridans was isolated in 41.3% of patients, Candida albicans in 11.9%, Staphilococcus (Staph.) epidermidis in 8.2%, S. pyogenes, in 2.7% - Klebsiella (Kl.) pneumoniae, in 41.3% - an association of bacteria. 43.1% of patients had serological markers of an active form of chlamydial infection, and 30.3% had mycoplasmosis.
The following outcomes of EBVI are possible: latent infection, EBVI, IDS, cancer, autoimmune diseases, chronic fatigue syndrome [5, 8, 10, 11]. The transition to CHEBVI is associated with a complex of unfavorable factors in the ante-, intra- and postnatal periods, disruption of neuroimmune-endocrine regulation, and genetic predisposition.
Our examination of 60 children aged 5 to 14 years with CEBVI showed that in this group 86.7% of mothers had a burdened obstetric history; In 83.3% of children, perinatal and postnatal pathologies of the central nervous system, ENT organs, etc. were detected.
The immune status of patients with CHEBVI revealed an increase in the content of interleukin-1 antagonist (IL-1RA), insufficient activation of immunocompetent cells (decrease in HLA-DR) and an increase in their readiness for apoptosis (increase in CD95). There was a disturbance in the functional activity of type 1 T helper cells (Th1) (decreased levels of interferon γ (IFN γ)); decrease in the total pool of T cells (CD3), the number of lymphocytes with receptors for IL-2 (CD25) and NK cells (CD16); the content of cytotoxic CD8 lymphocytes was increased. The persistence of EBV replication markers for a long time in this group indicated a violation of virus elimination; At the same time, an increase in the functional activity of Th2, polyclonal activation of B-lymphocytes (CD20), an increase in the content of IgA, IgM, IgG, CEC, a decrease in the level of neutrophil chemotactic factor (IL-8), and a change in their metabolism were noted.
Immune status disorders led to the activation of opportunistic microflora, viral and fungal infections. In the microbial spectrum of the oropharyngeal mucosa of patients with CHEBVI, S. Viridans (30%), Candida albicans (28.3%), Staph. Epidermidis (25%), S. Pyogenes (20%), Kl. Pneumoniae (8.4%), bacterial association (41.7%); 28.3% had serological markers of the active form of chlamydia, 26.7% had mycoplasmosis. In 90% of patients, the disease occurred in the form of a mixed infection involving herpes viruses: EBV + CMV, EBV + HSV-1, HSV-2.
Classification . There is no generally accepted classification of the disease; We recommend using the working classification of EBVI that we have developed.
- By period of occurrence: congenital, acquired.
- Form: typical (infectious mononucleosis), atypical: erased, asymptomatic, visceral.
- By severity: light, medium, heavy.
- According to the course: acute, protracted, chronic.
- By phase: active, inactive.
- Complications: hepatitis, splenic rupture, meningoencephalitis, polyradiculoneuropathy, myocarditis, sinusitis, otitis, hemolytic anemia, thrombocytopenia, neutropenia, pancreatitis, etc.
- Mixed infection.
Examples of diagnosis:
- Main: Acquired EBVI, typical severe form (infectious mononucleosis), acute course, active phase. Osl.: Acute hepatitis.
- Main: Acquired EBVI, visceral form (meningoencephalitis, hepatitis, nephritis), severe chronic course, active phase. Osl.: acute hepatic-renal failure. Associated with: Respiratory chlamydia (rhinopharyngitis, bronchitis, pneumonia).
The clinical picture of acute EBVI was first described by N. F. Filatov (1885) and E. Pfeiffer (1889). The incubation period lasts from 4 days to 7 weeks. A complete symptom complex is formed by 4–10 days of illness [4, 7].
We examined 109 children with OEBVI. In most patients, the disease begins acutely, with an increase in body temperature and the appearance of symptoms of intoxication; less often, a gradual onset is observed: for several days there is malaise, weakness, lethargy, and loss of appetite. Body temperature is subfebrile or normal. By days 2–4 of illness, the temperature reaches 39–40 °C; fever and symptoms of intoxication may persist for 2–3 weeks or more.
Generalized lymphadenopathy is a pathognomonic symptom of EBVI and from the first days of the disease manifests itself in the form of systemic damage to 5–6 groups of lymph nodes (LNs), with a predominant increase of up to 1–3 cm in diameter of the anterior and posterior cervical, submandibular LNs. LNs are slightly painful on palpation, are not fused to each other and the surrounding tissues, and are arranged in the form of a “chain” or “package”; visible when turning the head, giving the neck a “scalloped” outline. Sometimes there is a pastiness of the soft tissues over the enlarged lymph nodes.
Tonsillitis is the most common and early symptom of OEBVI, accompanied by enlargement of the tonsils to degree II-III. The lacunar pattern is emphasized due to infiltration of tonsil tissue or smoothed due to lymphostasis. On the tonsils there are plaques of yellowish-white or dirty gray color in the form of islands and stripes. They come from gaps, have a rough surface (reminiscent of lace), are easily removed without bleeding, rubbed, and do not sink in water. There is a discrepancy between the size of plaque and the degree of enlargement of regional lymph nodes. With the fibrinous-necrotic nature of the plaques, if they spread beyond the tonsils, a differential diagnosis with diphtheria is necessary. Plaques on the tonsils usually disappear after 5–10 days.
Signs of adenoiditis are found in the vast majority of patients. There is nasal congestion, difficulty in nasal breathing, snoring with an open mouth, especially during sleep. The patient’s face takes on an “adenoid” appearance: puffiness, pastiness of the eyelids, bridge of the nose, breathing through an open mouth, dry lips.
Hepatomegaly can be detected from the first days of the disease, but is more often detected in the second week. Normalization of liver size occurs within six months. In 15–20% of patients, hepatitis develops as a complication.
Splenomegaly is a late symptom and occurs in most patients. Normalization of the size of the spleen occurs within 1–3 weeks.
Exanthema with OEBVI appears on the 3rd–14th days of the disease, has a polymorphic character - spotted, papular, maculopapular, roseolous, punctate, hemorrhagic. There is no specific localization. The rash lasts for 4–10 days, sometimes leaving pigmentation. In children treated with ampicillin or amoxicillin, the rash appears more often (90–100%).
Hematological changes include leukocytosis (10–30 x 109/l), neutropenia with a band shift to the left, an increase in the number of lymphocytes, monocytes, and atypical mononuclear cells up to 50–80%, an increase in ESR up to 20–30 mm/hour. A characteristic hematological sign is atypical mononuclear cells in an amount of 10–50%: they appear by the end of the first week of the disease and persist for 1–3 weeks.
Chronic EBVI is the outcome of EBVI or develops as a primary chronic form [2, 5, 8, 10, 11, 15]. We examined 60 children with CHEBVI, the clinical picture of which included chronic mononucleosis-like syndrome and multiple organ pathology. All patients were found to have lymphoproliferative syndrome (generalized lymphadenopathy, hypertrophy of the palatine and pharyngeal tonsils, enlarged liver and spleen) and signs of chronic intoxication (prolonged low-grade fever, weakness, loss of appetite, etc.). Due to the development of IDS, acute infections of the respiratory tract and ENT organs were observed with exacerbations up to 6–11 times a year: nasopharyngitis (28.3%), pharyngotonsillitis (91.7%), adenoiditis (56.7%), otitis (11. 7%), sinusitis (20%), laryngotracheitis (18.3%), bronchitis (38.3%), pneumonia (25%). Noteworthy was the high frequency of multiple organ pathologies caused by long-term replication of EBV, secondary IDS, and autoimmune reactions (CNS pathology; chronic gastritis, biliary dyskinesia; cardiac syndrome, arthralgia).
In recent years, congenital EBVI has been described. It has been established that its risk with primary EBVI during pregnancy is 67%, with reactivation - 22%. The clinical picture of congenital EBVI is similar to that of CMVI.
The role of EBV in the development of cancer and paraneoplastic processes has been established - Burkett's lymphoma, nasopharyngeal carcinoma, lymphogranulomatosis, tumors of the stomach, intestines, salivary glands, uterus, leukoplakia of the tongue and oral mucosa, as well as a number of autoimmune diseases - systemic lupus erythematosus, rheumatoid arthritis, syndrome Sjögren, lymphoid interstitial pneumonitis, chronic hepatitis, uveitis, etc. [3, 5, 14, 15]. EBV, along with human herpes viruses types 6 and 7, is the etiological factor of chronic fatigue syndrome and the most common cause (15%) of the development of prolonged fever of unknown origin.
Diagnosis of EBVI is based on taking into account risk groups, leading clinical syndromes and laboratory data [8–11]. Risk groups in the mother include a burdened medical history, markers of herpes viral infections, etc., in the child - perinatal damage to the central nervous system, allergic phenotype, IDS, markers of herpes viral infections, etc. The leading clinical syndromes of EBVI are mononucleosis-like, general infectious syndromes, exanthema, syndrome of multiple organ pathology.
The mandatory standard for diagnosing EBVI includes a clinical blood test, a general urine test, a biochemical blood test, a bacteriological examination of the mucus of the oropharynx and nose, serological markers of EBV, other herpes viruses, chlamydia, mycoplasmas, ultrasound of the abdominal organs, consultation with an ENT doctor, if indicated. - radiography of the paranasal sinuses, chest organs, ECG. Additional diagnostic standard (in a specialized treatment and prophylactic institution): markers of EBV, other herpes viruses, chlamydia, mycoplasmas using polymerase chain reaction (PCR), second-level immunogram, consultation with an immunologist, if indicated - coagulogram, morphological picture of sternal puncture, consultation with a hematologist , oncologist.
The method of enzyme-linked immunosorbent assay (ELISA) is used to determine Abs to EBV antigens, which allows for laboratory diagnosis of EBV and determining the period of the infectious process.
IgM class antibodies to VCA appear simultaneously with the clinical manifestations of EBV, persist for 2–3 months, and are re-synthesized during EBV reactivation. Long-term persistence of high titers of these Abs is characteristic of CHEBVI, EBV-induced tumors, autoimmune diseases, and IDS.
IgG class antibodies to EA reach a high titer at 3–4 weeks of OEBVI and disappear after 2–6 months. They appear during reactivation and are absent in the atypical form of EBVI. High titers of Abs of this class are detected in cases of CHEBVI, EBV-induced oncological and autoimmune diseases, and IDS.
IgG antibodies to EBNA appear 1–6 months after the primary infection. Then their titer decreases and persists throughout life. When EBVI is reactivated, their titer increases again.
The study of IgG class Ab avidity (the strength of antigen binding to Ab) is of great importance. During primary infection, Abs with low avidity (avidity index (AI) less than 30%) are first synthesized. The late stage of primary infection is characterized by Abs with medium avidity (IA - 30–49%). High-avidity Abs (IA - more than 50%) are formed 1–7 months after EBV infection.
Serological markers of the active phase of EBVI are IgM Abs to VCA and IgG Abs to EA, low and medium avidity IgG Abs to markers of the inactive phase, IgG Abs to EBNA.
The material for PCR is blood, cerebrospinal fluid, saliva, smears from the oropharyngeal mucosa, organ biopsies, etc. The sensitivity of PCR for EBVI (70–75%) is lower than for other herpesvirus infections (95–100%). This is due to the appearance of EBV in biological fluids only during immune-mediated lysis of infected B lymphocytes.
Treatment. The principles of treatment for EBVI are complex, the use of etiotropic drugs, continuity, duration and continuity of treatment measures at the stages “hospital → clinic → rehabilitation center”, monitoring of clinical and laboratory parameters.
Based on the experience of treating 169 children with EBVI, we have developed a standard of treatment for this disease.
Basic therapy: protective regime; therapeutic nutrition; antiviral drugs: virocidal drugs - inosine pranobex (Isoprinosine), abnormal nucleosides (Valtrex, Acyclovir), Arbidol; IFN preparations - recombinant IFN α-2β (Viferon), Kipferon, Reaferon-ES-Lipint, interferons for intramuscular administration (Reaferon-EC, Realdiron, Intron A, Roferon A, etc.); IFN inducers - Amiksin, ultra-low doses of antibodies to γ-IFN (Anaferon), Cycloferon, Neovir. According to indications: local antibacterial drugs (Bioparox, Lizobakt, Stopangin, etc.); systemic antibacterial drugs (cephalosporins, macrolides, carbapenems); immunoglobulins for intravenous administration (Immunovenin, Gabriglobin, Intraglobin, Pentaglobin, etc.); vitamin and mineral complexes - Multi-tabs, Vibovit, Sanasol, Kinder Biovital gel, etc.
Intensification of basic therapy according to indications:
Immunocorrective therapy under the control of an immunogram - immunomodulators (Polyoxidonium, Likopid, Ribomunil, IRS-19, Imudon, Derinat, etc.), cytokines (Roncoleukin, Leukinferon); probiotics (Bifiform, Acipol, etc.); metabolic rehabilitation drugs (Actovegin, Solcoseryl, Elcar, etc.); enterosorbents (Smecta, Filtrum, Enterosgel, Polyphepan, etc.); second generation antihistamines (Claritin, Zyrtec, Fenistil, etc.); hepatoprotectors (Hofitol, Galstena, etc.); glucocorticosteroids (prednisolone, dexamethasone); protease inhibitors (Kontrikal, Gordox); neuro- and angioprotectors (Encephabol, Gliatilin, Instenon, etc.); “cardiotropic” drugs (Riboxin, Cocarboxylase, Cytochrome C, etc.); homeopathic and antihomotoxic remedies (Ocillococcinum, Aflubin, Lymphomyosot, Tonzilla compositum, etc.); non-drug methods (laser therapy, magnetic therapy, acupuncture, massage, physical therapy, etc.)
Symptomatic therapy.
For fever - antipyretic drugs (paracetamol, ibuprofen, etc.); if there is difficulty in nasal breathing - nasal medications (Isofra, Polydexa, Nazivin, Vibrocil, Adrianol, etc.); for a dry cough - antitussive drugs (Glauvent, Libexin), for a wet cough - expectorants and mucolytic drugs (AmbroHEXAL, bromhexine, acetylcysteine, etc.).
| Rice. 1. Scheme of complex therapy for Epstein-Barr viral infection in children |
For several years, for the treatment of EBVI, we have successfully used a combination stepwise etiotropic therapy regimen, which includes inosine pranobex (Isoprinosine) and recombinant interferon α-2β (Viferon) (Fig. 1, 2). Inosine pranobex (Isoprinosine) suppresses the synthesis of viral proteins and inhibits the replication of a wide range of DNA and RNA viruses, including EBV [3]. The drug has immunocorrective activity - modulates the immune response according to the cellular type, stimulates the production of Abs, cytokines, IFN, increases the functional activity of macrophages, neutrophils and NK cells; protects affected cells from post-viral decrease in protein synthesis. Inosine pranobex (Isoprinosine) was prescribed at 50–100 mg/kg/day orally in 3–4 divided doses. Three courses of treatment were carried out for 10 days with an interval of 10 days. Recombinant IFN α-2β (Viferon) inhibits viral replication by activating endonuclease and destroying viral messenger RNA [6]. The drug modulates the immune response, promotes the differentiation of B-lymphocytes, stimulates the production of cytokines, and increases the functional activity of macrophages, neutrophils and NK cells. The natural antioxidants it contains (vitamins E and C) stabilize cell membranes. The drug was prescribed according to a prolonged regimen (V.V. Malinovskoy et al., 2006) [6].
The effectiveness of etiotropic therapy for OEBVI was assessed in two groups of patients. Patients of the 1st group (52 people) received inosine pranobex (Isoprinosine) in combination with recombinant IFN α-2β (Viferon), patients of the 2nd group (57 children) received monotherapy with recombinant IFN α-2β (Viferon). Clinical and serological parameters before the start of treatment and after 3 months of therapy are presented in Table. 1. Over time, patients in both groups showed a significant decrease in symptoms such as generalized lymphadenopathy, tonsillitis, adenoiditis, hepatomegaly and splenomegaly. However, against the background of combination therapy, the positive dynamics of clinical indicators were more significant; acute respiratory infections (ARI) only in 19.2% of patients in group 1 and in 40.3% of patients in group 2 (p < 0.05). During combination therapy, a more rapid disappearance of serological replication markers was observed.
| Rice. 2. Mechanisms of etiopathogenetic action of the combination of inosine pranobex (Isoprinosine) and recombinant interferon α-βb (Viferon) in Epstein-Barr viral infection in children |
Combination therapy for OEBVI contributed to the modulation of the immune response by cell type (increase in CD3-, CD4-, CD8-, CD16- and HLA-DRT lymphocytes). The readiness of immunocompetent cells for apoptosis (CD95) decreased. There was stimulation of IgA production, switching of Ab synthesis from IgM to IgG, a decrease in CEC content, and improved neutrophil metabolic rates.
The effectiveness of etiotropic therapy was studied in 60 patients with CHEBVI. Patients of group 1 (30 children) received inosine pranobex (Isoprinosine) and recombinant IFN α-2β (Viferon), group 2 (30 people) received monotherapy with recombinant IFN α-2β (Viferon). Regardless of the treatment regimen, 3 months after the start of therapy, there was a significant decrease in the frequency of generalized lymphadenopathy, hypertrophy of the palatine and pharyngeal tonsils, splenomegaly, intoxication, infectious and vegetative-visceral syndromes (Table 2). The combination of inosine pranobex (Isoprinosine) with recombinant IFN α-2β (Viferon) contributed to more significant dynamics of clinical parameters. The number of ARI episodes decreased from 6–11 (7.9 ± 1.1) to 4–6 (5.2 ± 1.2) per year during monotherapy with recombinant IFN α-2β (Viferon), and to 2–4 ( 2.5 ± 1.4) per year during combination therapy (p < 0.05). In both groups, the frequency of EBV replication decreased, but with the combined use of antiviral drugs, this effect was more pronounced.
The use of a combination of inosine pranobex (Isoprinosine) and recombinant IFN α-2β (Viferon) in patients with CEBVI led to more pronounced positive dynamics of immune status indicators (decrease in IL-1RA content, normalization of the expression of activation markers of immunocompetent cells (HLA-DR) and apoptosis receptors ( CD95); increased functional activity of Th1 (increased IFN-γ), restoration of the number of T-lymphocytes and NK-cells, higher content of CD8-lymphocytes than with monotherapy. There was no complete normalization of the expression of the receptor for IL-2 (CD25). during combination antiviral therapy, the functional activity of Th2 decreased (normalization of IL-4 levels). The number of B cells at the end of treatment was normal. An increase in the level of IgA and a switch in Ab synthesis from the IgM class to IgG were recorded; the content of CEC decreased. Indicators of neutrophil metabolism improved The content of neutrophil chemotactic factor (IL-8) did not reach the norm, but was higher than with Viferon monotherapy.
There were no side effects when using inosine pranobex (Isoprinosine) and recombinant IFN α-2β (Viferon).
The results of the study indicate potentiation of the effects of the combination of inosine pranobex (Isoprinosine) with recombinant IFN a-2b (Viferon) in patients with EBVI.
Potentiation of the antiviral, immunomodulatory and cytoprotective effects of these drugs leads to more significant positive dynamics in the manifestations of clinical symptoms of EBVI than with monotherapy, and to the disappearance of serological markers of the activity of the infectious process. It should be noted the high efficiency and safety of combination therapy using inosine pranobex (Isoprinosine) and recombinant IFN α-2β (Viferon).
Rehabilitation. The child is observed by a local doctor and an infectious disease specialist, and is removed from the register 6–12 months after the disappearance of clinical and laboratory indicators of the activity of the infectious process. The frequency of inspections is 1 time per month. According to indications, a consultation with an ENT doctor, immunologist, hematologist, oncologist, etc. is recommended. Laboratory and instrumental studies of patients include: clinical blood test once a month for 3 months, then once every 3 months, more often if indicated; serological markers of EBV using ELISA once every three months, more often if indicated; PCR of blood, oropharyngeal smears once every 3 months, more often if indicated; immunogram - once every 3–6 months; biochemical and instrumental studies - according to indications.
Rehabilitation therapy includes: protective regime, nutritional therapy, antiviral drugs according to prolonged regimens. Under the control of the immunogram, immunocorrection is carried out. According to indications, local antibacterial drugs, courses of vitamin-mineral complexes, pro- and prebiotics, metabolic rehabilitation drugs, enterosorbents, antihistamines, hepato-, neuro- and angioprotectors, cardiotropic drugs, enzymes, homeopathic remedies, and non-drug treatment methods are prescribed.
Thus, EBVI is characterized by a wide distribution, a long course with periodic reactivation of the infectious process in some patients, the possibility of developing complications and adverse outcomes (oncological diseases, autoimmune pathology). The formation of secondary IDS plays an important role in EBVI. The leading clinical syndromes of EBVI are acute and chronic mononucleosis-like syndromes, intoxication, infectious, cerebral, gastrointestinal, cardiac and arthralgic syndromes. Diagnosis of EBVI is based on analysis of risk groups, identification of leading clinical syndromes and laboratory testing. Treatment of EBVI is complex and includes etiotropic drugs (virostatic drugs, interferon and its inducers), drugs for pathogenetic, immunomodulatory, and symptomatic therapy. The combined prolonged use of inosine pranobex (Isoprinosine) and recombinant IFN α-2β (Viferon), potentiating their immunocorrective and cytoprotective effects, significantly increases the effectiveness of treatment. Patients with EBVI need long-term rehabilitation with mandatory monitoring of clinical and laboratory indicators of the activity of the infectious process.
For questions regarding literature, please contact the editor.
E. N. Simovanyan , Doctor of Medical Sciences, Professor V. B. Denisenko , Candidate of Medical Sciences L. F. Bovtalo , Candidate of Medical Sciences A. V. Grigoryan Rostov State Medical University, Rostov-on-Don
What causes the appearance of atypical lymphocytes?
When a person is sick and his body needs protection, the immune system must produce a sufficient number of lymphocytes so that together they can cope with the aggressor. Unfortunately, sometimes there are not enough immune resources for this. Cells are produced, but cannot fully mature and prepare to meet a pathogen or allergen. So it turns out that the number of such unusual lymphocytes in the blood increases. They perform the necessary functions, but their “appearance” is not very complete.
As soon as the patient gets better, the blood picture immediately, in just a few days, improves.
Sometimes high lymphocytes in the blood and the appearance of atypical forms are observed not only with ARVI and allergies, but also in more serious situations. Whooping cough, syphilis, tuberculosis, lymphocytic leukemia, brucellosis, toxoplasmosis, and serum sickness can lead to the appearance of large numbers of them.
What to do if there are elevated levels of atypical lymphocytes in the blood?
There is only one option: to be treated by taking therapy prescribed by the doctor. This, depending on the nature of the disease, can be a variety of medications and techniques. In addition, in consultation with your doctor, you can take Transfer Factor.
The presence of atypical lymphocytes indicates that the human immune system is working under strain. This tool allows her to help. It is created on the basis of information molecules extracted from cow colostrum and egg yolks. Molecules “train” lymphocytes to function properly, which accelerates their formation, maturation and improves performance. Regular use of the drug helps to quickly restore health and return normal blood counts.
Sore throat or mononucleosis?
Viral mononucleosis is a rare disease, but sometimes it is confused with ordinary sore throat, which is better known. However, the treatment of these diseases is completely different and therefore an incorrect diagnosis can lead to serious complications. How to distinguish one disease from another? What to do if the doctor prescribes antibiotic after antibiotic, but they have no effect?
Viruses and bacteria
First of all, you need to understand a simple thing: viruses and bacteria are inherently different. If a virus is an extracellular life form, which is a simplified parasitic structure that can penetrate a living cell and multiply inside it, then a bacterium is a microscopic organism (usually single-celled) with a cell wall. Viruses create favorable conditions for activating the growth of bacteria, while bacteria do not affect viruses in the same way as antibiotics (antibacterial drugs).