6622 02 December
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. We remind you that independent interpretation of the results is unacceptable; the information below is for reference only.
Beta-2-microglobulin (in blood): indications for use, rules for preparing for the test, interpretation of results and normal indicators.
Indications for prescribing the study
Beta-2 microglobulin (Beta-2 microglobulinserum, BMG) is a protein that is found on the surface of almost all cells in the human body.
The study of beta-2-microglobulin in the blood is prescribed for kidney diseases, for patients on dialysis to assess the risk of developing amyloidosis (deposition of pathological proteins in organs and tissues), to identify early signs of kidney rejection after transplantation. Beta-2-microglobulin is often elevated in the blood in cancers such as multiple myeloma (a tumor of the blood cells (lymphocytes) that destroys bones), lymphoma (a tumor that primarily affects the lymph nodes), and leukemia (blood cancer).
Classification
Depending on the level of damage to the hypothalamic-pituitary system, the following are distinguished:
- hypergonadotropic hypogonadism (primary) in men. Testosterone production by the testicles is reduced or absent. Here we can distinguish congenital forms (Klinefelter syndrome - Fig. 1, anorchidism) and acquired forms (trauma, radiation, chemotherapy, other toxic lesions of the testicles, late initiation of treatment for cryptorchidism);
- hypogonadotropic (secondary) hypogonadism in men. Pituitary hormones that stimulate testosterone secretion are reduced or absent. This group also includes congenital forms (Kalman syndrome, isolated LH deficiency, other rare congenital diseases accompanied by hypogonadism), and acquired forms (tumors of the pituitary gland and hypothalamus, their surgical treatment or radiation therapy, hemorrhages in them, etc.);
- normogonadotropic hypogonadism. This condition is characterized by low testosterone production with normal levels of gonadotropins. It is based on mixed disorders in the reproductive system, expressed not only in primary damage to the testicles, but also in hidden insufficiency of hypothalamic-pituitary regulation. Typical examples are hypogonadism in obese men, hypogonadism with hyperprolactinemia (Fig. 2) and hypothyroidism, age-related hypogonadism (Fig. 3), iatrogenic hypogonadism;
- hypogonadism due to target organ resistance (feminization as a result of tissue receptor resistance to androgens; 5α-reductase deficiency; deficiency of estrogens, which in physiological concentrations are modulators of the normal effects of testosterone).
Figure 1. Example of patients with Klinefelter's sign
Based on the time of occurrence, prepubertal and postpubertal hypogonadism can be distinguished.
Preparation for the procedure
- It is preferable to wait 4 hours after your last meal.
- On the eve of the study, you should avoid food overload (do not eat too much!).
- Avoid drinking alcohol on the eve of the test.
- Do not smoke for at least 1 hour before the test.
- Try not to overexert yourself physically and emotionally on the eve of the test.
- When studying the concentration of beta-2-microglobulin in the blood over time, it is recommended to conduct repeated studies under the same conditions (donate blood in the same laboratory).
Clinical picture
The clinical picture of the disease depends on the time of occurrence of the disorder and is presented in Table 1.
Table 1. Main signs of hypogonadism
There are nonspecific signs that may lead a clinician to suspect hypogonadism:
- oligo- and azoospermia;
- pathological fractures (discrepancy between the strength of the traumatic factor and the severity of the injury);
- osteopenia;
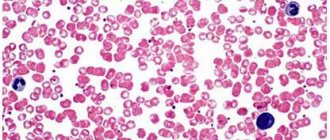
- moderate anemia (normochromic, normocytic);
- increase in adipose tissue;
- depression, sleep disturbance, memory loss.
Reference values:
| Age | Men, mg/l | Women, mg/l |
| 1 day – 4.3 weeks. | 1,6 – 4,8 | 1,7 – 4,5 |
| 4.3 weeks – 6 months | 1,4– 3,3 | 1,0 – 3,8 |
| 6 months – 12 months | 0,9 – 3,1 | 1,0 – 2,3 |
| Over 1 year old | 0,9 – 2,0 | 0,9 – 2,0 |
Beta-2-microglobulin is present on almost all cells of the body and is released into the blood, especially by beta lymphocytes (blood cells that provide immunity, recognize foreign structures, and synthesize antibodies).
In the human body, beta-2-microglobulin performs important functions:
- provides the process of antigenic presentation (presentation) of a foreign agent to trigger an immune response;
- participates in cell proliferation (cell reproduction by division);
- involved in the process of apoptosis (controlled physiological self-destruction of cells);
- regulates the production of hormones and cell growth factors.
Beta-2-microglobulin is used in clinical practice as a tumor marker for patients with blood cancer (when blood cells degenerate into tumor cells and cease to perform their functions).
Blood beta-2-microglobulin concentrations are used to determine the severity and spread of multiple myeloma and lymphoma. A higher level of beta-2-microglobulin in the blood corresponds to a more advanced stage of the oncological process.
Studying the concentration of beta-2-microglobulin in the blood over time allows us to draw conclusions about the effectiveness of treatment:
- an increase in beta-2-microglobulin levels may mean that the cancer is spreading and therapy is not effective;
- a decrease in beta-2-microglobulin levels indicates a good prognosis and effective treatment;
- A decrease and subsequent increase in beta-2-microglobulin levels indicates that the cancer has recurred after treatment.
Beta-2-microglobulin is present in most body fluids, most in the blood, less in the cerebrospinal fluid, and trace amounts in the urine.
In adults, the production of this protein is relatively constant. Beta-2-microglobulin passes through the glomeruli of the kidneys (structures that filter the blood), and then returns to the lower parts (in the kidney tubules). When the glomeruli of the kidneys are damaged, they cannot filter beta-2-microglobulin and its levels in the blood increase. The study of beta-2-microglobulin in patients with kidney disease is prescribed for differential diagnosis in order to determine which parts of the kidney are damaged.
In people with kidney disease who are on dialysis (a procedure to artificially cleanse the blood of toxins and harmful substances), beta-2-microglobulin can form abnormal structures that are deposited in joints and tissues (dialysis-associated amyloidosis). Therefore, for patients who have been on dialysis for more than five years, it is recommended to determine the level of beta-2-microglobulin for early detection of amyloidosis.
Complexes with this research
Female hormones.
Follicular phase Assessment of the hormonal status of a woman in the follicular phase 5,930 R Composition Male anti-aging diagnostics Monitoring of basic indicators in a man aged 40+ 13,300 R Composition
Advanced male anti-aging diagnostics Advanced monitoring of key indicators in men aged 40+ RUR 33,710 Composition
IN OTHER COMPLEXES
- Anti-aging diagnostics. Hormonal balance RUB 6,250
- Male infertility. Extended examination RUB 29,030
- Male hormones RUR 6,180
Reasons for increased levels of beta-2-microglobulin in the blood:
- inflammatory process in the body;
- autoimmune disorders (including systemic lupus erythematosus, Sjogren's syndrome, rheumatoid arthritis), when the immune system mistakenly attacks its own cells;
- blood cancer - multiple myeloma, B-cell chronic lymphocytic leukemia, non-Hodgkin's lymphoma, Hodgkin's disease;
- viral infections (HIV, cytomegalovirus infection, infectious mononucleosis, etc.);
- renal failure;
- kidney transplant rejection;
- in patients on hemodialysis.
What does exceeding the norm indicate?
| Albumin | Dehydration, shock |
| Alpha 1 globulin | Pathologies of functional liver cells, acute and chronic inflammation, neoplasms, third trimester of gestation, trauma (including surgery), androgen therapy |
| Alpha-2 globulin | Inflammatory processes, tissue death, malignant formations, nephrotic syndrome, liver cirrhosis, COCs and estrogen preparations, pregnancy |
| Beta globulin | Pathologies of immunoglobulin secretion, estrogen therapy, anemia caused by iron deficiency, pregnancy, subhepatic jaundice, multiple myeloma |
| Gamma globulin | Chronic liver diseases, chronic infectious and autoimmune diseases, pathologies of lymphoid cells |
Reasons for the decrease in beta-2-microglobulin in the blood over time:
- effective cancer treatment.
Sources:
- Drueke TB, Massy ZA. Beta2-microglobulin. Semin Dial 2009; 22: 378–380.
- ChanghoonYoo, Dok Hyun Yoon, Cheolwon Suh.Serum beta-2 microglobulin in malignant lymphomas: an old but powerful prognostic factor. Blood Res. – 2014.
- Burtis CA, Bruns DE. Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics, seventh edition, 2015; 306 p.
- Corlin D, Heegaard N (2012) β2-Microglobulin Amyloidosis. In: Harris J (eds) Protein Aggregation and Fibrillogenesis in Cerebral and Systemic Amyloid Disease. Subcellular Biochemistry, vol 65. Springer, Dordrecht.
- S. Vincent Rajkumar. Myeloma Today: Disease Definitions and Treatment Advances, Am J Hematol. 2021 Jan; 91(1): 90–100.
Diagnosis of hypogonadism
The diagnosis of hypogonadism in men is established on the basis of anamnesis, clinical picture, confirmed by laboratory and instrumental studies. Recent guidelines recommend that the diagnosis of hypogonadism should be made only in men with symptoms, external manifestations, and clearly reduced serum testosterone levels [2]. However, an analysis of the level of morning total testosterone in serum is recommended as an initial diagnostic test for hypogonadism.
Figure 2-3. Different types of hypogonadism
To calculate the level of free testosterone, you can use the online calculator www.issam.ch/freetesto.htm.
Table 2. Testosterone standards
If necessary, determine the levels of SSSH, FSH, LH, prolactin. High risk factors for developing hypogonadism:
- space-occupying formations of the hypothalamic-pituitary region;
- surgical interventions and/or radiation in the area of the sella turcica;
- long-term use of glucocorticoids, ketoconazole, opioids;
- diabetes mellitus, infertility, osteopenia and osteoporosis.
General population screening is not practical [3].
To identify a group at risk of hypogonadism, specialized questionnaires can be used.
Immunoglobulin is elevated in an adult - reasons
If immunoglobulin E is elevated, what does this mean? Immunoglobulin E may be elevated in the presence of parasitic infestations - ascariasis, intestinal nematode, echinococcosis, hookworm disease, amoebiasis, helminth larval migration syndrome. Immunoglobulin levels are also elevated in patients suffering from allergic bronchopulmonary aspergillosis. Elevated immunoglobulin in the blood is detected in patients with allergic diseases caused by IgE antibodies:
- atopic bronchial asthma;
- allergic rhinitis and sinusitis;
- atopic dermatitis;
- drug and food allergies.
Total immunoglobulin ig E may be elevated due to anaphylaxis, urticaria, and angioedema. High immunoglobulin in patients suffering from immunopathological diseases:
- IgE myeloma;
- periarteritis nodosa;
- hypereosinophilia syndrome;
- hyper-IgE syndrome;
- recurrent pyoderma;
- pemphigus (Neumann's syndrome).
Immunoglobulin may also be exceeded in the case of graft-versus-host disease.